Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (19): 3024-3030.doi: 10.12307/2024.140
Previous Articles Next Articles
Differential effects of hypoxia and oxidative stress on paracrine of mesenchymal stem cells from different sources
Pan Xiaoying1, 2, Xu Yongde3, Liu Zhiqiang4, Xing Xiaowen4, Yang Yong2
- 1Changchun University of Chinese Medicine, Changchun 130117, Jilin Province, China; 2Department of Urology, Affiliated Hospital of Changchun University of Chinese Medicine, Changchun 130021, Jilin Province, China; 3Beijing Friendship Hospital, Capital Medical University, Beijing 100000, China; 4Institute of Military Medicine, Academy of Military Sciences, Beijing 100000, China
-
Received:2023-02-22Accepted:2023-04-14Online:2024-07-08Published:2023-09-26 -
Contact:Yang Yong, Doctoral candidate, Chief physician, Department of Urology, Affiliated Hospital of Changchun University of Chinese Medicine, Changchun 130021, Jilin Province, China Xing Xiaowen, Institute of Military Medicine, Academy of Military Sciences, Beijing 100000, China -
About author:Pan Xiaoying, Attending physician, Changchun University of Chinese Medicine, Changchun 130117, Jilin Province, China; Department of Urology, Affiliated Hospital of Changchun University of Chinese Medicine, Changchun 130021, Jilin Province, China -
Supported by:National Natural Science Foundation of China, No. 8197051689 (to LZQ)
CLC Number:
Cite this article
Pan Xiaoying, Xu Yongde, Liu Zhiqiang, Xing Xiaowen, Yang Yong. Differential effects of hypoxia and oxidative stress on paracrine of mesenchymal stem cells from different sources[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(19): 3024-3030.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
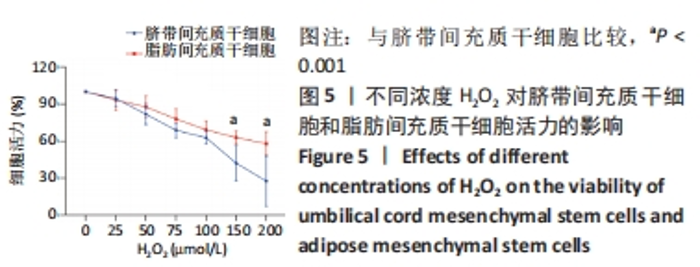
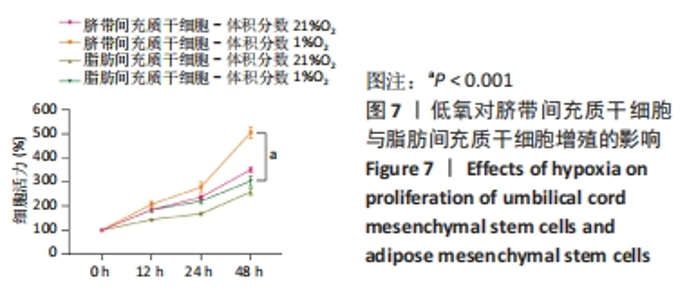
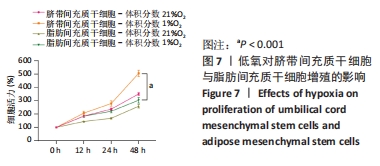
2.5 氧化应激条件对脐带间充质干细胞与脂肪间充质干细胞的影响 2.5.1 不同浓度H2O2对细胞活力的影响 为了比较H2O2对间充质干细胞活力的影响,以不加H2O2的细胞为对照,在细胞内加入不同浓度H2O2处理24 h后,CCK-8检测细胞活力,发现H2O2降低了间充质干细胞活力,见图5。但在≤100 μmol/L中低浓度范围内,H2O2对间充质干细胞活力影响较小;50-100 μmol/L中浓度范围内,2种间充质干细胞活力均高于60%,而且中低浓度时,2种间充质干细胞活力没有明显差异(P > 0.05)。> 100 μmol/L的高浓度H2O2对间充质干细胞毒性较大,尤其是对脐带间充质干细胞毒性较大,200 μmol/L浓度时脐带间充质干细胞活力仅为27%左右。"

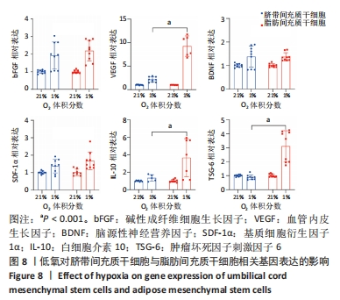
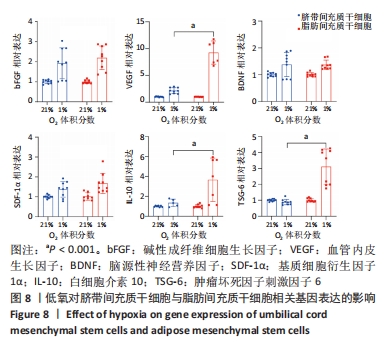
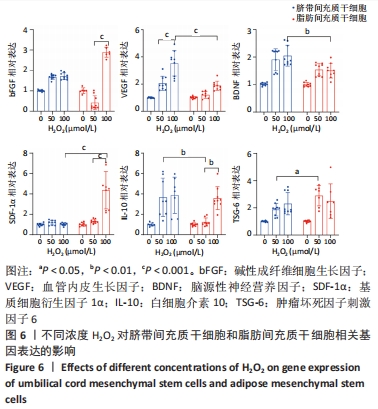
2.5.2 不同浓度H2O2对基因表达的影响 H2O2可以提高间充质干细胞中bFGF、VEGF、BDNF、SDF-1α、IL-10和TSG-6的表达水平,见图6。但H2O2浓度由50 μmol/L升高至100 μmol/L,脐带间充质干细胞中bFGF、BDNF、SDF-1α、IL-10和TSG-6的表达都没有明显变化(P > 0.05),只有VEGF的表达升高(P < 0.001),脂肪间充质干细胞中BDNF、VEGF、TSG-6的表达都没有明显变化(P > 0.05),脂肪间充质干细胞中bFGF、IL-10和SDF-1α的表达升高(P < 0.01)。当H2O2浓度为50 μmol/L时,脐带间充质干细胞中bFGF升高约1.7倍,但脂肪间充质干细胞中bFGF表达降低;而且脐间充质干细胞中IL-10表达升高约4倍,但脂肪间充质干细胞中IL-10表达仅升高约1.3倍。当H2O2浓度为100 μmol/L时,脐带间充质干细胞中bFGF和SDF-1α的表达与50 μmol/L浓度时基本一致,但脂肪间充质干细胞中bFGF升高约3倍,SDF-1α升高4倍多。"
| [1] LI Y, CHEN S, TAN J, et al. Combination therapy with DHA and BMSCs suppressed podocyte injury and attenuated renal fibrosis by modulating the TGF-β1/Smad pathway in MN mice. Ren Fail. 2023;45(1):2120821. [2] CHENG X, MAO GP, HU WJ, et al. Exercise combined with administration of adipose-derived stem cells ameliorates neuropathic pain after spinal cord injury. Neural Regen Res. 2023;18(8):1841-1846. [3] WANG X, ZHAO Y, LI S, et al. Activation of the kynurenine-aryl hydrocarbon receptor axis impairs the chondrogenic and chondroprotective effects of human umbilical cord-derived mesenchymal stromal cells in osteoarthritis rats. Hum Cell. 2023;36(1):163-177. [4] TIAN J, CHEN W, XIONG Y, et al. Small extracellular vesicles derived from hypoxic preconditioned dental pulp stem cells ameliorate inflammatory osteolysis by modulating macrophage polarization and osteoclastogenesis. Bioact Mater. 2022;22:326-342. [5] STEENS J, KLEIN D. HOX genes in stem cells: Maintaining cellular identity and regulation of differentiation. Front Cell Dev Biol. 2022;10:1002909. [6] LEIKER M, SUZUKI G, IYER VS, et al. Assessment of a nuclear affinity labeling method for tracking implanted mesenchymal stem cells. Cell Transplant. 2008; 17(8):911-922. [7] CHEN D, FU W, ZHUANG W, et al. Therapeutic effects of intranigral transplantation of mesenchymal stem cells in rat models of Parkinson’s disease. J Neurosci Res. 2017;95(3):907-917. [8] JOYCE N, ANNETT G, WIRTHLIN L, et al. Mesenchymal stem cells for the treatment of neurodegenerative disease. Regen Med. 2010;5(6):933-946. [9] YAO H, YUAN X, WU Z, et al. Fabrication and Performance Evaluation of Gelatin/Sodium Alginate Hydrogel-Based Macrophage and MSC Cell-Encapsulated Paracrine System with Potential Application in Wound Healing. Int J Mol Sci. 2023;24(2):1240. [10] PITTENGER MF, DISCHER DE, PÉAULT BM, et al. Mesenchymal stem cell perspective: cell biology to clinical progress. NPJ Regen Med. 2019;4:22. [11] TERATANI T, KASAHARA N, FUJIMOTO Y, et al. Mesenchymal Stem Cells Secretions Enhanced ATP Generation on Isolated Islets during Transplantation. Islets. 2022; 14(1):69-81. [12] VATSA P, NEGI R, ANSARI UA, et al. Insights of Extracellular Vesicles of Mesenchymal Stem Cells: a Prospective Cell-Free Regenerative Medicine for Neurodegenerative Disorders. Mol Neurobiol. 2022;59(1):459-474. [13] XU L, ZHANG F, CHENG G, et al. Attenuation of experimental osteoarthritis with human adipose-derived mesenchymal stem cell therapy: inhibition of the pyroptosis in chondrocytes. Inflamm Res. 2023;72(1):89-105. [14] XIAO X, LI W, XU Z, et al. Extracellular vesicles from human umbilical cord mesenchymal stem cells reduce lipopolysaccharide-induced spinal cord injury neuronal apoptosis by mediating miR-29b-3p/PTEN. Connect Tissue Res. 2022; 63(6):634-649. [15] LIN J, ZHU Q, HUANG J, et al. Hypoxia Promotes Vascular Smooth Muscle Cell (VSMC) Differentiation of Adipose-Derived Stem Cell (ADSC) by Regulating Mettl3 and Paracrine Factors. Stem Cells Int. 2020;2020:2830565. [16] WANG L, YAO S, HUANG F, et al. The UCMSC-bFGF/Scaffold System Accelerates the Healing of the Uterine Full-Thickness Injury. Tissue Eng Part A. 2023;29(3-4): 112-125. [17] VOLAREVIC V, GAZDIC M, SIMOVIC MARKOVIC B, et al. Mesenchymal stem cell-derived factors: Immuno-modulatory effects and therapeutic potential. Biofactors. 2017;43(5):633-644. [18] SU Y, XU C, CHENG W, et al. Pretreated Mesenchymal Stem Cells and Their Secretome: Enhanced Immunotherapeutic Strategies. Int J Mol Sci. 2023;24(2): 1277. [19] ISLAMI M, SOLEIMANIFAR F. A Review of Evaluating Hematopoietic Stem Cells Derived from Umbilical Cord Blood’s Expansion and Homing. Curr Stem Cell Res Ther. 2020;15(3):250-262. [20] SANGEETHA KN, VENNILA R, SECUNDA R, et al. Functional variations between Mesenchymal Stem Cells of different tissue origins: A comparative gene expression profiling. Biotechnol Lett. 2020;42(7):1287-1304. [21] SAGARADZE GD, BASALOVA NA, EFIMENKO AY, et al. Mesenchymal Stromal Cells as Critical Contributors to Tissue Regeneration. Front Cell Dev Biol. 2020;8: 576176. [22] HU X, WU R, SHEHADEH LA, et al. Severe hypoxia exerts parallel and cell-specific regulation of gene expression and alternative splicing in human mesenchymal stem cells. BMC Genomics. 2014;15:303. [23] XU CM, KARBASIAFSHAR C, BRINCK TEIXEIRA R, et al. Proteomic Assessment of Hypoxia-Pre-Conditioned Human Bone Marrow Mesenchymal Stem Cell-Derived Extracellular Vesicles Demonstrates Promise in the Treatment of Cardiovascular Disease. Int J Mol Sci. 2023;24(2):1674. [24] WANG M, YANG Y, HAN L, et al. Cell mechanical microenvironment for cell volume regulation. J Cell Physiol. 2020;235(5):4070-4081. [25] YANG Y, WANG X, WANG Y, et al. Influence of Cell Spreading Area on the Osteogenic Commitment and Phenotype Maintenance of Mesenchymal Stem Cells. Sci Rep. 2019;9(1):6891. [26] SONG L, TUAN RS. Transdifferentiation potential of human mesenchymal stem cells derived from bone marrow. FASEB J. 2004;18(9):980-982. [27] OJA S, KOMULAINEN P, PENTTILÄ A, et al. Automated image analysis detects aging in clinical-grade mesenchymal stromal cell cultures. Stem Cell Res Ther. 2018;9(1):6. [28] DOMINICI M, LE BLANC K, MUELLER I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315-317. [29] AL-NBAHEEN M, VISHNUBALAJI R, ALI D, et al. Human stromal (mesenchymal) stem cells from bone marrow, adipose tissue and skin exhibit differences in molecular phenotype and differentiation potential. Stem Cell Rev Rep. 2013; 9(1):32-43. [30] ALFONSETTI M, D’ANGELO M, CASTELLI V. Neurotrophic factor-based pharmacological approaches in neurological disorders. Neural Regen Res. 2023; 18(6):1220-1228. [31] YUAN X, BALOG BM, LIN DL, et al. Brain-Derived Neurotrophic Factor Is an Important Therapeutic Factor in Mesenchymal Stem Cell Secretions for Treatment of Traumatic Peripheral Pelvic Injuries. Front Cell Neurosci. 2022;16: 866094. [32] LIU X, ZHANG J, CHENG X, et al. Integrated printed BDNF-stimulated HUCMSCs-derived exosomes/collagen/chitosan biological scaffolds with 3D printing technology promoted the remodelling of neural networks after traumatic brain injury. Regen Biomater. 2022;10:rbac085. [33] WANG J, HU W, FENG Z, et al. BDNF-overexpressing human umbilical cord mesenchymal stem cell-derived motor neurons improve motor function and prolong survival in amyotrophic lateral sclerosis mice. Neurol Res. 2021;43(3): 199-209. [34] HUANG Y, LIAO L, SU H, et al. Psoralen accelerates osteogenic differentiation of human bone marrow mesenchymal stem cells by activating the TGF-β/Smad3 pathway. Exp Ther Med. 2021;22(3):940. [35] ZHANG X, WANG G, WANG W, et al. Bone marrow mesenchymal stem cells paracrine TGF-β1 to mediate the biological activity of osteoblasts in bone repair. Cytokine. 2023;164:156139. [36] TIE Y, TANG F, PENG D, et al. TGF-beta signal transduction: biology, function and therapy for diseases. Mol Biomed. 2022;3(1):45. [37] LIU Y, LIU N, LI X, et al. Ginsenoside Rb1 Modulates the Migration of Bone-Derived Mesenchymal Stem Cells through the SDF-1/CXCR4 Axis and PI3K/Akt Pathway. Dis Markers. 2022;2022:5196682. [38] MA J, LIU N, YI B, et al. Transplanted hUCB-MSCs migrated to the damaged area by SDF-1/CXCR4 signaling to promote functional recovery after traumatic brain injury in rats. Neurol Res. 2015;37(1):50-56. [39] LIAO N, ZHANG D, WU M, et al. Enhancing therapeutic effects and in vivo tracking of adipose tissue-derived mesenchymal stem cells for liver injury using bioorthogonal click chemistry. Nanoscale. 2021;13(3):1813-1822. [40] LU Y, ZHANG W, TIAN Z, et al. The optimal transplantation strategy of umbilical cord mesenchymal stem cells in spinal cord injury: a systematic review and network meta-analysis based on animal studies. Stem Cell Res Ther. 2022;13(1): 441. [41] SHIFA UL HAQ HM, ASHFAQ R, MEHMOOD A, et al. Priming with caffeic acid enhances the potential and survival ability of human adipose-derived stem cells to counteract hypoxia. Regen Ther. 2023;22:115-127. [42] LIU H, XUE W, GE G, et al. Hypoxic preconditioning advances CXCR4 and CXCR7 expression by activating HIF-1α in MSCs. Biochem Biophys Res Commun. 2010; 401(4):509-515. [43] LIU H, LIU S, LI Y, et al. The role of SDF-1-CXCR4/CXCR7 axis in the therapeutic effects of hypoxia-preconditioned mesenchymal stem cells for renal ischemia/reperfusion injury. PLoS One. 2012;7(4):e34608. [44] MERKHAN MM, SHEPHARD MT, FORSYTH NR. Physoxia alters human mesenchymal stem cell secretome. J Tissue Eng. 2021;12:20417314211056132. [45] NITAHARA-KASAHARA Y, KURAOKA M, ODA Y, et al. Enhanced cell survival and therapeutic benefits of IL-10-expressing multipotent mesenchymal stromal cells for muscular dystrophy. Stem Cell Res Ther. 2021;12(1):105. [46] DYER DP, THOMSON JM, HERMANT A, et al. TSG-6 inhibits neutrophil migration via direct interaction with the chemokine CXCL8. J Immunol. 2014;192(5):2177-2185. [47] LIU Y, ZENG R, WANG Y, et al. Mesenchymal stem cells enhance microglia M2 polarization and attenuate neuroinflammation through TSG-6. Brain Res. 2019; 1724:146422. [48] SALEEM U, SABIR S, NIAZI SG, et al. Role of Oxidative Stress and Antioxidant Defense Biomarkers in Neurodegenerative Diseases. Crit Rev Eukaryot Gene Expr. 2020;30(4):311-322. [49] DEMIRCI-ÇEKIÇ S, ÖZKAN G, AVAN AN, et al. Biomarkers of Oxidative Stress and Antioxidant Defense. J Pharm Biomed Anal. 2022;209:114477. [50] MAHMOUDI T, ABDOLMOHAMMADI K, BASHIRI H, et al. Hydrogen Peroxide Preconditioning Promotes Protective Effects of Umbilical Cord Vein Mesenchymal Stem Cells in Experimental Pulmonary Fibrosis. Adv Pharm Bull. 2020;10(1):72-80. [51] RAHIMI B, PANAHI M, SARAYGORD-AFSHARI N, et al. The secretome of mesenchymal stem cells and oxidative stress: challenges and opportunities in cell-free regenerative medicine. Mol Biol Rep. 2021;48(7):5607-5619. [52] REDZA-DUTORDOIR M, AVERILL-BATES DA. Activation of apoptosis signalling pathways by reactive oxygen species. Biochim Biophys Acta. 2016;1863(12): 2977-2992. [53] LI L, MA Q, MOU J, et al. Basic fibroblast growth factor gel preparation induces angiogenesis during wound healing. Int J Artif Organs. 2023;46(3):171-181. [54] DENG J, ZHANG X, YIN M, et al. Modified CFBP-bFGF targeting to ischemic brain promoted the functional recovery of cerebral ischemia. J Control Release. 2023;353:462-474. [55] WANG P, LI J, ZHANG C, et al. bFGF overexpression adipose derived mesenchymal stem cells improved the survival of pulmonary arterial endothelial cells via PI3k/Akt signaling pathway. Int J Biochem Cell Biol. 2019;113:87-94. [56] CALVO PM, HERNÁNDEZ RG, DE LA CRUZ RR, et al. Role of vascular endothelial growth factor as a critical neurotrophic factor for the survival and physiology of motoneurons. Neural Regen Res. 2023;18(8):1691-1696. [57] PARK JS, KIM D, HONG HS. Priming with a Combination of FGF2 and HGF Restores the Impaired Osteogenic Differentiation of Adipose-Derived Stem Cells. Cells. 2022;11(13):2042. [58] XU Z, CAO J, ZHAO Z, et al. A functional extracellular matrix biomaterial enriched with VEGFA and bFGF as vehicle of human umbilical cord mesenchymal stem cells in skin wound healing. Biomed Mater. 2021;17(1). |
| [1] | Yang Yifeng, Ye Nan, Wang Lin, Guo Shuaicheng, Huang Jian. Signaling pathway of dexmedetomidine against ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1464-1469. |
| [2] | Lou Guo, Zhang Yan, Fu Changxi. Role of endothelial nitric oxide synthase in exercise preconditioning-induced improvement of myocardial ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1283-1288. |
| [3] | Qiu Xiaoyan, Li Bixin, Li Jingdi, Fan Chuiqin, Ma Lian, Wang Hongwu. Differentiation of insulin-producing cells from human umbilical cord mesenchymal stem cells infected by MAFA-PDX1 overexpressed lentivirus [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1000-1006. |
| [4] | Liu Qiwei, Zhang Junhui, Yang Yuan, Wang Jinjuan. Role and mechanism of umbilical cord mesenchymal stem cells on polycystic ovary syndrome [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1015-1020. |
| [5] | Pan Xiaolong, Fan Feiyan, Ying Chunmiao, Liu Feixiang, Zhang Yunke. Effect and mechanism of traditional Chinese medicine on inhibiting the aging of mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1091-1098. |
| [6] | Cao Sheng, Kong Lingwei, Xu Kun, Sun Zhijie. Effect of gelatin methacryloyl hydrogel loaded with salvianolic acid B on intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 380-386. |
| [7] | Zheng Jianbin, Lu Yuchun, Jiang Zixian, Li Xiufang, Wang Tao, Wang Wenjing. Yi medicine Sambucus adnata Wall methanol extract in a rat osteoarthritis model: therapeutic effect and target prediction [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3627-3635. |
| [8] | Ma Wanli, Yang Hongsheng, Qu Bo, Zhang Zhengdong, Gong Kai, Lin Yanshui. Mechanisms by which baicalein protects against steriod-induced osteonecrosis of the femoral head in rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3661-3668. |
| [9] | Hai Zhen, Ning Zhongping. Protective effect of salidroside on angiotensin II-induced fibrosis in cardiac fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(20): 3137-3142. |
| [10] | Ji Weixiu, Bai Yi, Wang Shuo, Zhao Yungang. Protective effect and mechanism of 3-nitro-N-methyl salicylamide on the skeletal muscle of rats with limb ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(20): 3164-3169. |
| [11] | Zhang Jiahao, Liu Yuhao, Zhou Chi, Mo Liang, Fang Hanjun, Chen Zhenqiu. The pathological progression of steroid-induced osteonecrosis of the femoral head caused by oxidative stress-induced osteoblast ferroptosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(20): 3202-3208. |
| [12] | Sun Yuan, Wang Qingbo, Pi Yihua, Lu Chunmin, Xu Chuanyi, Zhang Yan. Effects of early and late aerobic exercise on right heart failure induced by monocrotaline in rats with pulmonary hypertension [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 177-185. |
| [13] | Chen Simin, Hu Yingjun, Yan Wenrui, Ji Le, Shao Mengli, Sun Ze, Zheng Hongxing, Qi Shanshan. Establishment and evaluation of a streptozotocin-induced diabetic encephalopathy rat model [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 237-241. |
| [14] | Wu Yaru, Mi Yan, Wei Kaiyue, Gao Heping, Zhang Dingyu, Wang Caili. Regulatory effect of human umbilical cord mesenchymal stem cells on intestinal barrier function in diabetic nephropathy rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(19): 2967-2973. |
| [15] | Xie Ting, Liu Tingting, Zeng Xuehui, Li Yamin, Zhou Panghu, Yi Nianhua. Vitamin D3 attenuates high-glucose exposure-induced oxidative stress to promote osteogenic differentiation of human umbilical cord mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(19): 2981-2987. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||