Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (31): 4928-4934.doi: 10.12307/2022.953
Previous Articles Next Articles
Neuroprotective effect of umbilical cord mesenchymal stem cell-derived exosomes on hippocampal neurons in mice with intracerebral hemorrhage
Wang Xue1, 2, Liu Yang1, 2, Xu Jianfeng2, Long Qianfa3, Wang Tong2, Zhong Jun2
- 1Department of Neurosurgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China; 2Department of Neurosurgery, The Third Hospital of Mianyang (Sichuan Mental Health Center), Mianyang 621000, Sichuan Province, China; 3Department of Neurosurgery, Xi’an Central Hospital, Xi’an 710003, Shaanxi Province, China
-
Received:2021-11-26Accepted:2022-01-21Online:2022-11-08Published:2022-04-24 -
Contact:Liu Yang, MD, Chief physician, Department of Neurosurgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China; Department of Neurosurgery, The Third Hospital of Mianyang (Sichuan Mental Health Center), Mianyang 621000, Sichuan Province, China -
About author:Wang Xue, Master candidate, Department of Neurosurgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China; Department of Neurosurgery, The Third Hospital of Mianyang (Sichuan Mental Health Center), Mianyang 621000, Sichuan Province, China -
Supported by:Sichuan Medical Association Support Project, No. S20013 (to LY); Mianyang Municipal Health Commission Support Project, No. 201901 (to LY); Mianyang Municipal Health Commission Encourages Project, No. 202141 (to LY)
CLC Number:
Cite this article
Wang Xue, Liu Yang, Xu Jianfeng, Long Qianfa, Wang Tong, Zhong Jun. Neuroprotective effect of umbilical cord mesenchymal stem cell-derived exosomes on hippocampal neurons in mice with intracerebral hemorrhage[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(31): 4928-4934.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
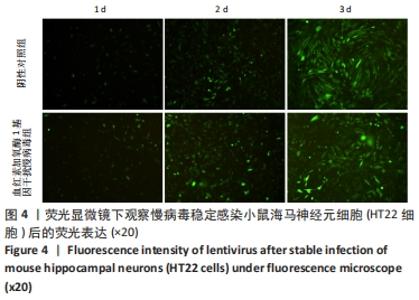
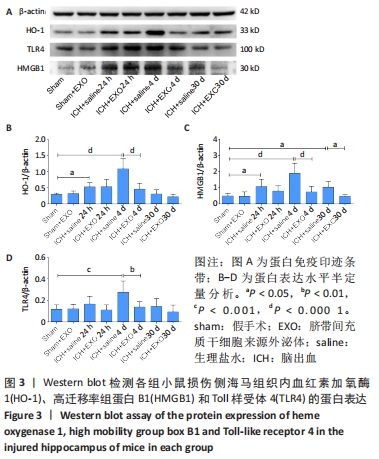
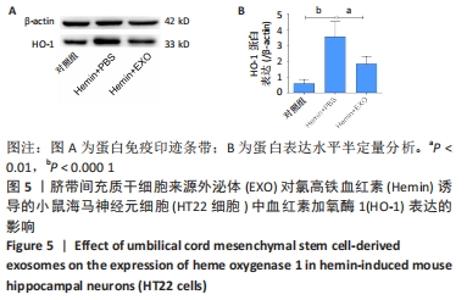
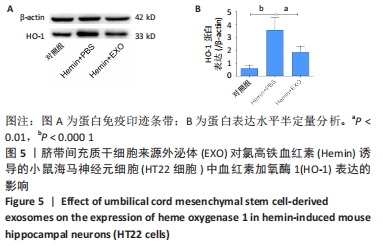
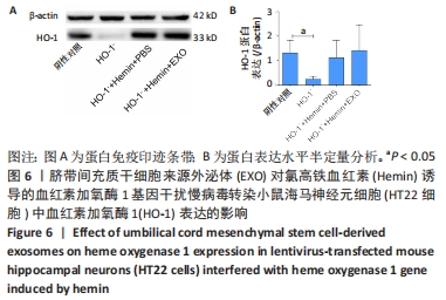
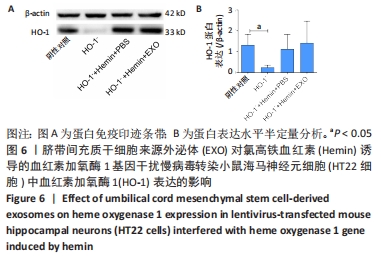
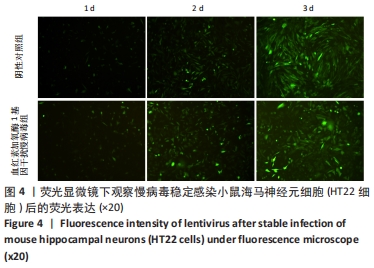
2.3 慢病毒稳定感染HT22细胞 以感染复数值为30的慢病毒感染HT22细胞,在倒置荧光显微镜下观察细胞荧光表达。阴性对照慢病毒及血红素加氧酶1基因干扰慢病毒感染HT22细胞,图4中可见第3天荧光表达最明显,转染效率约为80%,细胞状态良好,表明转染效率稳定,可进一步实验。 2.4 体外验证脐带间充质干细胞来源外泌体通过血红素加氧酶1介导发挥作用 蛋白免疫印迹结果显示,与对照组比较,氯高铁血红素刺激HT22细胞后血红素加氧酶1蛋白表达量显著升高,但予以外泌体预处理后血红素加氧酶1表达明显降低(均P < 0.05),见图5;当慢病毒转染HT22细胞敲低血红素加氧酶1表达后,与阴性对照慢病毒组相比,血红素加氧酶1基因干扰慢病毒组血红素加氧酶1的表达显著下降(P < 0.05);血红素加氧酶1基因干扰慢病毒+氯高铁血红 素+PBS组与血红素加氧酶1基因干扰慢病毒+氯高铁血红素+外泌体组血红素加氧酶1的表达差异无显著性意义(P > 0.05),见图6。"
| [1] LIU M, WU B, WANG WZ, et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6(5): 456-464. [2] FALLENIUS M, SKRIFVARS MB, REINIKAINEN M, et al. Spontaneous Intracerebral Hemorrhage. Stroke. 2019;50(9):2336-2343. [3] TSAI CF, THOMAS B, SUDLOW CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology. 2013;81(3):264-272. [4] GONG YH, HAO SL, WANG BC. Mesenchymal Stem Cells Transplantation in Intracerebral Hemorrhage: Application and Challenges. Front Cell Neurosci. 2021;15:653367. [5] EL ANDALOUSSI S, MÄGER I, BREAKEFIELD XO, et al. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013;12(5):347-357. [6] PHINNEY DG, PITTENGER MF. Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells. 2017;35(4):851-858. [7] YAGHOUBI Y, MOVASSAGHPOUR A, ZAMANI M, et al. Human umbilical cord mesenchymal stem cells derived-exosomes in diseases treatment. Life Sci. 2019;233:116733. [8] 刘超,张丽君,陶昊,等.基于细胞生物学方法比较5种不同组织来源间充质干细胞的特征[J].中国组织工程研究,2019,23(33): 5334-5340. [9] OTERO-ORTEGA L, GÓMEZ DE FRUTOS MC, LASO-GARCÍA F, et al. Exosomes promote restoration after an experimental animal model of intracerebral hemorrhage. J Cereb Blood Flow Metab. 2018;38(5):767-779. [10] CAI Y, LIU W, LIAN L, et al. Stroke treatment: Is exosome therapy superior to stem cell therapy. Biochimie. 2020;179:190-204. [11] DUAN S, WANG F, CAO J, et al. Exosomes Derived from MicroRNA-146a-5p-Enriched Bone Marrow Mesenchymal Stem Cells Alleviate Intracerebral Hemorrhage by Inhibiting Neuronal Apoptosis and Microglial M1 Polarization. Drug Des Devel Ther. 2020;14:3143-3158. [12] LI Q, HAN X, LAN X, et al. Inhibition of neuronal ferroptosis protects hemorrhagic brain. JCI Insight. 2017;2(7):e90777. [13] SHOAMANESH A, KATSANOS AH. Combatting Secondary Injury From Intracerebral Hemorrhage With Supplemental Antioxidant Therapy. Stroke. 2021;52(4):1182-1184. [14] CHEN-ROETLING J, LU X, REGAN RF. Targeting heme oxygenase after intracerebral hemorrhage. Ther Targets Neurol Dis. 2015;2(1):474. [15] YIN XP, WU D, ZHOU J, et al. Heme oxygenase 1 plays role of neuron-protection by regulating Nrf2-ARE signaling post intracerebral hemorrhage. Int J Clin Exp Pathol. 2015;8(9):10156-10163. [16] WANG G, YANG Q, LI G, et al. Time course of heme oxygenase-1 and oxidative stress after experimental intracerebral hemorrhage. Acta Neurochir (Wien). 2011;153(2):319-325. [17] FAN X, MU L. The role of heme oxygenase-1 (HO-1) in the regulation of inflammatory reaction, neuronal cell proliferation and apoptosis in rats after intracerebral hemorrhage (ICH). Neuropsychiatr Dis Treat. 2017; 13:77-85. [18] XIAN P, HEI Y, WANG R, et al. Mesenchymal stem cell-derived exosomes as a nanotherapeutic agent for amelioration of inflammation-induced astrocyte alterations in mice. Theranostics. 2019;9(20):5956-5975. [19] 朱东京,鲜盼盼,王甜,等.间充质干细胞外泌体对海马星形胶质细胞活化的抑制作用研究[J].中华细胞与干细胞杂志(电子版), 2021,11(2):99-105. [20] ZHANG Y, WANG WT, GONG CR, et al. Combination of olfactory ensheathing cells and human umbilical cord mesenchymal stem cell-derived exosomes promotes sciatic nerve regeneration. Neural Regen Res. 2020; 15(10): 1903-1911. [21] 陈思铭,胡加伟,李丽丽,等. 两种方法提取人脐带间充质干细胞三维培养生物学特性的比较[J].中国组织工程研究,2022,26(19): 2997-3003. [22] 王涵,刘卫平,龙乾发,等.脐血间充质干细胞外泌体对APP/PS1小鼠海马神经元的保护作用及其机制[J].临床神经外科杂志,2021, 18(3):299-304. [23] JIN P, DENG S, SHERCHAN P, et al. Neurokinin Receptor 1 (NK1R) Antagonist Aprepitant Enhances Hematoma Clearance by Regulating Microglial Polarization via PKC/p38MAPK/NFκB Pathway After Experimental Intracerebral Hemorrhage in Mice. Neurotherapeutics. 2021;18(3):1922-1938. [24] RYNKOWSKI MA, KIM GH, KOMOTAR RJ, et al. A mouse model of intracerebral hemorrhage using autologous blood infusion. Nat Protoc. 2008;3(1):122-128. [25] KARUPPAGOUNDER SS, ALIM I, KHIM SJ, et al. Therapeutic targeting of oxygen-sensing prolyl hydroxylases abrogates ATF4-dependent neuronal death and improves outcomes after brain hemorrhage in several rodent models. Sci Transl Med. 2016;8(328):328ra29. [26] REGAN RF, PANTER SS. Neurotoxicity of hemoglobin in cortical cell culture. Neurosci Lett. 1993;153(2):219-222. [27] WANG T, JIAN Z, BASKYS A, et al. MSC-derived exosomes protect against oxidative stress-induced skin injury via adaptive regulation of the NRF2 defense system. Biomaterials. 2020;257:120264. [28] NAKANO M, FUJIMIYA M. Potential effects of mesenchymal stem cell derived extracellular vesicles and exosomal miRNAs in neurological disorders. Neural Regen Res. 2021;16(12):2359-2366. [29] ZHENG H, ZHANG B, CHHATBAR PY, et al. Mesenchymal Stem Cell Therapy in Stroke: A Systematic Review of Literature in Pre-Clinical and Clinical Research. Cell Transplant. 2018;27(12):1723-1730. [30] HAN Y, SEYFRIED D, MENG Y, et al. Multipotent mesenchymal stromal cell-derived exosomes improve functional recovery after experimental intracerebral hemorrhage in the rat. J Neurosurg. 2018;131(1):290-300. [31] LI M, LI X, WANG D, et al. Inhibition of exosome release augments neuroinflammation following intracerebral hemorrhage. FASEB J. 2021; 35(6):e21617. [32] SCHIPPER HM, SONG W, TAVITIAN A, et al. The sinister face of heme oxygenase-1 in brain aging and disease. Prog Neurobiol. 2019;172:40-70. [33] KANNO H, OZAWA H, DOHI Y, et al. Genetic ablation of transcription repressor Bach1 reduces neural tissue damage and improves locomotor function after spinal cord injury in mice. J Neurotrauma. 2009;26(1): 31-39. [34] WEI CC, KONG YY, LI GQ, et al. Nicotinamide mononucleotide attenuates brain injury after intracerebral hemorrhage by activating Nrf2/HO-1 signaling pathway. Sci Rep. 2017;7(1):717. [35] LIAO YF, ZHU W, LI DP, et al. Heme oxygenase-1 and gut ischemia/reperfusion injury: A short review. World J Gastroenterol. 2013; 19(23): 3555-3561. [36] ZHANG ZF, LIU SM, XIU BH. Research progression about role of hemeoxygenase-1 during brain injuries. Prog Mod Biomed. 2011;11(5): 961-963. [37] LIU XH, WANG XL, XIN H, et al. Induction of Heme Oxygenase-1 by Sodium 9-Hydroxyltanshinone IIA Sulfonate Derivative Contributes to Inhibit LPS-Mediated Inflammatory Response in Macrophages. Cell Physiol Biochem. 2015;36(4):1316-1330. [38] LI Y, JIANG Q, WANG L. Appetite Regulation of TLR4-Induced Inflammatory Signaling. Front Endocrinol (Lausanne). 2021;12:777997. [39] RANZATO E, MARTINOTTI S, PEDRAZZI M, et al. High mobility group box protein-1 in wound repair. Cells. 2012;1(4):699-710. [40] XIONG L, SUN L, ZHANG Y, et al. Exosomes from Bone Marrow Mesenchymal Stem Cells Can Alleviate Early Brain Injury After Subarachnoid Hemorrhage Through miRNA129-5p-HMGB1 Pathway. Stem Cells Dev. 2020;29(4):212-221. |
| [1] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [2] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [3] | Tian Chuan, Zhu Xiangqing, Yang Zailing, Yan Donghai, Li Ye, Wang Yanying, Yang Yukun, He Jie, Lü Guanke, Cai Xuemin, Shu Liping, He Zhixu, Pan Xinghua. Bone marrow mesenchymal stem cells regulate ovarian aging in macaques [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 985-991. |
| [4] | Hou Jingying, Guo Tianzhu, Yu Menglei, Long Huibao, Wu Hao. Hypoxia preconditioning targets and downregulates miR-195 and promotes bone marrow mesenchymal stem cell survival and pro-angiogenic potential by activating MALAT1 [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1005-1011. |
| [5] | Liang Xuezhen, Yang Xi, Li Jiacheng, Luo Di, Xu Bo, Li Gang. Bushen Huoxue capsule regulates osteogenic and adipogenic differentiation of rat bone marrow mesenchymal stem cells via Hedgehog signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1020-1026. |
| [6] | Wen Dandan, Li Qiang, Shen Caiqi, Ji Zhe, Jin Peisheng. Nocardia rubra cell wall skeleton for extemal use improves the viability of adipogenic mesenchymal stem cells and promotes diabetes wound repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1038-1044. |
| [7] | Zhu Bingbing, Deng Jianghua, Chen Jingjing, Mu Xiaoling. Interleukin-8 receptor enhances the migration and adhesion of umbilical cord mesenchymal stem cells to injured endothelium [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1045-1050. |
| [8] | Fang Xiaolei, Leng Jun, Zhang Chen, Liu Huimin, Guo Wen. Systematic evaluation of different therapeutic effects of mesenchymal stem cell transplantation in the treatment of ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1085-1092. |
| [9] | Guo Jia, Ding Qionghua, Liu Ze, Lü Siyi, Zhou Quancheng, Gao Yuhua, Bai Chunyu. Biological characteristics and immunoregulation of exosomes derived from mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1093-1101. |
| [10] | Wu Weiyue, Guo Xiaodong, Bao Chongyun. Application of engineered exosomes in bone repair and regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1102-1106. |
| [11] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [12] | Huang Chuanjun, Zou Yu, Zhou Xiaoting, Zhu Yangqing, Qian Wei, Zhang Wei, Liu Xing. Transplantation of umbilical cord mesenchymal stem cells encapsulated in RADA16-BDNF hydrogel promotes neurological recovery in an intracerebral hemorrhage rat model [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 510-515. |
| [13] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [14] | Lu Dongdong, Zhu Tianfeng, Zhang Yijian, Zhao Zhijian, Liu Yang, Shen Xu, Zhu Xuesong. 3D bio-printing methylacrylated gelatin hydrogel scaffolds promote the repair of subchondral bone defects [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(34): 5454-5460. |
| [15] | Li Maoxue, Ding Yi, Guo Shujuan. Understanding of periodontal biomaterials based on the concept of bone homeostasis control and the effects on bone formation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(34): 5562-5568. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||