Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (36): 5897-5904.doi: 10.12307/2021.360
Efficacy of posterior cruciate ligament retaining versus posterior stabilized prostheses in total knee arthroplasty: a systematic review and a meta-analysis
Wan Dadi1,2, Duan Xiangrui1,2, Fan Xinchao1,3, Yuan Ye1,3, Huang Teng1, Pan Dikang2, Liu Jingyan2, Li Xicheng1
- 1Department of Orthopedics, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China; 2Graduate School of North China University of Science and Technology, Tangshan 063210, Hebei Province, China; 3Hebei North University, Zhangjiakou 075000, Hebei Province, China
-
Received:2021-03-22Revised:2021-03-24Accepted:2021-04-12Online:2021-12-28Published:2021-09-18 -
Contact:Li Xicheng, MD, Chief physician, Department of Orthopedics, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China -
About author:Wan Dadi, Master candidate, Department of Orthopedics, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China; Graduate School of North China University of Science and Technology, Tangshan 063210, Hebei Province, China
CLC Number:
Cite this article
Wan Dadi, Duan Xiangrui, Fan Xinchao, Yuan Ye, Huang Teng, Pan Dikang, Liu Jingyan, Li Xicheng. Efficacy of posterior cruciate ligament retaining versus posterior stabilized prostheses in total knee arthroplasty: a systematic review and a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5897-5904.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
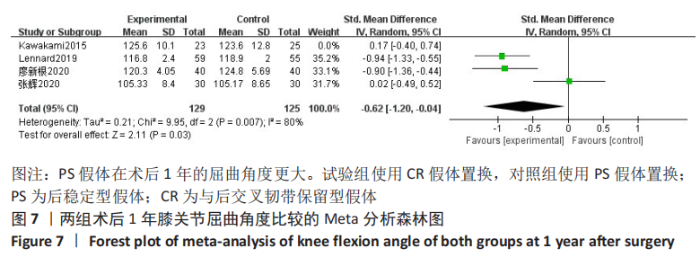
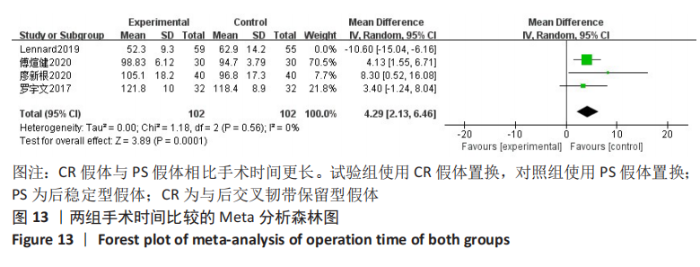
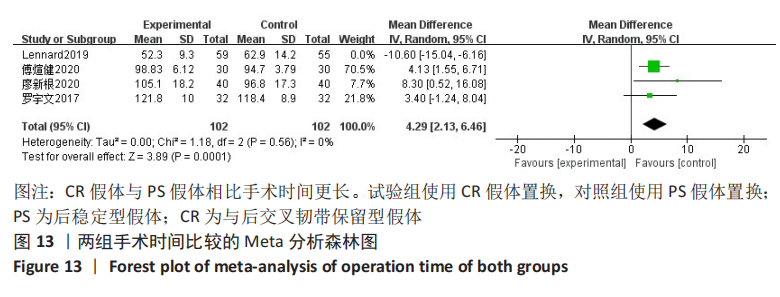
2.3.3 各组术后1年膝关节屈曲角度差异 4项研究对术后1年膝关节活动度进行了比较[3-4,10-11],Meta分析森林图显示存在统计学异质性(I2=83%,P=0.000 7),首先查找异质性的来源,使用敏感性分析,剔除1篇文献后异质性下降最大但不明显(I2=80%)[10],且Meta分析的结果改变。阅读全文后,考虑与此篇文章研究的对象为日本人,使用的假体不同,而且样本量较少有关;同时此篇文献随访的时间最长,这些原因可能导致了研究的异质性大。所以使用随机效应模型,结果表明,全膝关节置换使用CR假体与PS假体相比,在术后1年的膝关节屈曲角更小(SMD=-0.62,95%CI:-1.20至-0.04,P=0.03),见图7。"

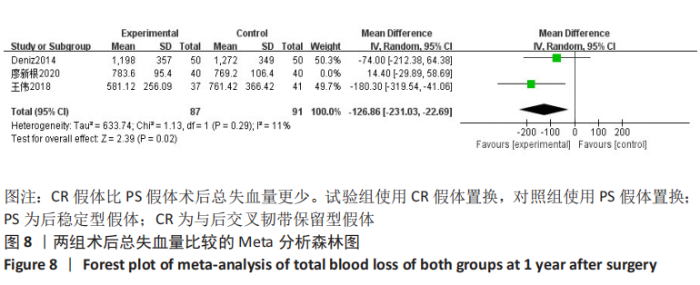
2.3.4 各组术后总失血量差异 共3项研究对术后总失血量进行了比较[3-4,8],Meta分析森林图显示存在统计学异质性(I2=74%,P=0.02),首先查找异质性的来源,使用敏感性分析,当剔除廖新根等[3]这篇文章时,异质性下降最明显(I2=11%),且Meta分析的结果发生改变。仔细阅读此篇文章后,考虑主要是与手术医师的熟练度、止血带使用的时间、引流管放置的位置以及术后应用低分子肝素预防下肢血栓有关,这些因素导致了文献的异质性偏大。故使用随机效应模型,结果表明,全膝关节置换使用CR假体比PS假体术后总失血量更少(WMD=-126.86,95%CI:-231.03至-22.69,P=0.02),见图8。"


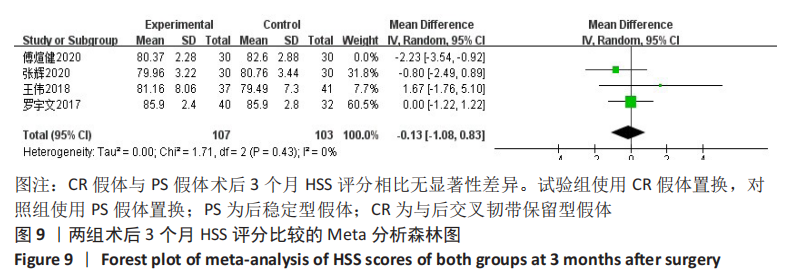
2.3.5 各组术后3个月目测类比评分差异 共2项研究对术后目测类比评分进行了比较[4,6]。因为文献较少,故进行描述性分析。傅煊健等[6]对60例行全膝关节置换的膝关节炎患者进行了回顾性分析,其中30例使用CR假体,30例使用PS假体,随访3个月以上。结果表明,在术后3个月CR假体组的目测类比评分为(2.63±0.85)分,PS假体患者为(1.80±0.76)分,两者比较差异显著(P < 0.05)。张辉等[4]回顾性分析了60例行全膝关节置换的患者,其中30例使用CR假体,30例使用PS假体,随访5-16个月,结果术后3个月CR假体组患者的目测类比评分为(1.56±0.67)分,PS假体组患者为(1.66±0.71)分,两者比较无显著性差异(P > 0.05)。此2篇文献的结论不同,考虑主要与评估目测类比评分的人员、术者熟练度、术后止疼药应用的方式等不同有关[4,6]。 2.3.6 各组术后3个月HSS评分差异 共4项研究对术后3个月HSS评分进行了比较[2,4-6],Meta分析森林图显示存在统计学异质性(I2=63%,P=0.04),首先查找异质性的来源,进行敏感性分析,逐一剔除文献后发现在剔除傅煊健等[6]的研究时异质性改变最大(I2=0%),但Meta分析的结果未改变,说明结果较稳定。仔细阅读全文后,考虑主要是由于术者熟练度、HSS评分者、术后患者是否主动进行功能锻炼等原因造成的异质性。使用随机效应模型,结果表明,全膝关节置换使用CR假体与PS假体相比术后3个月HSS评分无显著性差异(WMD=-0.13,95%CI:-1.08-0.83,P=0.80),见图9。"
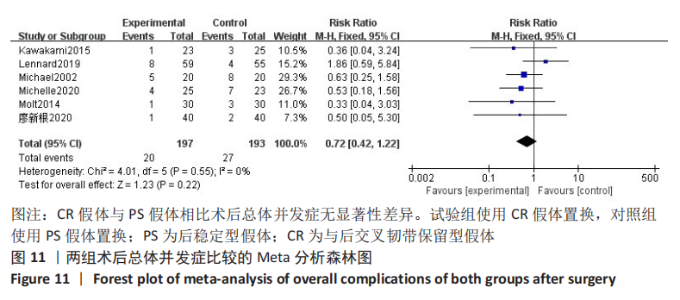
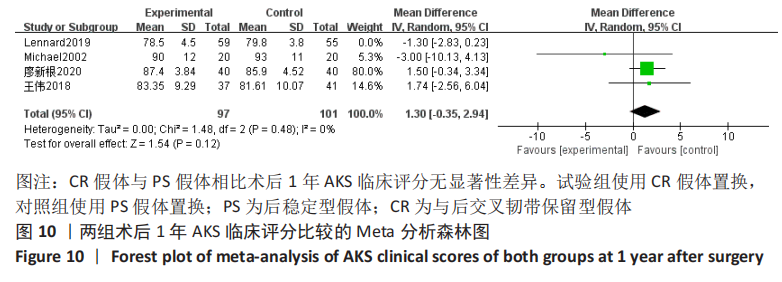
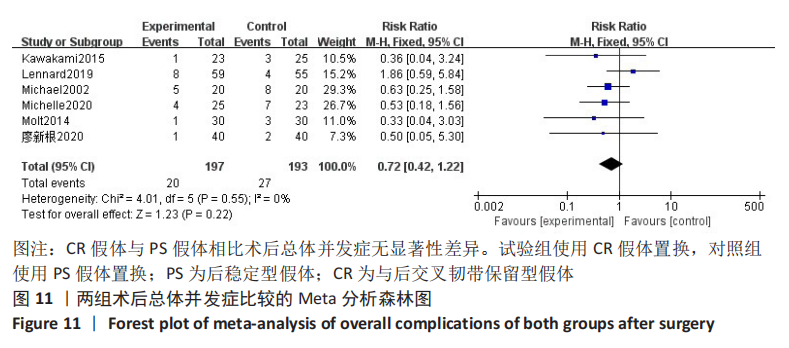
2.3.8 各组术后1年AKS膝功能评分差异 共2项研究对术后1年AKS膝功能评分进行了比较[3,7],因研究数较少,故行描述性分析。廖新根等[3]采用随机对照试验分析了80例行全膝关节置换的患者,其中40例PS假体,40例CR假体,随访一两年,结果表明术后1年AKS膝功能评分,在CR假体组为(76.3±7.5)分,在PS假体组为(75.2±8.2)分,差异无显著性意义(P > 0.05)。有1项随机对照试验对40例全膝关节置换患者进行了分析[7],包括20例PS假体,20例CR假体。术后2年的AKS膝功能评分在PS假体组为(76±28)分,在CR假体组为(73±24)分,差异无显著性意义(P > 0.05)。此2项研究的结果均表明术后AKS膝功能评分无显著性差异[3,7]。 2.3.9 各组总体并发症差异 共6项随机对照试验对术后总体并发症进行了比较[3,7,9-12],Meta分析森林图显示不存在统计学异质性(I2=0%,P=0.55),使用固定效应模型。结果表明,全膝关节置换使用CR假体与PS假体相比术后总体并发症无显著性差异(RR=0.72,95%CI:0.42-1.22,P=0.22),见图11。"
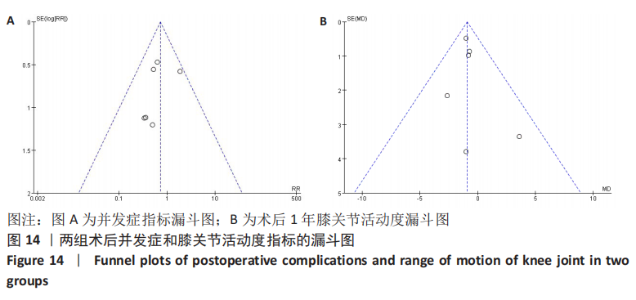
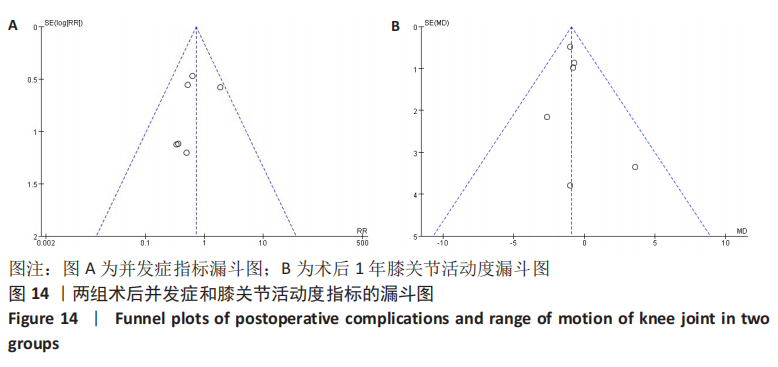
2.3.12 各组术后膝关节遗忘度差异 有1篇文献研究了术后膝关节遗忘度[4],侧重评估全膝关节置换后的患者在平时生活中遗忘膝关节假体存在的主观感觉,与平时医师做出的HSS、AKS等客观的膝关节评分不同。张辉等[4]回顾性分析了60例使用全膝关节置换的患者,随访5-16个月发现,术后3个月PS假体组与CR假体组患者的膝关节遗忘度评分无显著性差异(P > 0.05)。 2.3.13 各组术后膝关节KT-1000测量值变化 有1篇文献研究了术后KT-1000测量值[3],在患者屈膝30°时使用KT-1000 仪器进行测量,结果表明术后1年膝关节KT-1000 测量值在CR假体组为(3.7±1.75) mm,在PS假体组为(4.8±1.42) mm,两者的KT-1000测量值比较差异无显著性意义。 2.4 发表偏倚分析 以纳入研究最多的不良结局做漏斗图,均为随机对照试验,选用RR指标作为效应量,可见图形双侧不十分对称,可能有发表偏倚,见图14A。 再以主要结局指标之一的膝关节活动度做漏斗图,可见图形双侧不十分对称,可能有发表偏倚,见图14B。"
| [1] MOHER D, LIBERATI A, TETZLAFF J,等.系统综述和荟萃分析优先报告的条目:PRISMA声明[J].中西医结合学报,2009,7(9): 889-896. [2] 王伟.CR假体与PS假体置换治疗中重度膝骨关节炎的短期临床效果对比研究[D].银川:宁夏医科大学,2018:1-80. [3] 廖新根,唐智明,吴梨华,等.保留和不保留后交叉韧带的全膝关节置换治疗重度骨关节炎近期疗效前瞻对照研究[J].实用医学杂志,2020,36(19):2672-2677. [4] 张辉,李鸿,李叶天,等.后交叉韧带保留型和后稳定型全膝关节假体置换后早期关节遗忘度的对比[J].中国组织工程研究,2020,24(30):4802-4806. [5] 罗宇文,刘世桢,周雪明,等.后交叉韧带保留型及替代型假体在全膝关节置换后早期疗效比较[J].广东医科大学学报, 2017,35(4):381-384. [6] 傅煊健,陈扬,利春叶.后稳定型与后交叉韧带保留型假体TKA治疗膝关节骨性关节炎的疗效比较[J].中国骨与关节损伤杂志,2020,35(2):178-180. [7] TANZER M, SMITH K, BURNETT S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: balancing the gap. J Arthroplasty. 2002;17(7):813-819. [8] CANKAYA D, OZKURT B, AYDIN C, et al. No difference in blood loss between posterior-cruciate-ligament-retaining and posterior-cruciate-ligament-stabilized total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1865-1869. [9] MOLT M, TOKSVIG-LARSEN S. Similar early migration when comparing CR and PS in Triathlon™ TKA: a prospective randomised RSA trial. Knee. 2014;21(5):949-954. [10] KAWAKAMI Y, MATSUMOTO T, TAKAYAMA K, et al. Intermediate-term comparison of posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty using the new knee scoring system. Orthopedics. 2015;38(12):e1127-e1132. [11] VAN DEN BOOM LGH, BROUWER RW, VAN DEN AKKER-SCHEEK I, et al. No difference in recovery of patient-reported outcome and range of motion between cruciate retaining and posterior stabilized total knee arthroplasty: a double-blind randomized controlled trial. J Knee Surg. 2020;33(12):1243-1250. [12] DOWSEY MM, GOULD DJ, SPELMAN T, et al. A randomized controlled trial comparing a medial stabilized total knee prosthesis to a cruciate retaining and posterior stabilized design: a report of the clinical and functional outcomes following total knee replacement. J Arthroplasty. 2020;35(6):1583. [13] DION CB, HOWARD JL, LANTING BA, et al. Does recession of the posterior cruciate ligament influence outcome in total knee arthroplasty? J Arthroplasty. 2019;34(10):2383-2387. [14] GEORGAKLIS VA, KARACHALIOS T, MAKRIDIS KG, et al. Genesis 1 posterior cruciate-retaining total knee arthroplasty with asymmetric tibial tray: an 18-to-26-year long-term clinical outcome study. Knee. 2019;26(4):838-846. [15] BEACH A, REGAZZOLA G, NERI T, et al. The effect of knee prosthesis design on tibiofemoral biomechanics during extension tasks following total knee arthroplasty. Knee. 2019;26(5):1010-1019. [16] JIANG C, LIU Z, WANG Y, et al. Posterior cruciate ligament retention versus posterior stabilization for total knee arthroplasty: a meta-analysis. PLoS One. 2016;11(1):e0147865. [17] D’ANCHISE R, ANDREATA M, BALBINO C, et al. Posterior cruciate ligament-retaining and posterior-stabilized total knee arthroplasty: differences in surgical technique. Joints. 2013;1(1):5-9. [18] SONG SJ, PARK CH, BAE DK. What to know for selecting cruciate-retaining or posterior-stabilized total knee arthroplasty. Clin Orthop Surg. 2019;11(2):142-150. [19] BAE DK, SONG SJ, KIM KI, et al. Intraoperative factors affecting conversion from cruciate retaining to cruciate substituting in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3247-3253. [20] MIHALKO WM, MILLER C, KRACKOW KA. Total knee arthroplasty ligament balancing and gap kinematics with posterior cruciate ligament retention and sacrifice. Am J Orthop (Belle Mead NJ). 2000;29(8): 610-616. [21] SU E P. Fixed flexion deformity and total knee arthroplasty. J Bone Joint Surg Br. 2012;94(11 Suppl A):112-115. [22] LOMBARDI AV JR, BEREND KR. Posterior cruciate ligament-retaining, Posterior stabilized, and varus/valgus posterior stabilized constrained articulations in total knee arthroplasty. Instr Course Lect. 2006; 55:419-427. [23] SIERRA RJ, BERRY DJ. Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty. 2008;23(7 Suppl): 20-23. [24] VAN OPSTAL N, FEYEN H, LUYCKX JP, et al. Mean tensile strength of the PCL in TKA depends on the preservation of the tibial insertion site. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):273-278. [25] OKAZAKI K, TASHIRO Y, MIZU-UCHI H, et al. Influence of the posterior tibial slope on the flexion gap in total knee arthroplasty. Knee. 2014;21(4):806-809. [26] SONG SJ, PARK CH, BAE DK. What to know for selecting cruciate-retaining or posterior-stabilized total knee arthroplasty. Clin Orthop Surg. 2019;11(2):142-150. [27] HATAYAMA K, TERAUCHI M, HASHIMOTO S, et al. Factors associated with posterior cruciate ligament tightness during cruciate-retaining total knee arthroplasty. J Arthroplasty. 2018;33(5):1389-1393. [28] TSAI TY, LIOW MHL, PENG Y, et al. In-vivo elongation of anterior and posterior cruciate ligament in bi-cruciate retaining total knee arthroplasty. J Orthop Res. 2018; 36(12):3239-3246. [29] ZHANG B, LIN Y, REN S, et al. Effectiveness comparison of partial versus intact posterior cruciate ligament-retaining in total knee arthroplasty with cruciate-retaining prosthesis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(1):51-57. [30] KHASIAN M, MECCIA BA, LACOUR MT, et al. Effects of posterior tibial slope on a posterior cruciate retaining total knee arthroplasty kinematics and kinetics. J Arthroplasty. 2021;36(7):2379-2385. [31] SAVOV P, MIELKE E, WINDHAGEN H, et al. Higher revision rate for posterior cruciate-retaining than posterior-stabilized total knee arthroplasty for the treatment of valgus osteoarthritis. Arch Orthop Trauma Surg. 2021;141(2):305-312. |
| [1] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [2] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [3] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [4] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [5] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [6] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [7] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [8] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [9] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [10] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| [11] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| [12] | Yuan Jiawei, Zhang Haitao, Jie Ke, Cao Houran, Zeng Yirong. Underlying targets and mechanism of Taohong Siwu Decoction in prosthetic joint infection on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1428-1433. |
| [13] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [14] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [15] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||