Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (12): 1856-1862.doi: 10.12307/2023.102
Previous Articles Next Articles
Rat bone defect repaired with polytrimethylene carbonate/beta-tricalcium phosphate microsphere scaffold
Huang Yanni1, Yang Hua2, Yang Dongmei1, Hu Xulin3, Gao Hong4, Huang Yina1
- 1West China School of Public Health, Sichuan University/West China Fourth Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China; 2Analysis and Assay Center, West China School of Public Health, Sichuan University, Chengdu 610041, Sichuan Province, China; 3Chengdu Institute of Organic Chemistry, Chinese Academy of Sciences, Chengdu 610041, Sichuan Province, China; 4College of Biomass Science and Engineering, Sichuan University, Chengdu 610065, Sichuan Province, China
-
Received:2021-09-22Accepted:2021-11-11Online:2023-04-28Published:2022-07-30 -
Contact:Huang Yina, Professor, West China School of Public Health, Sichuan University/West China Fourth Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China -
About author:Huang Yanni, Master candidate, West China School of Public Health, Sichuan University/West China Fourth Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
CLC Number:
Cite this article
Huang Yanni, Yang Hua, Yang Dongmei, Hu Xulin, Gao Hong, Huang Yina. Rat bone defect repaired with polytrimethylene carbonate/beta-tricalcium phosphate microsphere scaffold[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1856-1862.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
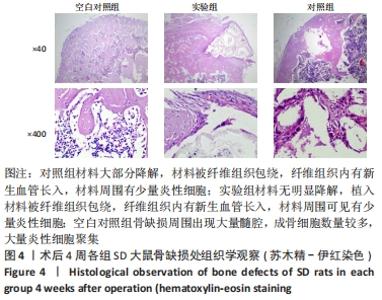
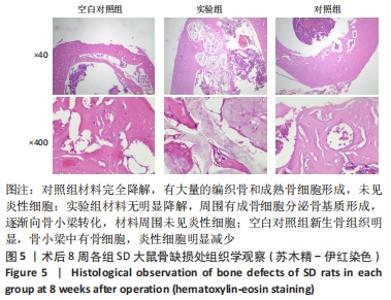
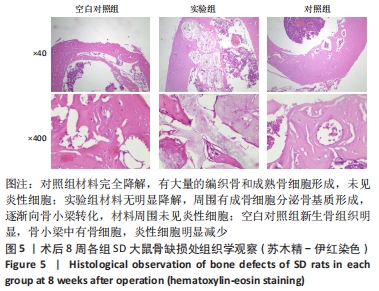
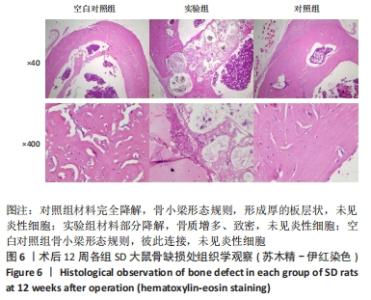
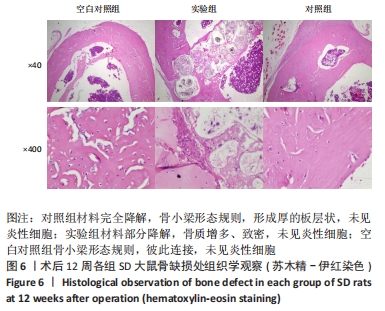
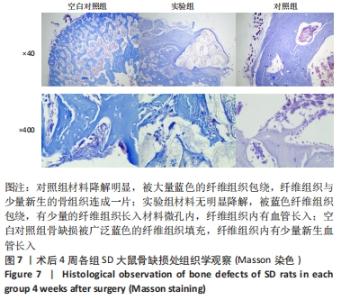
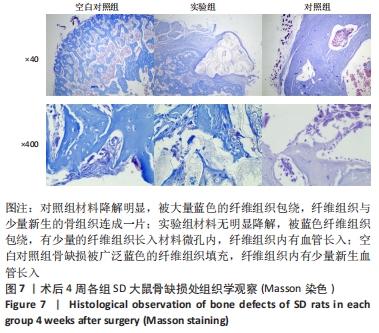
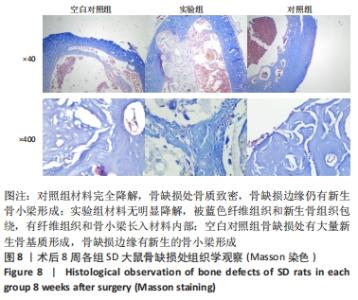
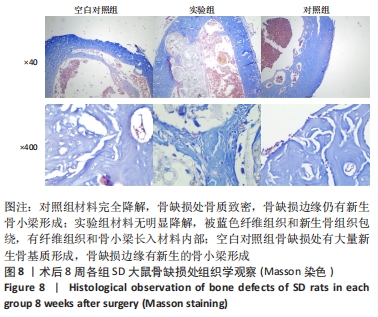
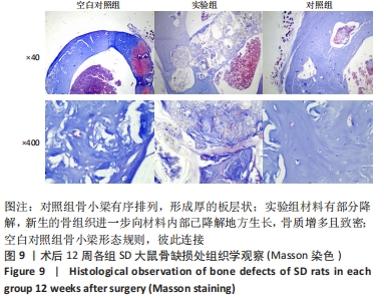
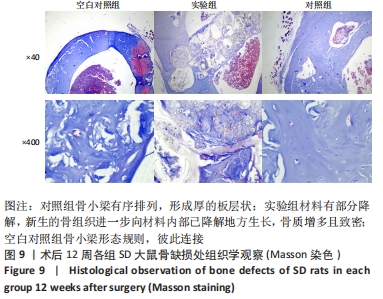
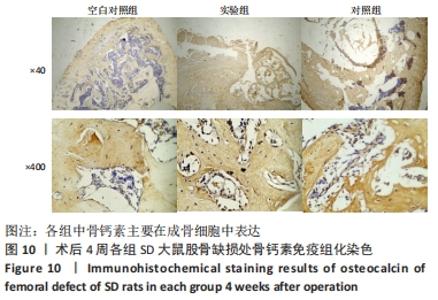
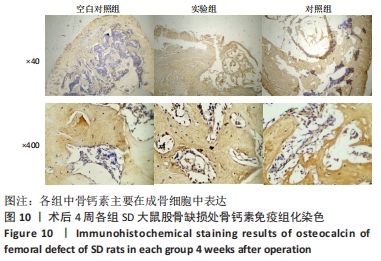
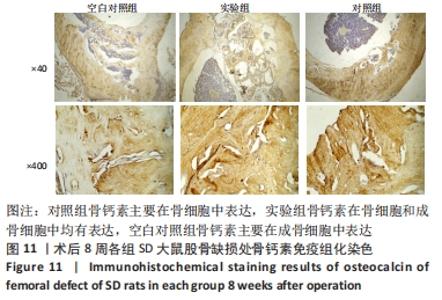
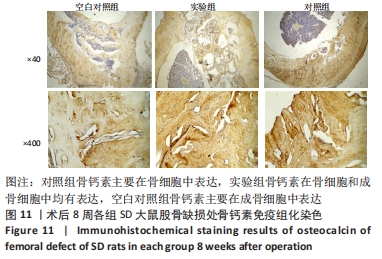
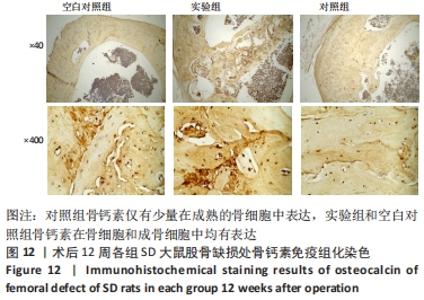
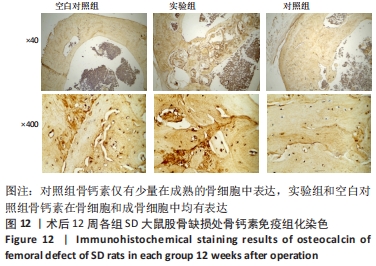
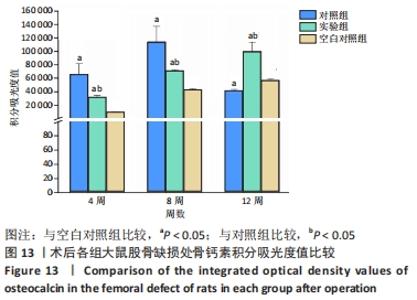
2.2 实验动物数量分析 整个实验过程中无菌操作,合理使用抗生素,术后对大鼠进行了密切观察且其饲养环境良好,没有大鼠死亡,18只大鼠全部进入结果分析。 2.3 动物实验解剖学大体观察结果 对照组植入的β-磷酸三钙骨水泥在术后第4周时已降解吸收,大体观察看不到材料,但可以观察到骨缺损处;术后第8,12周材料β-磷酸三钙骨水泥已完全降解,未观察到骨缺损处。实验组植入的PTMC/β-磷酸三钙微球支架在术后第12周仍可以观察到材料。空白对照组从第4周开始未观察到骨缺损处。 2.4 动物实验股骨组织病理学观察 2.4.1 苏木精-伊红染色 术后4周,对照组材料大部分降解,镜下可见大片空泡,未降解的材料被染成红色,材料被纤维组织包绕,纤维组织内有新生血管长入,骨缺损处有少量新生骨基质、骨小梁形成,材料周围有少量炎性细胞;实验组材料无明显降解,骨缺损处被植入材料填充,植入材料被纤维组织包绕,纤维组织内有新生血管长入,材料周围可见有少量炎性细胞,骨缺损处材料边缘有少量新生骨基质、骨小梁形成;空白对照组骨缺损周围出现大量髓腔,成骨细胞数量较多,出现大量条索状骨小梁,大量炎性细胞聚集,见图4。术后8周,对照组材料完全降解,骨缺损处消失,出现髓腔,有大量的编织骨和成熟骨细胞形成,未见炎性细胞;实验组材料无明显降解,可见骨组织长入材料的微孔内,周围有成骨细胞分泌骨基质形成,逐渐向骨小梁转化,骨小梁上可见成熟的骨细胞,材料周围出现髓腔,材料周围未见炎性细胞;空白对照组先前散在分布的骨小梁连接成网状,新生骨组织明显,骨小梁中有骨细胞,边缘有少量成骨细胞分布,炎性细胞较4周时明显减少,见图5。"
| [1] 刘洋.骨组织工程支架材料研究进展[J].临床口腔医学杂志,2019, 35(10):637-639. [2] 倪建光,刘丹平.骨组织工程支架材料的研究进展[J].中国组织工程研究,2009,13(8):1525-1528. [3] WANG W, YEUNG KWK. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact Mater. 2017;2(4):224-247. [4] CAMPANA V, MILANO G, PAGANO E, et al. Bone substitutes in orthopaedic surgery: from basic science to clinical practice. J Mater Sci Mater Med. 2014;25(10):2445-2461. [5] BUROVA I, WALL I, SHIPLEY RJ. Mathematical and computational models for bone tissue engineering in bioreactor systems. J Tissue Eng. 2019;10:204173141982792. [6] BI L, CHENG W, FAN H, et al. Reconstruction of Goat Tibial Defects Using an Injectable Tricalcium Phosphate/Chitosan in Combination with Autologous Platelet-Rich Plasma. Biomaterials 2010;31(12):3201-3211. [7] BAL Z, KAITO T, KORKUSUZ F, et al. Bone regeneration with hydroxyapatite-based biomaterials. Emergent Mater. 2020;3(4):521-544. [8] REZWAN K, CHEN QZ, BLAKER JJ, et al. Biodegradable and Bioactive Porous Polymer/Inorganic Composite Scaffolds for Bone Tissue Engineering. Biomaterials. 2006;27(18):3413-3431. [9] REN J, BLACKWOOD KA, DOUSTGANI A, et al. Melt-electrospun polycaprolactone strontium substituted bioactive glass scaffolds for bone regeneration. J Biomed Mater Res A. 2014;102(9):3140-3153. [10] LI J, JIN L, WANG M, et al. Repair of rat cranial bone defect by using bone morphogenetic protein-2-related peptide combined with microspheres composed of polylactic acid/polyglycolic acid copolymer and chitosan. Biomed Mater. 2015;10(4):045004. [11] FUKUSHIMA K. Poly(trimethylene carbonate)-based polymers engineered for biodegradable functional biomaterials. Biomater Sci. 2016;4(1):9-24. [12] LIU H, SLAMOVICH EB, WEBSTER TJ. Increased osteoblast functions among nanophase titania/poly(lactide-co-glycolide) composites of the highest nanometer surface roughness. J Biomed Mater Res A. 2006; 78(4):798-807. [13] FIRDAUS SM, SHENG TJ, ARIFFIN Z, et al. Properties improvement of acrylic resin for denture application: effect of single and hybrid types of fillers with different weight loadings. Plast Rubber Compos. 2021;(1): 1-11. [14] PÊGO AP, VAN LUYN MJ, BROUWER LA, et al. In vivo behavior of poly(1,3-trimethylene carbonate) and copolymers of 1,3-trimethylene carbonate with D,L-lactide or Ɛ-caprolactone: Degradation and tissue response. J Biomed Mater Res A. 2003;67(3):1044-1054. [15] RONGEN JJ, VAN BOCHOVE B, HANNINK G, et al. Degradation behavior of, and tissue response to photo-crosslinked poly(trimethylene carbonate) networks. J Biomed Mater Res A. 2016;104(11):2823-2832. [16] PÊGO AP, VLEGGEERT-LANKAMP CL, DEENEN M, et al. Adhesion and growth of humanSchwann cells on trimethylene carbonate (co)polymers. J BiomedMater Res A. 2003;67:876-885. [17] ZENG N, LEEUWEN A, YUAN H, et al. Evaluation of novel resorbable membranes for bone augmentation in a rat model. Clin Oral Implants Res. 2016;27(2):8-14. [18] HE J, ZHANG Y, LIU X, et al. Load-bearing PTMC-beta tri-calcium phosphate and dexamethasone biphasic composite microsphere scaffolds for bone tissue engineering. Mater Lett. 2019; 260:126939. [19] 陈江,陈旭晞,周麟.骨免疫调节机制对种植体骨结合及骨生物材料引导骨再生的影响[J].广东牙病防治,2018,26(10):613-620. [20] CHAN JK, GLASS GE, ERSEK A, et al. Low-dose TNF augments fracture healing in normal and osteoporotic bone by up-regulating the innate immune response. EMBO Mol Med. 2015;7(5):547-561. [21] 罗伟,李翔翮,杨先腾,等.骨折模型小鼠周围组织E、P选择素含量变化及意义[J].中国组织工程研究,2019,23(3):82-86. [22] KIM J, HEMATTI P. Mesenchymal stem cell-educated macrophages: A novel type of alternatively activated macrophages. Exp Hematol. 2009;37(12):1445-1453. [23] BORCHERS A, TEUBER SS, KEEN CL, et al. Clinical Reviews in Allergy and Immunology. Clin Rev Allergy Immunol. 2010;39(2):95-141. [24] KEILIS-BOROK IV, RAEVSKAYA MV, FRIDENSHTEIN AY, et al. Properties of bone tissue induced by transitional epithelium. Biull Eksp Biol Med. 1982;94(12):87-89. [25] LIU H, CAI Q, LIAN P, et al. β-tricalcium phosphate nanoparticles adhered carbon nanofibrous membrane for human osteoblasts cell culture. Mater Lett. 2010;64(6):725-728. [26] GHAYOR C, BHATTACHARYA I, WEBER FE. The optimal microarchitecture of 3D-printed β-TCP bone substitutes for vertical bone augmentation differs from that for osteoconduction. Mater Design. 2021;204(6): 109650. [27] YUAN H. Bone formation induced by calcium phosphate ceramics in soft tissue of dogs: a comparative study between porous α-TCP and β-TCP. J Mater Sci Mater Med.2001;12(1):7-13. [28] TAYEBI M, PARHAM S, AHANGAR HA, et al. Preparation and evaluation of bioactive bilayer composite membrane PHB/β‐TCP with ciprofloxacin and vitamin D3 delivery for regenerative damaged tissue in periodontal disease. J Appl Polym Sci. 2021;139(3):e51507. [29] 刘兆强,朱立国.磷酸钙材料在骨再生中的应用进展[J].中国医疗设备,2019,34(10):158-163. [30] BEREZOVSKA O, YILDIRIM G, BUDELL WC, et al. Osteocalcin affects bone mineral and mechanical properties in female mice. Bone. 2019; 128:115031. [31] AL-RIFAI O, CHOW J, LACOMBE J, et al. Proprotein convertase furin regulates osteocalcin and bone endocrine function. J ClinInvest. 2017; 127(11):4104-4117. [32] HAUSCHKA PV, LIAN JB, GALLOP PM. Direct identification of the calcium-binding amino acid, gamma-carboxyglutamate, in mineralized tissue. Proc Natl Acad Sci U S A. 1975;72(10):3925-3929. [33] PRICE PA, OTSUKA AA, POSER JW, et al. Characterization of a gamma-carboxyglutamic acid-containing protein from bone. Proc Natl Acad Sci U S A. 1976;73(5):1447-1451. [34] HAN X, DU J, DI L, et al. Histochemical examination of systemic administration of eldecalcitol combined with guided bone regeneration for bone defect restoration in rats. J Mol Histol. 2016;48(1):1-11. [35] HE J, HU X, ZHANG Y, et al. A composite polytrimethylene carbonate microsphere-reinforced porous scaffold for osteoblast regeneration. Colloids Surf A Physicochem Eng Asp. 2019;587:124325 |
| [1] | Tang Haotian, Liao Rongdong, Tian Jing. Application and design of piezoelectric materials for bone defect repair [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1117-1125. |
| [2] | Qin Yuxing, Ren Qiangui, Li Zilong, Quan Jiaxing, Shen Peifeng, Sun Tao, Wang Haoyu. Action mechanism and prospect of bone microvascular endothelial cells for treating femoral head necrosis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 955-961. |
| [3] | Zhang Min, Zhang Xiaoming, Liu Tongbin. Application potential of naringin in bone tissue regeneration [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 787-792. |
| [4] | Chen Feng, Ren Guowu, Zhang Xiaoyun, Chen Yueping, Shi Rusheng. Receptor activator of nuclear factor-kappa B ligand signal transduction mechanism and osteoclast activation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(2): 293-299. |
| [5] | Jiang Chengming, Jiang Sainan, Tang Ye, Jiang Lin. Efficacy of 3D printed microporous titanium fusion device applied to anterior cervical decompression graft fusion and its effects on cervical spine anatomy and stress hormones [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2837-2841. |
| [6] | Liang Weiye, Duan Qinghong. Correlation between femur bone morphogenetic protein 2 expression and bone fluoride content in fluorosis rabbits [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(17): 2675-2680. |
| [7] | Wu Boyu, Ye Kai, Chen Jiahan, Wang Jianghua, Wurikaixi·Aiyiti, Jiang Houfeng, Teng Yong. Biocompatibility of 3D printed polyetheretherketone/hydroxyapatite composites [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1932-1937. |
| [8] | Ren Wenyan, Liu Xue, Wang Yiyu. Grophene-family nanomaterials in the treatment of periodontal disease: beneficial for osteogenic differentiation and reconstruction of periodontal support tissues [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1954-1960. |
| [9] | Zhang Zihan, Wang Wenli, Li Jinnuo, Li Yourui. Effects of carvacrol on osteoblasts and common oral pathogens [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(11): 1765-1771. |
| [10] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [11] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [12] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [13] | Le Guoping, Zhang Ming, Xi Licheng, Luo Hanwen. Preparation and in vitro evaluation of vancomycin hydrochloride@polylactic acid-glycolic acid copolymer-chitosan-hyaluronic acid composite sustained-release microspheres [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 528-534. |
| [14] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [15] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||