Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (3): 404-410.doi: 10.12307/2023.888
Previous Articles Next Articles
Leukocyte- and platelet-rich fibrin with autologous hamstring tendon for traumatic patella dislocation
Wang Xinmin, Yan Wenkai, Song Yahui, Liu Fei
- Orthopedics and Arthroscopic Ward Two, First Hospital of Qinhuangdao, Qinhuangdao 066000, Hebei Province, China
-
Received:2022-10-26Accepted:2023-01-05Online:2024-01-28Published:2023-07-10 -
Contact:Liu Fei, Professor, Master’s supervisor, Orthopedics and Arthroscopic Ward Two, First Hospital of Qinhuangdao, Qinhuangdao 066000, Hebei Province, China -
About author:Wang Xinmin, MD, Associate chief physician, Orthopedics and Arthroscopic Ward Two, First Hospital of Qinhuangdao, Qinhuangdao 066000, Hebei Province, China
CLC Number:
Cite this article
Wang Xinmin, Yan Wenkai, Song Yahui, Liu Fei. Leukocyte- and platelet-rich fibrin with autologous hamstring tendon for traumatic patella dislocation[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 404-410.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
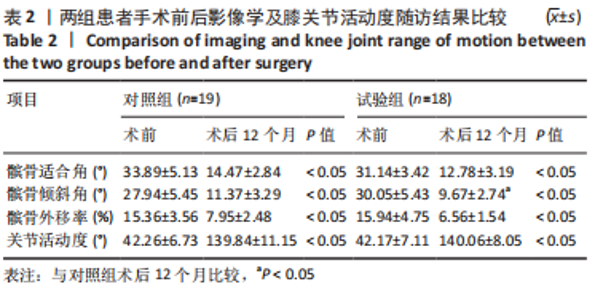
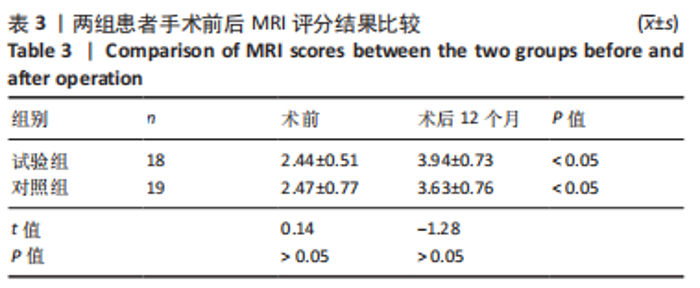
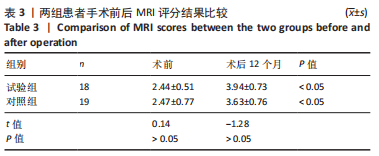
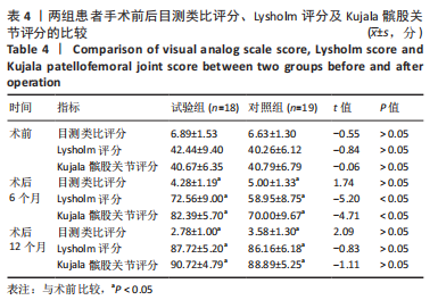
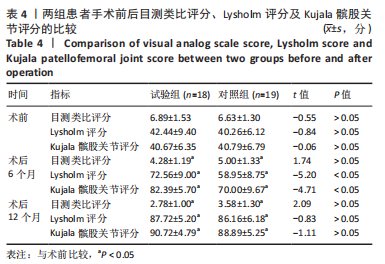
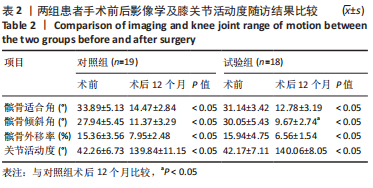
2.4 两组术中情况及不良事件 对照组合并髌骨内缘或股骨外髁软骨撕脱骨折患者3例,由于骨折块直径均< 1 cm,均在膝关节镜下给予取出,3例合并外侧半月板损伤(Ⅲ级),1例给予关节镜下半月板缝合器(Smith Nephew360)全内缝合,其余2例给予部分切除+成形。试验组合并软骨撕脱骨折患者2例,均在膝关节镜下给予取出,4例合并半月板损伤(内侧+外侧),均在膝关节镜下给予部分切除、成形处理。 随访期间两组患者均未出现切口愈合不良、深静脉血栓、锚钉松动、膝关节粘连或僵硬、过敏反应及髌骨再脱位等并发症。对照组1例患者由于体质量指数达到30.2 kg/m2,术后6个月膝关节主动屈曲< 100°,被动屈曲达到120°,静脉麻醉下给予手法屈曲松解,术中被动屈曲达到150°,后于康复科经过手法及CPM机康复锻炼,末次随访时膝关节主动屈曲达到130°,最终成功入组。 2.5 两组患者影像学检查与膝关节活动度比较 两组术后12个月的髌骨倾斜角、适合角及髌骨外移率及膝关节活动度均较术前显著改善(P < 0.05);术后12个月,试验组髌骨倾斜角小于对照组(P < 0.05),两组间髌骨适合角、髌骨外移率及膝关节活动度比较差异无显著性意义(P > 0.05),见表2。"
| [1] LEE BJ, CHRISTINO MA, DANIELS AH, et al. Adolescent patellar osteochondral fracture following patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1856-1861. [2] GURUSAMY P, PEDOWITZ JM, CARROLL AN, et al. Medial Patellofemoral Ligament Reconstruction for Adolescents With Acute First-Time Patellar Dislocation With an Associated Loose Body. Am J Sports Med. 2021;49(8):2159-2164. [3] JAQUITH BP, PARIKH SN. Predictors of Recurrent Patellar Instability in Children and Adolescents After First-time Dislocation. J Pediatr Orthop. 2017;37(7):484-490. [4] IBRAHIM SA, SHOHDY EM, RAMADAN SA, et al. Medial Patellofemoral Ligament Reconstruction in Traumatic Patellar Dislocation without Patellar Fixation. J Knee Surg. 2020;33(10):998-1003. [5] NWACHUKWU BU, SO C, SCHAIRER WW, et al. Surgical versus conservative management of acute patellar dislocation in children and adolescents: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):760-767. [6] LIND M, ENDERLEIN D, NIELSEN T, et al. Clinical outcome after reconstruction of the medial patellofemoral ligament in paediatric patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):666-671. [7] PARK MJ, LEE MC, SEONG SC. A comparative study of the healing of tendon autograft and tendon-bone autograft using patellar tendon in rabbits. Int Orthop. 2001;25(1):35-39. [8] SOON MY, HASSAN A, HUI JH, et al. An analysis of soft tissue allograft anterior cruciate ligament reconstruction in a rabbit model: a short-term study of the use of mesenchymal stem cells to enhance tendon osteointegration. Am J Sports Med. 2007;35(6):962-971. [9] ROTHRAUFF BB, TUAN RS. Cellular therapy in bone-tendon interface regeneration. Organogenesis. 2014;10(1):13-28. [10] MIRON RJ, FUJIOKA-KOBAYASHI M, BISHARA M, et al. Platelet-Rich Fibrin and Soft Tissue Wound Healing: A Systematic Review. Tissue Eng Part B Rev. 2017;23(1):83-99. [11] MASUKI H, OKUDERA T, WATANEBE T, et al. Growth factor and pro-inflammatory cytokine contents in platelet-rich plasma (PRP), plasma rich in growth factors (PRGF), advanced platelet-rich fibrin (A-PRF), and concentrated growth factors (CGF). Int J Implant Dent. 2016;2(1):19. [12] MIJIRITSKY E, ASSAF HD, PELEG O, et al. Use of PRP, PRF and CGF in Periodontal Regeneration and Facial Rejuvenation-A Narrative Review. Biology (Basel). 2021; 10(4).317-340. [13] LANDESBERG R, ROY M, GLICKMAN RS. Quantification of growth factor evels using a simplified method of platelet-rich plasma gel preparation. J Oral Maxillofac Surg. 2000;58(3):297-300,300-301. [14] WEBER-SPICKSCHEN TS, SPANG J, KOHN L, et al. The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: an MRI evaluation. Knee. 2011;18(3).185-188. [15] FIGUEROA D, MELEAN P, CALVO R, et al. Magnetic resonance imaging evaluation of the integration and maturation of semitendinosus-gracilis graft in anterior cruciate ligament reconstruction using autologous platelet concentrate. Arthroscopy. 2010;26(10):1318-1325. [16] DEL TM, ENEA D, PANFOLI N, et al. Hamstrings anterior cruciate ligament reconstruction with and without platelet rich fibrin matrix. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3614-3622. [17] ZHANG Z, ZHANG H, SONG G, et al. A High-Grade J Sign Is More Likely to Yield Higher Postoperative Patellar Laxity and Residual Maltracking in Patients With Recurrent Patellar Dislocation Treated With Derotational Distal Femoral Osteotomy. Am J Sports Med. 2020;48(1):117-127. [18] MULLIEZ A, LAMBRECHT D, VERBRUGGEN D, et al. Clinical outcome in MPFL reconstruction with and without tuberositas transposition. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2708-2714. [19] DONG S, XIE G, ZHANG Y, et al. Ligamentization of Autogenous Hamstring Grafts After Anterior Cruciate Ligament Reconstruction: Midterm Versus Long-term Results. Am J Sports Med. 2015;43(8):1908-1917. [20] BENJAMIN M, KUMAI T, MILZ S, et al. The skeletal attachment of tendons--tendon “entheses”. Comp Biochem Physiol A Mol Integr Physiol. 2002;133(4):931-945. [21] BI F, SHI Z, JIANG S, et al. Intermittently administered parathyroid hormone [1-34] promotes tendon-bone healing in a rat model. Int J Mol Sci. 2014;15(10):17366-17379. [22] SAPPEY-MARINIER E, SONNERY-COTTET B, O’LOUGHLIN P, et al. Clinical Outcomes and Predictive Factors for Failure With Isolated MPFL Reconstruction for Recurrent Patellar Instability: A Series of 211 Reconstructions With a Minimum Follow-up of 3 Years. Am J Sports Med. 2019;47(6):1323-1330. [23] GUO R, GAO L, XU B. Current Evidence of Adult Stem Cells to Enhance Anterior Cruciate Ligament Treatment: A Systematic Review of Animal Trials. Arthroscopy. 2018;34(1):331-340. [24] HEXTER AT, KARALI A, KAO A, et al. Effect of Demineralized Bone Matrix, Bone Marrow Mesenchymal Stromal Cells, and Platelet-Rich Plasma on Bone Tunnel Healing After Anterior Cruciate Ligament Reconstruction: A Comparative Micro-Computed Tomography Study in a Tendon Allograft Sheep Model. Orthop J Sports Med. 2021;9(9):941639222. [25] MAYR R, SMEKAL V, KOIDL C, et al. Tunnel widening after ACL reconstruction with aperture screw fixation or all-inside reconstruction with suspensory cortical button fixation: Volumetric measurements on CT and MRI scans. Knee. 2017;24(5):1047-1054. [26] ALVES R, GRIMALT R. A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification. Skin Appendage Disord. 2018;4(1):18-24. [27] YOU JS, KIM SG, OH JS, et al. Effects of Platelet-Derived Material (Platelet-Rich Fibrin) on Bone Regeneration. Implant Dent. 2019;28(3):244-255. [28] 张松,张涛,付桂红,等.自体富血小板血浆联合骨髓间充质干细胞治疗长骨干骨折术后骨不连[J]. 中国组织工程研究,2017,21(29):4716-4721. [29] KANAZAWA T, SOEJIMA T, NOGUCHI K, et al. Tendon-to-bone healing using autologous bone marrow-derived mesenchymal stem cells in ACL reconstruction without a tibial bone tunnel-A histological study-. Muscles Ligaments Tendons J. 2014;4(2):201-206. [30] QIAO J, AN N, OUYANG X. Quantification of growth factors in different platelet concentrates. Platelets. 2017;28(8):774-778. [31] KANNO T, TAKAHASHI T, TSUJISAWA T, et al. Platelet-rich plasma enhances human osteoblast-like cell proliferation and differentiation. J Oral Maxillofac Surg. 2005; 63(3):362-369. [32] MASUKI H, OKUDERA T, WATANEBE T, et al. Growth factor and pro-inflammatory cytokine contents in platelet-rich plasma (PRP), plasma rich in growth factors (PRGF), advanced platelet-rich fibrin (A-PRF), and concentrated growth factors (CGF). Int J Implant Dent. 2016;2(1):19. [33] TAKAHASHI A, TSUJINO T, YAMAGUCHI S, et al. Distribution of platelets, transforming growth factor-β1, platelet-derived growth factor-BB, vascular endothelial growth factor and matrix metalloprotease-9 in advanced platelet-rich fibrin and concentrated growth factor matrices. J Investig Clin Dent. 2019;10(4):e12458. [34] BIERCEVICZ AM, AKELMAN MR, FADALE PD, et al. MRI volume and signal intensity of ACL graft predict clinical, functional, and patient-oriented outcome measures after ACL reconstruction. Am J Sports Med. 2015;43(3):693-699. [35] STARANTZIS KA, MASTROKALOS D, KOULALIS D, et al. The Potentially Positive Role of PRPs in Preventing Femoral Tunnel Widening in ACL Reconstruction Surgery Using Hamstrings: A Clinical Study in 51 Patients. J Sports Med (Hindawi Publ Corp). 2014;2014:789317. [36] SILVA A, SAMPAIO R. Anatomic ACL reconstruction: does the platelet-rich plasma accelerate tendon healing? Knee Surg Sports Traumatol Arthrosc. 2009;17(6):676-682. [37] HONG S, CHEN W, JIANG B. A Comparative Evaluation of Concentrated Growth Factor and Platelet-rich Fibrin on the Proliferation, Migration, and Differentiation of Human Stem Cells of the Apical Papilla. J Endod. 2018;44(6):977-983. [38] DRAGOO JL, BRAUN HJ, DURHAM JL, et al. Comparison of the acute inflammatory response of two commercial platelet-rich plasma systems in healthy rabbit tendons. Am J Sports Med. 2012;40(6):1274-1281. [39] HU Y, JIANG Y, WANG M, et al. Concentrated Growth Factor Enhanced Fat Graft Survival: A Comparative Study. Dermatol Surg. 2018;44(7):976-984. [40] VENTURA A, TERZAGHI C, BORGO E, et al. Use of growth factors in ACL surgery: preliminary study. J Orthop Traumatol. 2005;6(2):76-79. [41] KIM TH, KIM SH, SÁNDOR GK, et al. Comparison of platelet-rich plasma (PRP), platelet-rich fibrin (PRF), and concentrated growth factor (CGF) in rabbit-skull defect healing. Arch Oral Biol. 2014;59(5):550-558. [42] LIOU JJ, ROTHRAUFF BB, ALEXANDER PG, et al. Effect of Platelet-Rich Plasma on Chondrogenic Differentiation of Adipose- and Bone Marrow-Derived Mesenchymal Stem Cells. Tissue Eng Part A. 2018;24(19-20):1432-1443. |
| [1] | Gu Mingxi, Wang Changcheng, Tian Fengde, An Ning, Hao Ruihu, Guo Lin. Preparation and in vitro evaluation of a three-dimensional porous cartilage scaffold made of silk fibroin/gelatin/chitosan [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 366-372. |
| [2] | Bi Yujie, Ma Dujun, Peng Liping, Zhou Ziqiong, Zhao Jing, Zhu Houjun, Zhong Qiuhui, Yang Yuxin. Strategy and significance of Chinese medicine combined with medical hydrogel for disease treatment [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 419-425. |
| [3] | Wang Xinyi, Xie Xianrui, Chen Yujie, Wang Xiaoyu, Xu Xiaoqing, Shen Yihong, Mo Xiumei. Electrospun nanofiber scaffolds for soft and hard tissue regeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 426-432. |
| [4] | Gao Xueyu, Zhang Wentao, Sun Tianze, Zhang Jing, Li Zhonghai. Application of metal ions in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 439-444. |
| [5] | Yang Jie, Hu Haolei, Li Shuo, Yue Wei, Xu Tao, Li Yi. Application of bio-inks for 3D printing in tissue repair and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 445-451. |
| [6] | Chen Pinrui, Pei Xibo, Xue Yiyuan. Function and advantages of magnetically responsive hydrogel in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 452-457. |
| [7] | Long Zhirui, Huang Lei, Xiao Fang, Wang Lin, Wang Xiaobei. Characteristics of hydrogel microspheres in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 472-478. |
| [8] | Kong Xiangyu, Wang Xing, Pei Zhiwei, Chang Jiale, Li Siqin, Hao Ting, He Wanxiong, Zhang Baoxin, Jia Yanfei. Biological scaffold materials and printing technology for repairing bone defects [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 479-485. |
| [9] | Xu Jing, Lyu Huixin, Bao Xin, Zhang Yi, Wang Yihan, Zhou Yanmin. Application of near infrared responsive hydrogels in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 486-492. |
| [10] | Fan Yongjing, Wang Shu, Jin Wulong. Characteristics, advantages and application of osteogenic differentiation of jaw bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 100-106. |
| [11] | Sun Kexin, Zeng Jinshi, Li Jia, Jiang Haiyue, Liu Xia. Mechanical stimulation enhances matrix formation of three-dimensional bioprinted cartilage constructs [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(在线): 1-7. |
| [12] | Xu Xingxing, Wen Chaoju, Meng Maohua, Wang Qinying, Chen Jingqiao, Dong Qiang. Carbon nanomaterials in oral implant [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1062-1070. |
| [13] | Yang Yitian, Wang Lu, Yao Wei, Zhao Bin. Application of the interaction between biological scaffolds and macrophages in bone regeneration [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1071-1079. |
| [14] | Li Cheng, Zheng Guoshuang, Kuai Xiandong, Yu Weiting. Alginate scaffold in articular cartilage repair [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1080-1088. |
| [15] | Shi Yehong, Wang Cheng, Chen Shijiu. Early thrombosis and prevention of small-diameter blood vessel prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1110-1116. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||