Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (6): 977-984.doi: 10.3969/j.issn.2095-4344.4006
Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis
Zhan Fangbiao1, Cheng Jun1, Zou Xinsen2, Long Jie1, Xie Lizhong1, Deng Qianrong3
- 1Department of Orthopedics, 2Department of Critical Care Medicine, 3Health Management Center, Three Gorges Hospital Affiliated to Chongqing University (Chongqing Three Gorges Central Hospital), Chongqing 404000, China
-
Received:2020-03-19Revised:2020-03-24Accepted:2020-04-27Online:2021-02-28Published:2020-12-05 -
Contact:Xie Lizhong, Associate chief physician, Department of Orthopedics, Three Gorges Hospital Affiliated to Chongqing University (Chongqing Three Gorges Central Hospital), Chongqing 404000, China Deng Qianrong, Attending physician, Health Management Center, Three Gorges Hospital Affiliated to Chongqing University (Chongqing Three Gorges Central Hospital), Chongqing 404000, China -
About author:Zhan Fangbiao, Doctoral candidate, Associate chief physician, Department of Orthopedics, Three Gorges Hospital Affiliated to Chongqing University (Chongqing Three Gorges Central Hospital), Chongqing 404000, China
CLC Number:
Cite this article
Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
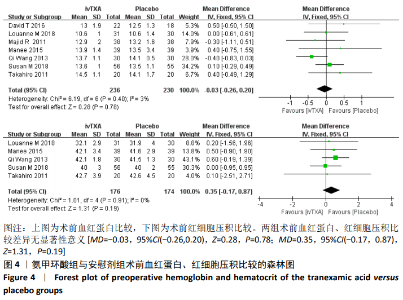
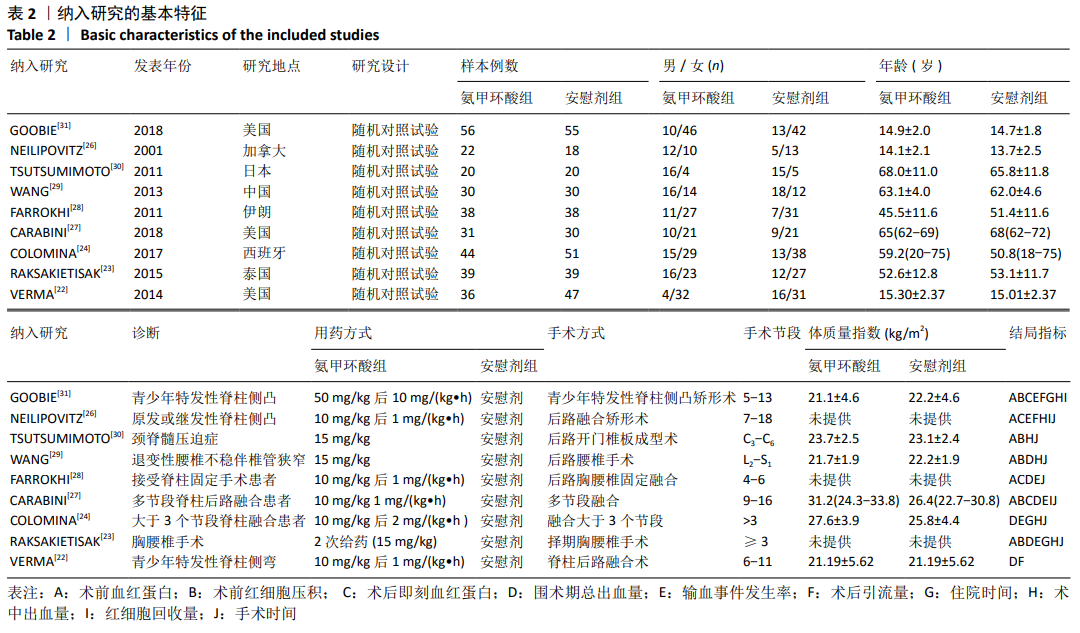
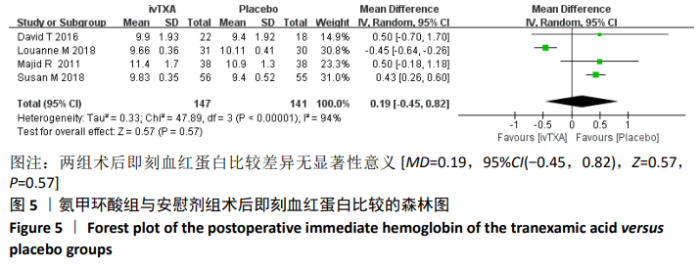
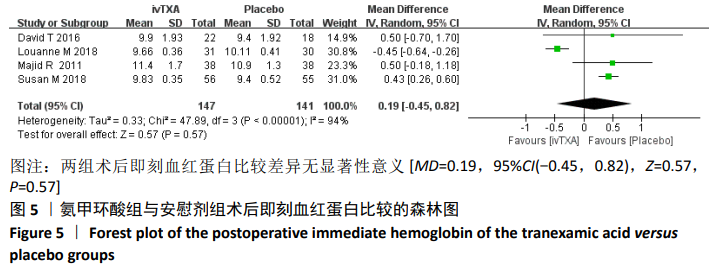
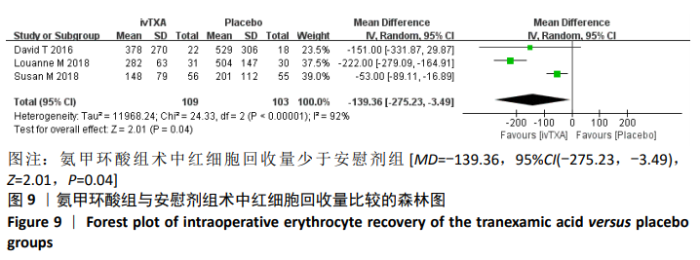
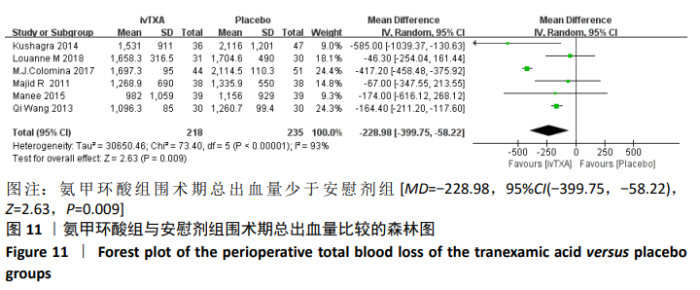
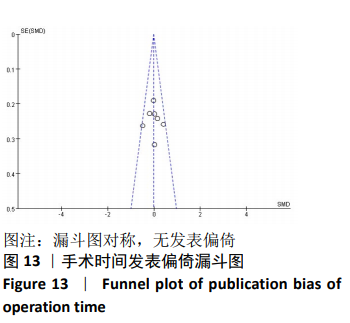
2.4 Meta分析结果 2.4.1 两组术前血红蛋白及红细胞压积差异的Meta分析结果 有7篇文献详细比较了术前血红蛋白[23-24,26-30],5篇文献详细比较了术前红细胞压积[23,27,29-31]。介绍术前血红蛋白的7篇文献间无异质性(Chi2=6.19,df=6,P=0.40,I2=3%),可以选择固定效应模型进行Meta分析。介绍术前红细胞压积的5篇文献间无异质性(Chi2=1.01,df=4,P=0.91,I2=0%),可以选择固定效应模型进行Meta分析。Meta分析结果显示,两组术前血红蛋白、红细胞压积比较差异无显著性意义[MD= -0.03,95%CI(-0.26,0.20),Z=0.28,P=0.78;MD=0.35,95%CI(-0.17,0.87),Z=1.31,P=0.19],见图4。"

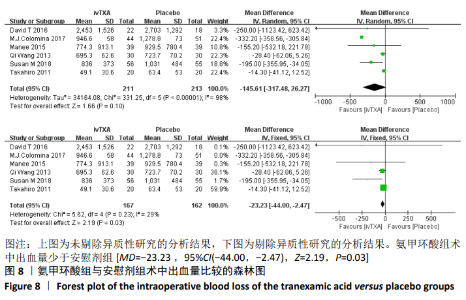
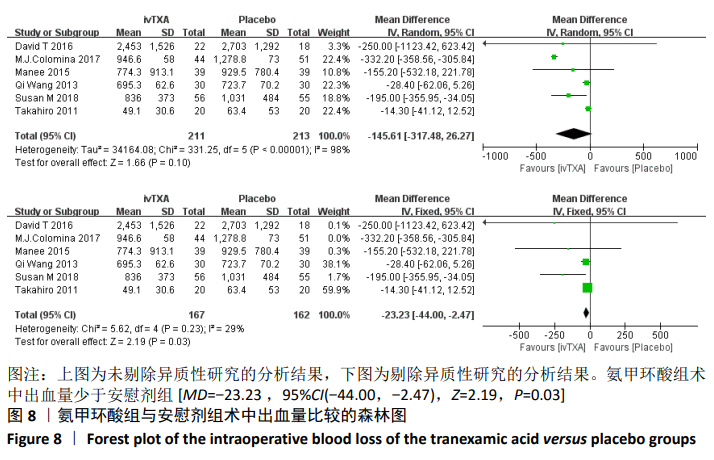
2.4.5 两组术中出血量差异的Meta分析结果 有6篇文献详细比较了术中出血量[23-24,26,27-331]。6篇文献间有异质性(Chi2=331.25,df=5,P < 0.000 01,I2=98%),逐一剔除文献进行敏感性分析,发现剔除COLOMINA等[24]后的总效应量合并值[MD=-23.23,95%CI (-44.00,-2.47)]与未剔除时的总效应量合并值[MD=-145.61,95%CI(-317.48,26.27)]存在较大差异,提示该研究可能导致研究结果不稳定,分析原因可能为COLOMINA等研究中两组患者基线中年龄(P=0.01)和体质量指数(P=0.03)均有显著性差异,故剔除COLOMINA等的研究进行Meta分析。剩余的5篇研究无异质性(Chi2=5.62,df=4,P=0.23,I2=29%)[23,26,29-31],选择固定效应模型进行Meta分析。Meta分析结果显示,氨甲环酸组术中出血量少于安慰剂组[MD=-23.23 ,95%CI(-44.00,-2.47),Z=2.19,P=0.03],见图8。"
| [1] ZHANG Y, LIU H, HE F, et al. Does Tranexamic Acid Improve Bleeding, Transfusion, and Hemoglobin Level in Patients Undergoing Multilevel Spine Surgery? A Systematic Review and Meta-Analysis.World Neurosurg. 2019;127:289-301. [2] WILLNER D, SPENNATI V, STOHL S, et al. Spine surgery and blood loss:Systematic review of clinical evidence.Anesth Analg. 2016;123:1307-1315. [3] LAN T, HU SY, YANG XJ, et al. The efficacy of bipolar sealer on blood loss in spine surgery: A meta-analysis.Eur Spine J.2017;26:1796-1802. [4] SCHWARZKOPF R, CHUNG C, PARK JJ, et al. Effects of perioperative blood product use on surgical site infection following thoracic and lumbar spinal surgery.Spine (Phila Pa 1976). 2010;35(3):340-346. [5] ALTER HJ, KLEIN HG. The hazards of blood transfusion in historical perspective.Blood. 2008;112(7):2617-2626. [6] SANDLER SG, YU H, RASSAI N, et al. Risks of blood transfusion and their prevention.Clin Adv Hematol Oncol.2003;1(5):307-313. [7] MUELLER MM, VAN RH, MEYBOHM P, et al. Patient Blood Management Recommendations From the 2018 Frankfurt Consensus Conference.JAMA. 2019;321 (10):983-997. [8] ZENG Y, SHEN B, YANG J, et al. Tranexamic acid administration in primary total hip arthroplasty: a randomized controlled trial of intravenous combined with topical versus single-dose intravenous administration.J Bone Joint Surg Am.2016;98:983-991. [9] WANG CD, KANG PD, MA J, et al. Single-dose tranexamic acid for reducing bleeding and transfusions in total hip arthroplasty: a double-blind, randomized controlled trial of different doses.Thromb Res.2016;141:119-123. [10] WANG N, XIONG X, XU L, et al. Transfusions and cost-benefit of oral versus intravenous tranexamic acid in primary total hip arthroplasty A meta-analysis of randomized controlled trials.Medicine (Baltimore).2019;98(17):e15279. [11] ALTAWIL Z, GENDRON BJ, SCHECHTER-PERKINS EM, et al. Topical use of tranexamic acid for the management of post-procedural rectal bleeding.Am J Emerg Med. 2019;37(1):173.e3-173.e4. [12] SMITH SR, MURRAY D, POCKNEY PG, et al. Tranexamic Acid for Lower GI Hemorrhage: A Randomized Placebo-Controlled Clinical Trial.Dis Colon Rectum.2018;61(1):99-106. [13] ZHANG HZ, DONG L, WANG HM, et al. Safety and efficacy of tranexamic acid in spinal canal tumors: a retrospective cohort study.Br J Neurosurg.2020:1-3. [14] BUKHARI NS, JOOMA R. Early tranexamic acid in traumatic brain injury: Evidence for an effective therapy.J Pak Med Assoc.2020;70(Suppl 1)(2):S49-S52. [15] SENTILHES L, DANIEL V, DENEUX-THARAUX C, et al. TRAAP2 - TR. Anexamic Acid for Preventing postpartum hemorrhage after cesarean delivery: a multicenter randomized, doubleblind, placebo- controlled trial - a study protocol.BMC Pregnancy Childbirth.2020;20(1):63. [16] SAMY A, RASLAN AN, TALAAT B, et al. Perioperative nonhormonal pharmacological interventions for bleeding reduction during open and minimally invasive myomectomy: a systematic review and network meta-analysis.Fertil Steril.2020;113(1):224-233.e6. [17] ZHANG Y, JIA Y, SHI J, et al. Safety and efficacy of tranexamic acid in paediatric cardiac surgery: study protocol for a double-blind randomised controlled trial.BMJ Open. 2019;9(11):e032642. [18] PING WD, ZHAO QM, SUN HF, et al. Role of tranexamic acid in nasal surgery A systemic review and meta-analysis of randomized control trial.Medicine (Baltimore). 2019; 98(16):e15202. [19] CHAMBERS S, TIDWELL L, KERKHOF A, et al. Topical Tranexamic Acid Is Effective in Cementless Total Knee Arthroplasty.Orthop Clin North Am.2020;51(1):7-11. [20] HINES JT, PETIS SM, AMUNDSON AW, et al. Intravenous Tranexamic Acid Safely and Effectively Reduces Transfusion Rates in Revision Total Knee Arthroplasties.J Bone Joint Surg Am.2020;102(5):381-387. [21] FATIMA N, BARRA ME, ROBERTS RJ, et al. Advances in surgical hemostasis: a comprehensive review and meta-analysis on topical tranexamic acid in spinal deformity surgery.Neurosurg Rev.2020.doi: 10.1007/s10143-020-01236-z. [22] VERMA K, ERRICO T, DIEFENBACH C, et al. The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis: a prospective randomized trial.J Bone Joint Surg Am.2014;96(10):e80. [23] RAKSAKIETISAK M, SATHITKARNMANEE B, SRISAEN P, et al. Two Doses of Tranexamic Acid Reduce Blood Transfusion in Complex Spine Surgery: A Prospective Randomized Study.Spine (Phila Pa 1976). 2015;40(24):E1257-1263. [24] COLOMINA MJ, KOO M, BASORA M, et al. Intraoperative tranexamic acid use in major spine surgery in adults: a multicentre, randomized, placebo-controlled trial.Br J Anaesth.2017;118(3):380-390. [25] HIGGINS JP, GREEN S. Cochrane handbook for systematic reviews of interventions version 5.1.0.Naunyn Schmiedebergs Arch Pharmakol.2011;5:S38. [26] NEILIPOVITZ DT, MURTO K, HALL L, et al. A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery.Anesth Analg.2001;93(1):82-87. [27] CARABINI LM, MORELAND NC, VEALEY RJ, et al. A Randomized Controlled Trial of Low-Dose Tranexamic Acid versus Placebo to Reduce Red Blood Cell Transfusion During Complex Multilevel Spine Fusion Surgery.World Neurosurg.2018;110:e572-e579. [28] FARROKHI MR, KAZEMI AP, EFTEKHARIAN HR, et al. Efficacy of prophylactic low dose of tranexamic acid in spinal fixation surgery:a randomized clinical trial.J Neurosurg Anesthesiol.2011;23(4):290-296. [29] WANG Q, LIU J, FAN R, et al. Tranexamic acid reduces postoperative blood loss of degenerative lumbar instability with stenosis in posterior approach lumbar surgery: a randomized controlled trial.Eur Spine J.2013;22(9):2035-2038. [30] TSUTSUMIMOTO T, SHIMOGATA M, OHTA H, et al. Tranexamic acid reduces perioperative blood loss in cervical laminoplasty: a prospective randomized study.Spine(Phila Pa 1976).2011;36(23):1913-1918. [31] GOOBIE SM, ZURAKOWSKI D, GLOTZBECKER MP, et al. Tranexamic Acid Is Efficacious at Decreasing the Rate of Blood Loss in Adolescent Scoliosis Surgery.J Bone Joint Surg Am.2018;100(23):2024-2032. [32] HUR SR, HUIZENGA BA, MAJOR M. Acute normovolemic hemodilution combined with hypotensive anesthesia and other techniques to avoid homologous transfusion in spinal fusion surgery.Spine (Phila Pa 1976). 1992;17(8):867-873. [33] NEILIPOVITZ DT. Tranexamic acid for major spinal surgery.Eur Spine J.2004;13 Suppl 1: S62-65. [34] SUN H, DENG L, DENG J, et al. The Efficacy and Safety of Prophylactic Intravenous Tranexamic Acid on Perioperative Blood Loss in Patients Treated with Posterior Lumbar Interbody Fusion.World Neurosurg. 2019;125:e198-e204. [35] PERNIK MN, DOSSELMAN LJ, AOUN SG, et al. The effectiveness of tranexamic acid on operative and perioperative blood loss in long-segment spinal fusions: a consecutive series of 119 primary procedures.J Neurosurg Spine.2020:1-7. |
| [1] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [2] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [3] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [4] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [5] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [6] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [7] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [8] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [9] | Xu Yulin, Shen Shi, Zhuo Naiqiang, Yang Huilin, Yang Chao, Li Yang, Zhao Heng, Zhao Lu. Biomechanical comparison of three different plate fixation methods for acetabular posterior column fractures in standing and sitting positions [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 826-830. |
| [10] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [11] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [12] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [13] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [14] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [15] | Ye Haimin, Ding Linghua, Kong Weihao, Huang Zutai, Xiong Long. Role and mechanism of hierarchical microchanneled bone scaffolds in promoting osteogenesis and angiogenesis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 621-625. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||