Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (7): 1141-1148.doi: 10.12307/2023.007
Effects of different dressings in the treatment of burn wounds: a network meta-analysis
Li Wenjie1, You Aijia1, Zhou Junli1, Fang Sujuan2, Li Chun1
- 1School of Nursing, Guangzhou University of Chinese Medicine, Guangzhou 510006, Guangdong Province, China; 2Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510120, Guangdong Province, China
-
Received:2021-11-10Accepted:2021-12-21Online:2023-03-08Published:2022-07-20 -
Contact:Li Chun, Associate professor, School of Nursing, Guangzhou University of Chinese Medicine, Guangzhou 510006, Guangdong Province, China -
About author:Li Wenjie, Master candidate, School of Nursing, Guangzhou University of Chinese Medicine, Guangzhou 510006, Guangdong Province, China -
Supported by:University Characteristic Innovation Project of Guangdong Provincial Department of Education, No. 2020KTSCX025 (to LC)
CLC Number:
Cite this article
Li Wenjie, You Aijia, Zhou Junli, Fang Sujuan, Li Chun. Effects of different dressings in the treatment of burn wounds: a network meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(7): 1141-1148.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
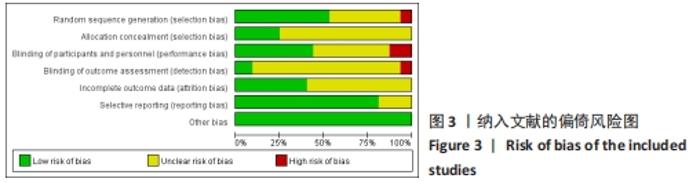
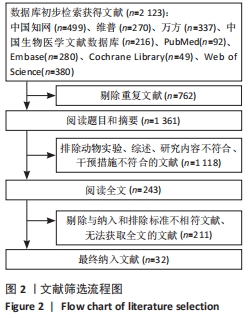
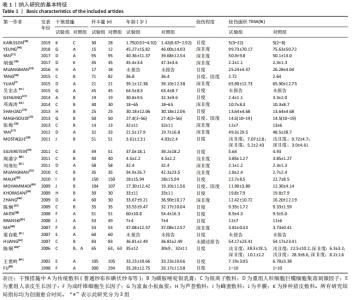
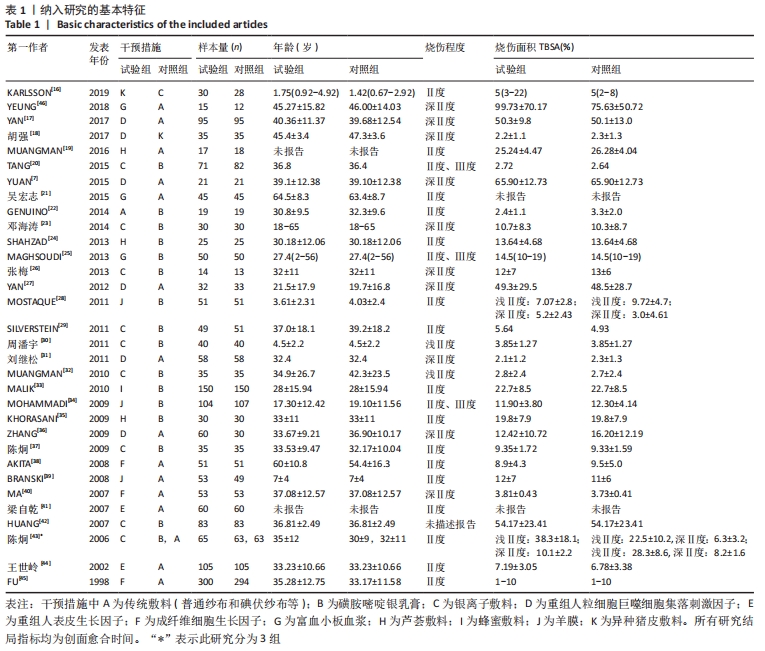
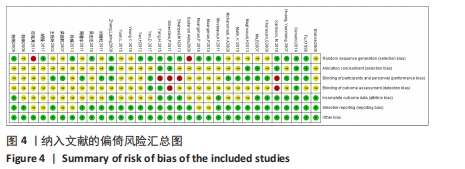
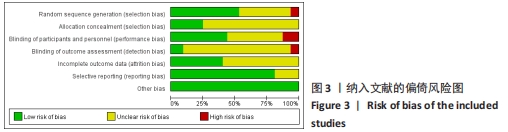
2.3 纳入研究质量评价结果 共纳入32篇文献,均为随机对照试验,所有研究均提及随机分组,其中19项研究报告了随机序列产生的具体方法[16-24,26-29,32,36-38,42,45],主要采用随机数字表法[17-19,21-22,26,28,36-37,42,45]、随机序列法[16,27,42],2项研究按就诊日期或就诊顺序随机[23,38];5项研究报告了分配隐藏的具体方法[16,22,36,40,45];15项研究报告了盲法的使用情况[17,20,22,25,30-31,33-36,40-42,44-45],其中9项研究采用双盲法[25,30-31,33,35-36,40-41,44],纳入研究中有3项研究提出因敷料特殊性或其他原因而无法设置盲法[16,24,29];12项研究报告了试验组和对照组病例具体脱落情况[16,20,22,28-29,35-37,39-40,42,45],对研究结果影响较小,其他研究未提及病例脱落、退出,数据完整。其结果运用RevMan 5.4软件绘制如图3,4。"
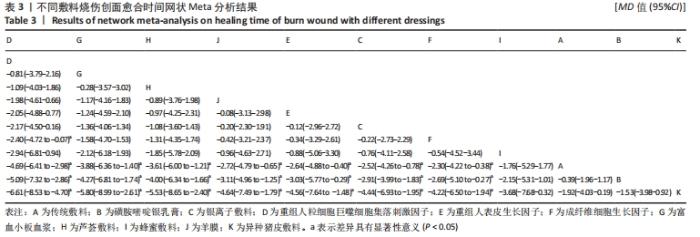
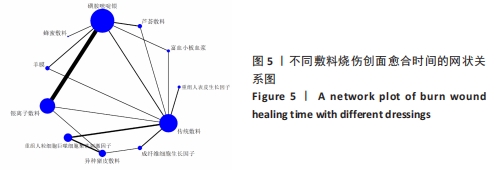
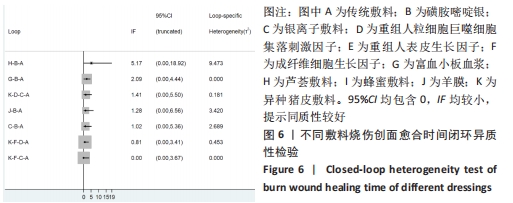
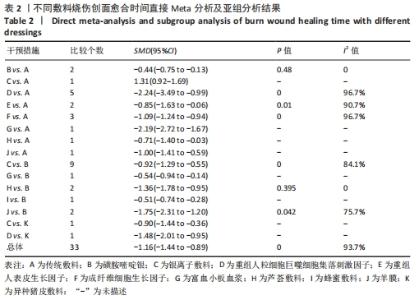
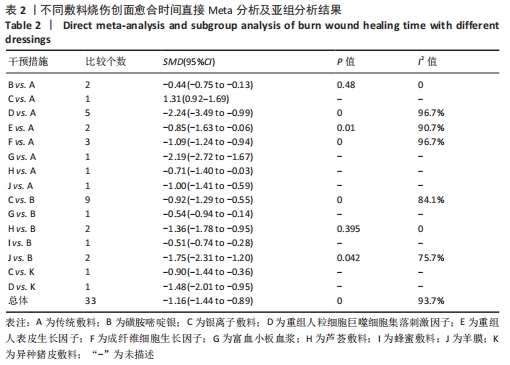
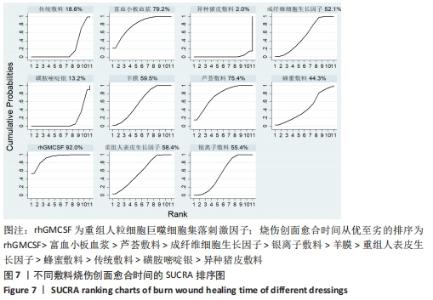
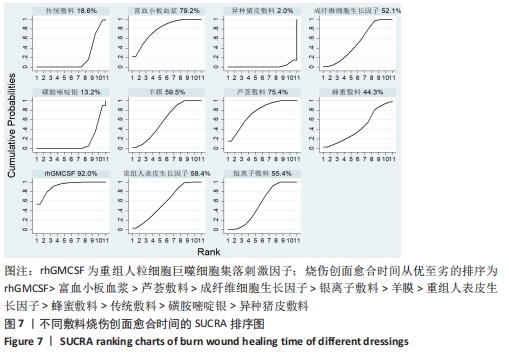
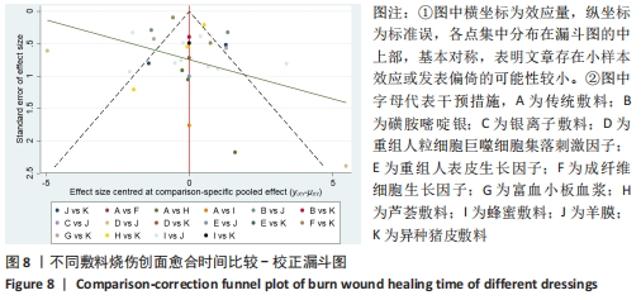
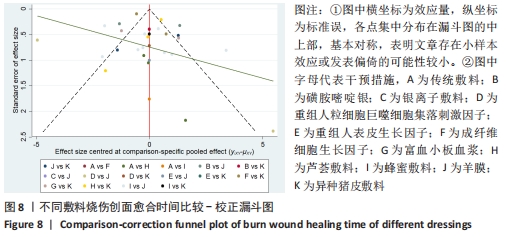
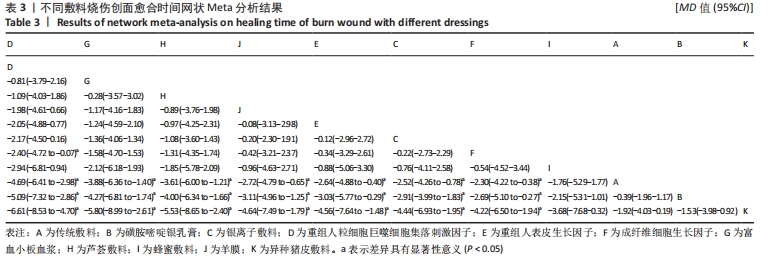
对纳入的31项研究运用不一致性模型进行检验,结果显示:P=0.634,P > 0.05,说明不一致性模型不显著,可以使用一致性模型进行一致性拟合,结果显示:P=0.634,P > 0.05,说明一致性较好。运用节点分裂法(node-splitting method)进行局部不一致性检验,结果显示:P > 0.05,表明各研究间具有一致性,因此在一致性模型下进行网状Meta分析。 2.4.3 不同敷料烧伤创面愈合时间的网状Meta分析结果 纳入的31个随机对照试验[7,16-45],网状Meta分析结果显示:重组人粒细胞巨噬细胞集落刺激因子、富血小板血浆、芦荟敷料、羊膜、重组人表皮生长因子、银离子敷料、成纤维细胞生长因子在缩短烧伤创面愈合时间方面均优于传统敷料、磺胺嘧啶银和异种猪皮敷料(P < 0.05);重组人粒细胞巨噬细胞集落刺激因子在烧伤创面愈合时间上优于成纤维细胞生长因子,差异有显著性意义(P < 0.05);其他干预措施之间比较差异无显著性意义(P > 0.05),见表3。 "
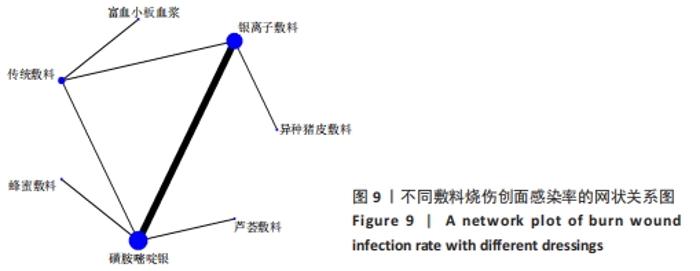
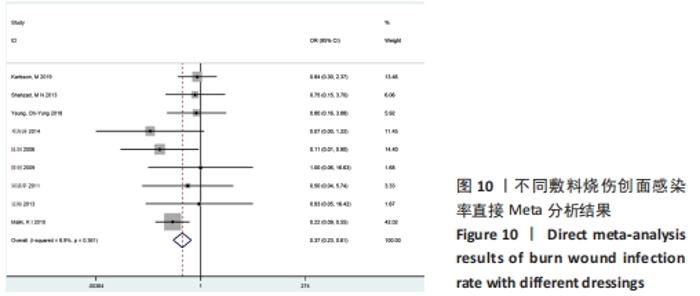
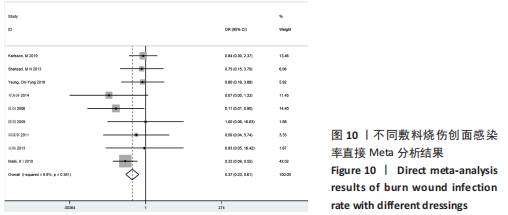
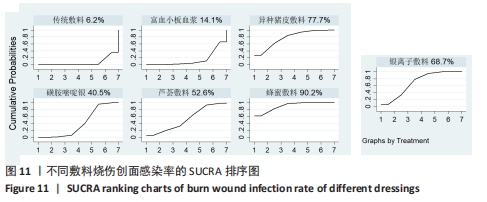
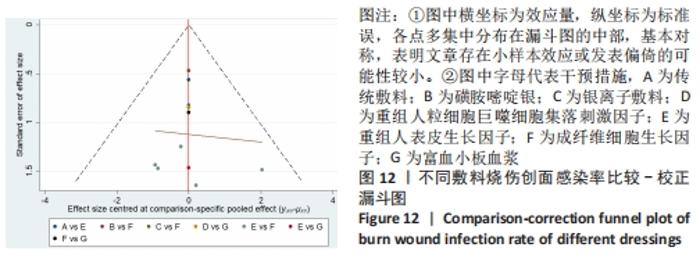
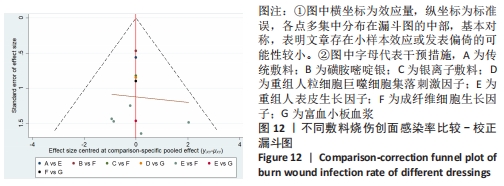
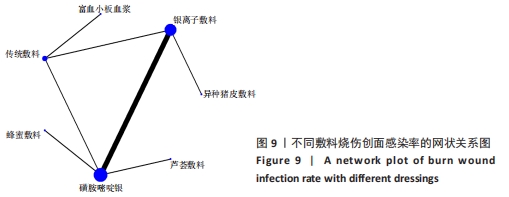
2.5 各研究烧伤创面感染率的网状Meta分析结果 2.5.1 结局指标证据网络 有9项研究报告了烧伤创面感染率[16,23-24,26,30,33,37,43,46],涉及7种敷料,分别为传统敷料,磺胺嘧啶银、银离子敷料、芦荟敷料、富血小板血浆、蜂蜜敷料和异种猪皮敷料。烧伤创面感染率的网状关系图见图9,图中点的大小代表该干预措施的数量,线的粗细代表涉及该2种干预措施对比的研究数量。 2.5.2 异质性及一致性检验结果 针对形成的1个闭环进行异质性检验,结果显示95%CI:0.00-3.88包含0,不一致因子(IF)=0.24,提示同质性较好。运用直接Meta分析对各研究间异质性进行分析,结果显示,整体I2=8.9%,P > 0.05,提示各研究间统计学异质性较小,故采用固定效应模型分析,见图10。"
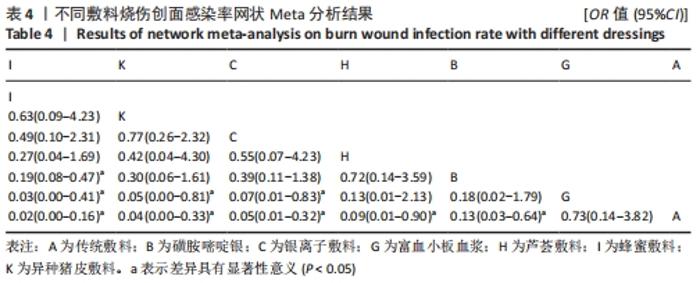
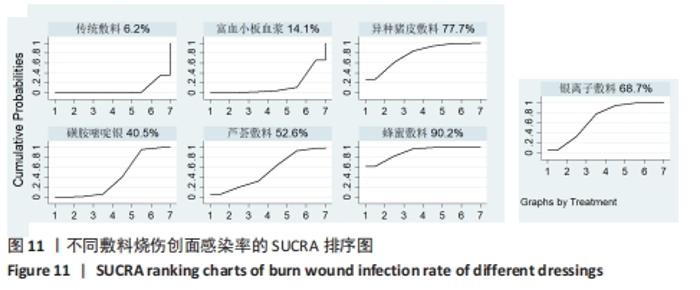
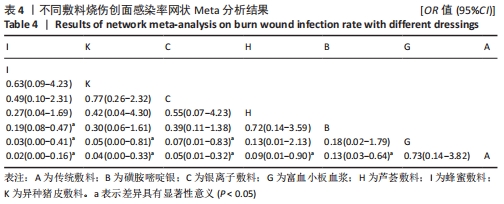
在进行网状Meta分析时,首先运用不一致性模型进行检验,结果显示P=0.892,I2=0.02,因P > 0.05说明不一致性检验不显著,一致性较好,可以使用一致性模型进行一致性拟合,通过一致性检验显示,P > 0.05,提示一致性较好。运用节点分裂法进行局部不一致性检验,结果显示P > 0.05,表明各研究间具有一致性,因此在一致性模型下进行网状Meta分析。 2.5.3 不同敷料烧伤创面感染率的网状Meta分析结果 纳入的9个随机对照试验,涉及7种敷料。网状Meta分析结果显示:在控制烧伤创面感染率上,蜂蜜敷料、异种猪皮敷料、银离子敷料、芦荟敷料和磺胺嘧啶银均优于传统敷料(P < 0.05);蜂蜜敷料、异种猪皮敷料及银离子敷料在控制感染率上均优于富血小板血浆(P < 0.05);相比磺胺嘧啶银,蜂蜜敷料抗感染效果更佳(P < 0.05),其他干预措施之间比较差异无显著性意义(P > 0.05),见表4。 "
| [1] 王正国.全球烧伤近况——来自世界卫生组织的报告[J].中华烧伤杂志,2001, 17(4):250-251. [2] PECK MD. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns. 2011;37(7):1087-1100. [3] WANG Y, TANG HT, XIA ZF, et al. Factors affecting survival in adult patients with massive burns. Burns. 2010;36(1):57-64. [4] Burn Incidence Fact Sheet-American Burn Association. https://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/. [5] 谢卫国.从中外比较看我国烧伤防治体系建设[J].中华烧伤杂志,2013,29(2):126-129. [6] 钟淑贤,石雨晴,杨亚兰,等.软聚硅酮银离子敷料应用于烧伤创面的效果评价[J]. 中国组织工程研究,2020,24(22): 3602-3608. [7] YUAN L, MINGHUA C, FEIFEI D, et al. Study of the use of recombinant human granulocyte-macrophage colony-stimulating factor hydrogel externally to treat residual wounds of extensive deep partial-thickness burn. Burns. 2015;41(5):1086-1091. [8] ROWAN MP, CANCIO LC, ELSTER EA, et al. Burn wound healing and treatment: review and advancements. Crit Care. 2015;19:243. [9] YANG C, XIONG AB, HE XC, et al. Efficacy and feasibility of amniotic membrane for the treatment of burn wounds: a meta-analysis. J Trauma Acute Care Surg. 2021;90(4):744-755. [10] CHAGANTI P, GORDON I, CHAO JH, et al. A systematic review of foam dressings for partial thickness burns. Am J Emerg Med. 2019;37(6):1184-1190. [11] PAGGIARO AO, BASTIANELLI R, CARVALHO VF, et al. Is allograft skin, the gold-standard for burn skin substitute? A systematic literature review and meta-analysis. J Plast Reconstruc Aesth Surg. 2019;72(8):1245-1253. [12] CHAGANTI P, GORDON I, CHAO JH, et al. A systematic review of foam dressings for partial thickness burns. Am J Emerg Med. 2019;37(6):1184-1190. [13] NIMIA HH, CARVALHO VF, ISAAC C, et al. Comparative study of Silver Sulfadiazine with other materials for healing and infection prevention in burns: a systematic review and meta-analysis. Burns. 2019; 45(2):282-292. [14] 王巍巍,杨智荣,孙凤,等.网状Meta分析GRADE证据总结表的制订、解读与应用[J].中国循证医学杂志,2020,20(12): 1471-1476. [15] HIGGINS JP, ALTMAN DG, GOTZSCHE PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [16] KARLSSON M, ELMASRY M, STEINVALL I, et al. Superiority of silver-foam over porcine xenograft dressings for treatment of scalds in children: a prospective randomised controlled trial. Burns. 2019;45(6):1401-1409. [17] YAN D, LIU S, ZHAO X, et al. Recombinant human granulocyte macrophage colony stimulating factor in deep second-degree burn wound healing. Medicine (Baltimore). 2017;96(22):e6881. [18] 胡强,隋爽,王国栋,等.rhGM-CSF凝胶与异种皮对深Ⅱ度烧伤创面愈合效果分析[J].医学研究杂志,2017,46(2):149-151. [19] Muangman P, Praditsuktavorn B, Chinaroonchai K, et al. Clinical efficacy test of polyester containing herbal extract dressings in burn wound healing. Int J Low Extrem Wounds. 2016;15(3):203-212. [20] TANG H, LV G, FU J, et al. An open, parallel, randomized, comparative, multicenter investigation evaluating the efficacy and tolerability of Mepilex Ag versus silver sulfadiazine in the treatment of deep partial-thickness burn injuries. J Trauma Acute Care Surg. 2015;78(5):1000-1007. [21] 吴宏志,李晓,杨蒙,等.自体富血小板血浆凝胶对中老年电烧伤患者创面愈合的影响[J].中国老年学杂志,2015,35(5): 1182-1184. [22] GENUINO GAS, BALUYUT-ANGELES KV, ESPIRITU APT, et al. Topical petrolatum gel alone versus topical silver sulfadiazine with standard gauze dressings for the treatment of superficial partial thickness burns in adults: a randomized controlled trial. Burns. 2014;40(7):1267-1273. [23] 邓海涛,赵耀华,徐丽红,等.亲水性纤维含银敷料治疗深Ⅱ度烧伤的疗效[J].江苏医药,2014,40(20):2460-2461. [24] SHAHZAD MN, AHMED N. Effectiveness of Aloe Vera gel compared with 1% silver sulphadiazine cream as burn wound dressing in second degree burns. J Pak Med Assoc. 2013;63(2):225-230. [25] MAGHSOUDI H, NEZAMI N, MIRZAJANZADEH M. Enhancement of burn wounds healing by platelet dressing. Int J Burns Trauma. 2013;3(2):96-101. [26] 张梅,唐洪泰,马兵,等.软聚硅酮银离子泡沫敷料在患者关节部位深Ⅱ度烧伤创面的应用[J].中华烧伤杂志,2013,29(3): 315-317. [27] YAN H, CHEN J, PENG X. Recombinant human granulocyte-macrophage colony-stimulating factor hydrogel promotes healing of deep partial thickness burn wounds. Burns. 2012;38(6):877-881. [28] MOSTAQUE AK, RAHMAN KBMA. Comparisons of the effects of biological membrane (amnion) and silver sulfadiazine in the management of burn wounds in children. J Burn Care Res. 2011;32(2):200-209. [29] SILVERSTEIN P, HEIMBACH D, MEITES H, et al. An open, parallel, randomized, comparative, multicenter study to evaluate the cost-effectiveness, performance, tolerance, and safety of a silver-containing soft silicone foam dressing (intervention) vs silver sulfadiazine cream. J Burn Care Res. 2011;32(6):617-626. [30] 周潘宇,夏照帆,贲道锋,等.爱康肤银离子敷料在小儿浅Ⅱ度烧伤创面的临床应用[J].第二军医大学学报,2011,32(12): 1321-1323. [31] 刘继松,方勇,姚敏,等.重组人粒细胞巨噬细胞集落刺激因子凝胶剂对深Ⅱ度烧伤创面溶痂及愈合影响的临床研究[J].中国修复重建外科杂志,2011,25(9):1059-1062. [32] MUANGMAN P, PUNDEE C, OPASANON S, et al. A prospective, randomized trial of silver containing hydrofiber dressing versus 1% silver sulfadiazine for the treatment of partial thickness burns. Int Wound J. 2010; 7(4):271-276. [33] MALIK KI, MALIK MA, ASLAM A. Honey compared with silver sulphadiazine in the treatment of superficial partial-thickness burns. Int Wound J. 2010;7(5):413-417. [34] MOHAMMADI AA, SABET B, RIAZI H, et al. Human amniotic membrane dressing: an excellent method for outpatient management of burn wounds. Iran J Med Sci. 2009;34(1):61-64. [35] KHORASANI G, HOSSEINIMEHR SJ, AZADBAKHT M, et al. Aloe versus silver sulfadiazine creams for second-degree burns: a randomized controlled study. Surg Today. 2009;39(7):587-591. [36] ZHANG L, CHEN J, HAN C. A multicenter clinical trial of recombinant human GM-CSF hydrogel for the treatment of deep second-degree burns. Wound Repair Regen. 2009; 17(5):685-689. [37] 陈炯,韩春茂,张力成,等.纳米银用于Ⅱ度烧伤创面的疗效及安全性评价[J]. 中华创伤杂志,2009,25(5):451-455. [38] AKITA S, AKINO K, IMAIZUMI T, et al. Basic fibroblast growth factor accelerates and improves second‐degree burn wound healing. Wound Repair Regen. 2008;16(5): 635-641. [39] BRANSKI LK, HERNDON DN, CELIS MM, et al. Amnion in the treatment of pediatric partial-thickness facial burns. Burns. 2008; 34(3):393-399. [40] MA B, CHENG DS, XIA ZF, et al. Randomized, multicenter, double-blind, and placebo-controlled trial using topical recombinant human acidic fibroblast growth factor for deep partial-thickness burns and skin graft donor site. Wound Repair Regen. 2007;15(6):795-799. [41] 梁自乾,黎洪棉,蒙诚跃.重组人表皮生长因子对儿童面部非Ⅲ度烧伤创面的修复[J].中国组织工程研究与临床康复, 2007,11(10):1974-1975. [42] HUANG Y, LI X, LIAO Z, et al. A randomized comparative trial between Acticoat and SD-Ag in the treatment of residual burn wounds, including safety analysis. Burns. 2007;33(2):161-166. [43] 陈炯,韩春茂,林小玮,等.纳米银敷料在修复Ⅱ度烧伤创面的应用研究[J].中华外科杂志,2006,44(1):50-52. [44] 王世岭,马建丽,柴家科,等.重组人表皮生长因子软膏对烧伤创面修复的促进作用[J].中国修复重建外科杂志,2002, 16(3):173-176. [45] FU X, SHEN Z, CHEN Y, et al. Randomised placebo-controlled trial of use of topical recombinant bovine basic fibroblast growth factor for second-degree burns. Lancet. 1998;352(9141):1661-1664. [46] YEUNG C, HSIEH P, WEI L, et al. Efficacy of lyophilised platelet-rich plasma powder on healing rate in patients with deep second degree burn injury a prospective double-blind randomized clinical trial. Ann Plast Surge. 2018;801:S66-S69. [47] YOSHINO Y, OHTSUKA M, KAWAGUCHI M, et al. The wound/burn guidelines - 6: Guidelines for the management of burns. J Dermatol. 2016;43(9):989-1010. [48] 张烨.组织工程人工真皮替代物研究进展综述及临床应用体会[D].广州:南方医科大学,2018. [49] ZHAO J, CHEN L, SHU B, et al. Granulocyte/macrophage colony-stimulating factor influences angiogenesis by regulating the coordinated expression of VEGF and the Ang/Tie system. PLoS One. 2014;9(3): e92691. [50] KRZYSZCZYK P, SCHLOSS R, PALMER A, et al. The role of macrophages in acute and chronic wound healing and interventions to promote pro-wound healing phenotypes. Front Physiol. 2018;9:419. [51] MANN A, BREUHAHN K, SCHIRMACHER P, et al. Keratinocyte-derived granulocyte-macrophage colony stimulating factor accelerates wound healing: stimulation of keratinocyte proliferation, granulation tissue formation, and vascularization. J Invest Dermatol. 2001;117(6):1382-1390. [52] FANG Y, SHEN J, YAO M, et al. Granulocyte-macrophage colony-stimulating factor enhances wound healing in diabetes via upregulation of proinflammatory cytokines. Br J Dermatol. 2010;162(3):478-486. [53] KAPLAN G, WALSH G, GUIDO LS, et al. Novel responses of human skin to intradermal recombinant granulocyte/macrophage-colony-stimulating factor: langerhans cell recruitment, keratinocyte growth, and enhanced wound healing. J Exp Med. 1992; 175(6):1717-1728. [54] WU F, DAI L, GENG L, et al. Practically feasible production of sustained-release microspheres of granulocyte-macrophage colony-stimulating factor (rhGM-CSF). J Control Release. 2017;259:195-202. [55] COKCETIN NN, PAPPALARDO M, CAMPBELL LT, et al. The Antibacterial Activity of Australian Leptospermum Honey Correlates with Methylglyoxal Levels. PLoS One. 2016; 11(12):e167780. [56] ALBARIDI NA. Antibacterial potency of honey. Int J Microbiol. 2019;2019:2464507. [57] ESCUREDO O, DOBRE I, FERNANDEZ-GONZALEZ M, et al. Contribution of botanical origin and sugar composition of honeys on the crystallization phenomenon. Food Chem. 2014;149:84-90. [58] BRUDZYNSKI K, ABUBAKER K, ST-MARTIN L, et al. Re-examining the role of hydrogen peroxide in bacteriostatic and bactericidal activities of honey. Front Microbiol. 2011; 2:213. [59] HUSSAIN MB. Role of honey in topical and systemic bacterial infections. J Altern Complement Med. 2018;24(1):15-24. [60] COOKE J, DRYDEN M, PATTON T, et al. The antimicrobial activity of prototype modified honeys that generate reactive oxygen species (ROS) hydrogen peroxide. BMC Res Notes. 2015;8:20. [61] MOLAN PC. The evidence supporting the use of honey as a wound dressing. Int J Low Extrem Wounds. 2006;5(1):40-54. [62] ZHU G, WANG Q, LU S, et al. Hydrogen peroxide: a potential wound therapeutic target? Med Princ Pract. 2017;26(4):301-308. [63] BOGDANOV S. Nature and origin of the antibacterial substances in honey. Lebensm Wissu Techol. 1997;30(7):748-753. [64] WASIHUN AG, KASA BG. Evaluation of antibacterial activity of honey against multidrug resistant bacteria in Ayder Referral and Teaching Hospital, Northern Ethiopia. Springerplus. 2016;5(1):842. [65] PATTAMAYUTANON P, ANGELI S, THAKEOW P, et al. Biomedical Activity and Related Volatile Compounds of Thai Honeys from 3 Different Honeybee Species. J Food Sci. 2015,80(10):M2228-M2240. [66] POSTMES T, VANDEPUTTE J. Recombinant growth factors or honey? Burns. 1999; 25(7):676-678. [67] KARAYIL S, DESHPANDE SD, KOPPIKAR GV. Effect of honey on multidrug resistant organisms and its synergistic action with three common antibiotics. J Postgrad Med. 1998;44(4):93-96. [68] WANG R, STARKEY M, HAZAN R, et al. Honey’s ability to counter bacterial infections arises from both bactericidal compounds and QS inhibition. Front Microbiol. 2012;3:144. [69] ATKINSON S, WILLIAMS P. Quorum sensing and social networking in the microbial world. J R Soc Interface. 2009;6(40):959-978. [70] CUTTING KF, WHITE RJ. Maceration of the skin and wound bed. 1: Its nature and causes. J Wound Care. 2002;11(7):275-278. [71] GOPAL SK, BALAJI M, SUBIKSHA G, et al. Honey based treatment strategies for infected wounds and burns: a systematic review of recent pre-clinical research. Wound Med. 2020 (prepublish). [72] VICTORIA CN, JAMES H, JONATHAN AGC. Dissecting the antimicrobial composition of honey. Antibiotics. 2019;8(4):251. [73] SIMON A, TRAYNOR K, SANTOS K, et al. Medical honey for wound care--still the ‘latest resort’? Evid Based Complement Alternat Med. 2009;6(2):165-173. [74] EGGER M, EBRAHIM S, SMITH GD. Where now for meta-analysis? Int J Epidemiol. 2002;31(1):1-5. |
| [1] | Jiang Xiaocheng, Shi Lu, Wang Yinbin, Li Qiujiang, Xi Chuangzhen, Ma Zefeng, Cai Lijun. Systematical evaluation of bone fusion rate after interbody fusion in patients with osteoporosis and lumbar degenerative disease treated with teriparatide [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1427-1433. |
| [2] | Zhou Jie, Pei Xibo, Wan Qianbing. Advances and biological application of asymmetric dressings [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 434-440. |
| [3] | You Aijia, Li Wenjie, Zhou Junli, Li Chun. Systematic evaluation of six dressings on wound safety following total hip and knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 486-492. |
| [4] | Jing Jinpeng, Zhang Yue, Liu Xiaomin, Liu Yi. Traditional Chinese medicine injection for promoting blood circulation in prevention of deep vein thrombosis after orthopedic surgery: network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1467-1476. |
| [5] | Liu Gang, Ma Chao, Wang Le, Zeng Jie, Jiao Yong, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Ankle-foot orthoses improve motor function of children with cerebral palsy: a Meta-analysis based on 12 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1299-1304. |
| [6] | Wang Nan, Qian Yuzhang, Xie Lin. Network Meta-analysis of different acupuncture methods for the treatment of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 813-820. |
| [7] | Wei Zhoudan, Li Wenjin, Zhu Li, Wang Yu, Zhao Jiaoyang, Chen Yanan, Guo Dong, Hao Min. Platelet-rich fibrin as a material for alveolar ridge preservation significantly reduces the resorption of alveolar bone height and width after tooth extraction: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 643-648. |
| [8] | Zhang Tiantian, Li Jiamin, Ou Liang, Shang Yan, Xu Yaqian, Hu Guoheng. Electromyographic biofeedback for post-stroke limb spasticity: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(29): 4742-4748. |
| [9] | An Dong, Liu Yang, Yang Tongjiang. Application of extracorporeal shock wave therapy in burn wound repair and post-burn scar treatment [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(20): 3265-3272. |
| [10] | Zhou Junli, Wang Xiaojun, Wang Haijiao, Li Chun. A network meta-analysis of the efficacy of new medical dressings for diabetic foot ulcers [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(16): 2562-2569. |
| [11] | Zhao Tianyu, Jin Song, Zhang Di, Liu Xiaoxiao, Ma Jiang, Wang Ju. Baduanjin training for patellar tendinopathy in a randomized controlled trial: improving pain, muscle flexibility and lower limb balance stability [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(11): 1662-1668. |
| [12] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [13] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [14] | Xiong Chen, He Guiping, Zhang Kun, He Xiao, Yang Jiarui, He Changjun, Wang Xiaolong, Wang Chen, Shi Zhengwei, Zhu Yangjun, Heng Lisong. Conservative treatment, open reduction, percutaneous minimally invasive plate internal fixation and intramedullary nail fixation in the treatment of humeral shaft fractures: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5878-5887. |
| [15] | Wan Dadi, Duan Xiangrui, Fan Xinchao, Yuan Ye, Huang Teng, Pan Dikang, Liu Jingyan, Li Xicheng. Efficacy of posterior cruciate ligament retaining versus posterior stabilized prostheses in total knee arthroplasty: a systematic review and a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5897-5904. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||