[1] EINHORN TA, GERSTENFELD LC. Fracture healing: mechanisms and interventions. Nat Rev Rheumatol. 2015;11(1):45-54.
[2] RAVI P, NAGESWARAN J, RAMANUJAM M, et al. Correlation between traumatic brain injuries and callusformation in long bone fractures. Indian J Orthop. 2022; 56(5):837-846.
[3] TSITSILONIS S, SEEMANN R, MISCH M, et al. The effect of traumatic brain injury on bone healing: an experimental study in a novel in vivo animal model. Injury. 2015;46(4):661-665.
[4] BRADY RD, GRILLS BL, CHURCH JE, et al. Closed head experimental traumatic brain injury increases size and bone volume of callus in mice with concomitant tibial fracture. Sci Rep. 2016;6:34491.
[5] RUSSO MV, MCGAVERN DB. Inflammatory neuroprotection following traumatic brain injury. Science. 2016;353(6301):783-785.
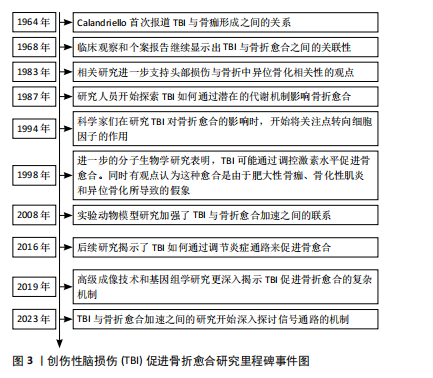
[6] CALANDRIELLO B. Callus formation in severe brain injuries. Bull Hosp Joint Dis. 1964;25:170-175.
[7] ROBERTS PH. Heterotopic ossification complicating paralysis of intracranial origin. J Bone Joint Surg Br. 1968;50-B(1):70-77.
[8] GARLAND DE, DOWLING V. Forearm fractures in the head-injured adult. Clin Orthop Relat Res. 1983;(176):190-196.
[9] NEWMAN RJ, STONE MH, MUKHERJEE SK. Accelerated fracture union in association with severe head injury. Injury. 1987;18(4):241-246.
[10] WILDBURGER R, ZARKOVIC N, EGGER G, et al. Basic fibroblast growth factor (BFGF) immunoreactivity as a possible link between head injury and impaired bone fracture healing. Bone Miner. 1994;27(3):183-192.
[11] WILDBURGER R, ZARKOVIC N, TONKOVIC G, et al. Post-traumatic hormonal disturbances: prolactin as a link between head injury and enhanced osteogenesis. J Endocrinol Invest. 1998;21(2):78-86.
[12] KUSHWAHA VP, GARLAND DG. Extremity fractures in the patient with a traumatic brain injury. J Am Acad Orthop Surg. 1998;6(5):298-307.
[13] WEI Y, WANG L, CLARK JC, et al. Elevated leptin expression in a rat model of fracture and traumatic brain injury. J Pharm Pharmacol. 2008;60(12):1667-1672.
[14] SHIM DW, HONG H, CHO KC, et al. Accelerated tibia fracture healing in traumatic brain injury in accordance with increased hematoma formation. BMC Musculoskelet Disord. 2022;23(1):1110.
[15] 韩立功,刘林,陈天成,等.脑外伤合并尺骨骨折家兔血清花生四烯酸、环氧二碳三烯酸的变化及对骨折愈合的影响[J].徐州医科大学学报,2017,37(7): 448-451.
[16] CORREALE J, VILLA A. The neuroprotective role of inflammation in nervous system injuries. J Neurol. 2004;251(11):1304-1316.
[17] CRUPI R, CORDARO M, CUZZOCREA S, et al. Management of traumatic brain injury: from present to future. Antioxidants (Basel). 2020;9(4):297.
[18] CALIS Z, MOGULKOC R, BALTACI AK. The roles of flavonols/flavonoids in neurodegeneration and neuroinflammation. Mini rev med chem. 2020;20(15): 1475-1488.
[19] SIMS NA. Cell-specific paracrine actions of IL-6 family cytokines from bone, marrow and muscle that control bone formation and resorption. Int J Biochem Cell Biol. 2016;79:14-23.
[20] CIARAMELLA A, DELLA VEDOVA C, SALANI F, et al. Increased levels of serum IL-18 are associated with the long-term outcome of severe traumatic brain injury. Neuroimmunomodulation. 2014;21(1):8-12.
[21] ZHANG E, MIRAMINI S, PATEL M, et al. Role of TNF-α in early-stage fracture healing under normal and diabetic conditions. Comput Methods Programs Biomed. 2022;213:106536.
[22] SUN M, BRADY RD, WRIGHT DK, et al. Treatment with an interleukin-1 receptor antagonist mitigates neuroinflammation and brain damage after polytrauma. Brain Behav Immun. 2017;66:359-371.
[23] SHULTZ SR, SUN M, WRIGHT DK, et al. Tibial fracture exacerbates traumatic brain injury outcomes and neuroinflammation in a novel mouse model of multitrauma. J Cereb Blood Flow Metab. 2015;35(8):1339-1347.
[24] JUNGNER M, SIEMUND R, VENTUROLI D, et al. Blood-brain barrier permeability following traumatic brain injury. Minerva Anestesiol. 2016;82(5):525-533.
[25] BAJWA NM, KESAVAN C, MOHAN S. Long-term consequences of traumatic brain injury in bone metabolism. Front Neurol. 2018;9:115.
[26] ALLURI H, WIGGINS-DOHLVIK K, DAVIS ML, et al. Blood-brain barrier dysfunction following traumatic brain injury. Metab Brain Dis. 2015;30(5):1093-1104.
[27] AURORA R, SILVA MJ. T cells heal bone fractures with help from the gut microbiome. J Clin Invest. 2023;133(8):e167311.
[28] MARSELL R, EINHORN TA. The biology of fracture healing. Injury. 2011;42(6):551-555.
[29] SALHOTRA A, SHAH HN, LEVI B, et al. Mechanisms of bone development and repair. Nat Rev Mol Cell Biol. 2020;21(11):696-711.
[30] SMITH É, COMISKEY C, CARROLL Á. Prevalence of and risk factors for osteoporosis in adults with acquired brain injury. Ir J Med Sci. 2016;185(2):473-481.
[31] BANHAM-HALL N, KOTHWAL K, PIPKIN J, et al. Prevalence of low bone mineral density in inpatients with traumatic brain injury receiving neurobehavioural rehabilitation: a postoperative, observational study. Physiotherapy. 2013;99(4): 328-334.
[32] YU H, WATT H, MOHAN S. The negative impact of traumatic brain injury (TBI) on bone in a mouse model. Brain Inj. 2014;28(2):244-251.
[33] BRADY RD, SHULTZ SR, SUN M, et al. Experimental Traumatic Brain Injury Induces Bone Loss in Rats. J Neurotrauma. 2016;33(23):2154-2160.
[34] YU H, WERGEDAL JE, RUNDLE CH, et al. Reduced bone mass accrual in mouse model of repetitive mild traumatic brain injury. J Rehabil Res Dev. 2014;51(9): 1427-1437.
[35] CHEN CH, GAN D, YANG CS, et al. Discussion on bone healing rate and expression of cytokines and growth factors in rat models with simple fracture and brain injury. J King Saud Univ Sci. 2020;32(4):2439-2444.
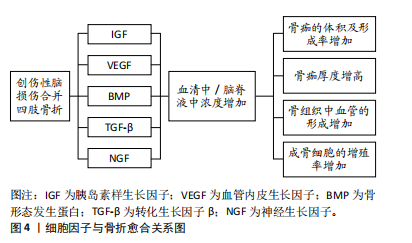
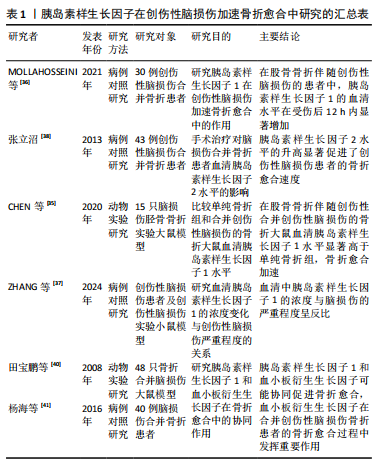
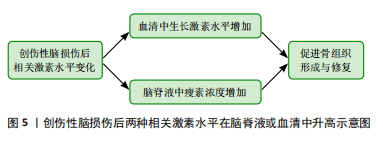
[36] MOLLAHOSSEINI M, AHMADIRAD H, GOUJANI R, et al. The association between traumatic brain injury and accelerated fracture healing: a study on the effects of growth factors and cytokines. J Mol Neurosci. 2021;71(1):162-168.
[37] ZHANG Z, WU X, KONG Y, et al. Dynamic changes and effects of H(2)S, IGF-1, and GH in the traumatic brain injury. Biochem Genet. 2024;62(5):3821-3840.
[38] 张立沼.手术治疗对脑外伤合并骨折患者血清胰岛素样生长因子Ⅱ水平的影响[J].中国老年学杂志,2013,33(24):6310-6311.
[39] 郑少涛,林喜容,周少鹏.脑外伤合并骨折患者血清胰岛素生长因子Ⅱ水平的变化[J].中国现代医生,2014,52(2):19-20.
[40] 田宝鹏,陈雯辉,潘海涛,等.脑外伤后胰岛素样生长因子Ⅰ及血小板衍生生长因子对骨折愈合的影响[J].首都医科大学学报,2008,29(1):69-73.
[41] 杨海,董金波,王维山,等.PDGF-BB在脑外伤合并骨折患者血液中的表达及临床意义[J].系统医学,2016,1(11):7-10.
[42] 唐生平,廖世杰,黄乾,等.骨H型血管生成机制及影响因素的研究现状[J].中国矫形外科杂志,2024,32(6):525-529.
[43] JAHN D, KNAPSTEIN PR, OTTO E, et al. Increased β(2)-adrenergic signaling promotes fracture healing through callus neovascularization in mice. Sci Transl Med. 2024;16(743):eadk9129.
[44] 季卫锋,杨成贵,肖鲁伟.补肾助阳中药与合并脑外伤骨折加速愈合分子机制的研究[J].中华中医药学刊,2015,33(7):1570-1573.
[45] ZHANG R, LIANG Y, WEI S. The expressions of NGF and VEGF in the fracture tissues are closely associated with accelerated clavicle fracture healing in patients with traumatic brain injury. Ther Clin Risk Manag. 2018;14:2315-2322.
[46] 段世博,刘永杰,王志峰,等.血管内皮生长因子在骨折伴颅脑损伤患者血清中的表达[J].世界最新医学信息文摘,2018,18(34):132-133.
[47] DING W, JI R, YAO S, et al. Hu’po Anshen decoction promotes fracture healing in mice with traumatic brain injury through BMP2-COX2-ATF4 signaling pathway. FASEB J. 2023;37(6):e22952.
[48] GAUTSCHI OP, TOFFOLI AM, JOESBURY KA, et al. Osteoinductive effect of cerebrospinal fluid from brain-injured patients. J Neurotrauma. 2007;24(1):154-162.
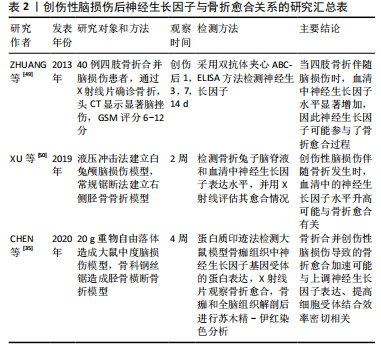
[49] ZHUANG YF, LI J. Serum EGF and NGF levels of patients with brain injury and limb fracture. Asian Pac J Trop Med. 2013;6(5):383-386.
[50] XU YQ, QIN ML, FENG SY, et al. Expressions and significance of calcitonin gene-related peptide and nerve growth factor in rabbit model of traumatic brain injury complicated with tibial fracture: preliminary results. Eur Rev Med Pharmacol Sci. 2019;23(12):5040-5050.
[51] Yang S, Cheng J, Man C, et al. Effects of exogenous nerve growth factor on the expression of BMP-9 and VEGF in the healing of rabbit mandible fracture with local nerve injury. J Orthop Surg Res. 2021;16(1):74.
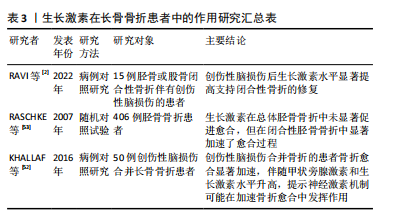
[52] KHALLAF FG, KEHINDE EO, HUSSEIN S. Bone healing and hormonal bioassay in patients with long-bone fractures and concomitant head injury. Med Princ Pract. 2016;25(4):336-342.
[53] RASCHKE M, RASMUSSEN MH, GOVENDER S, et al. Effects of growth hormone in patients with tibial fracture: a randomised, double-blind, placebo-controlled clinical trial. Eur J Endocrinol. 2007;156(3):341-351.
[54] ZHANG C, DENG K, GUO Y, et al. Research progress of correlation between traumatic brain injury and fracture healing. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31(7):885-889.
[55] YAN H, ZHANG HW, FU P, et al. Leptin’s effect on accelerated fracture healing after traumatic brain injury. Neurol Res. 2013;35(5):537-544.
[56] WANG L, SUN S, YANG L, et al. Effects of leptin on femoral fracture in rats. J Biomed Res. 2018;32(2):130-135.
[57] GARBE A, GRAEF F, APPELT J, et al. Leptin mediated pathways stabilize posttraumatic insulin and osteocalcin patterns after long bone fracture and concomitant traumatic brain injury and thus influence fracture healing in a combined murine trauma model. Int J Mol Sci. 2020;21(23):9144.
[58] GRAEF F, SEEMANN R, GARBE A, et al. Impaired fracture healing with high non-union rates remains irreversible after traumatic brain injury in leptin-deficient mice. J Musculoskelet Neuronal Interact. 2017;17(2):78-85.
[59] SEEMANN R, GRAEF F, GARBE A, et al. Leptin-deficiency eradicates the positive effect of traumatic brain injury on bone healing: histological analyses in a combined trauma mouse model. J Musculoskelet Neuronal Interact. 2018; 18(1):32-41.
[60] 李祥泽,卜宪敏,李冬梅,等.创伤性脑外伤促进骨折愈合中的干细胞、细胞因子、激素、神经肽及基因[J].中国组织工程研究,2021,25(19):3057-3063.
[61] XU J, WANG J, CHEN X, et al. The effects of calcitonin gene-related peptide on bone homeostasis and regeneration. Curr Osteoporos Rep. 2020;18(6):621-632.
[62] PARKER RS, NAZZAL MK, MORRIS AJ, et al. Role of the neurologic system in fracture healing: an extensive review. Curr Osteoporos Rep. 2024;22(1):205-216.
[63] APPELT J, BARANOWSKY A, JAHN D, et al. The neuropeptide calcitonin gene-related peptide alpha is essential for bone healing. EBioMedicine. 2020;59:102970.
[64] SONG Y, HAN GX, CHEN L, et al. The role of the hippocampus and the function of calcitonin gene-related peptide in the mechanism of traumatic brain injury accelerating fracture-healing. Eur Rev Med Pharmacol Sci. 2017;21(7):1522-1531.
[65] 孙东良,陈通,付爱军,等.颅脑损伤合并股骨闭合性骨折大鼠模型的建立及骨痂中降钙素基因相关肽的表达及意义[J].中国煤炭工业医学杂志, 2014,17(7):1123-1126.
[66] NIEDERMAIR T, STRAUB RH, BROCHHAUSEN C, et al. Impact of the sensory and sympathetic nervous system on fracture healing in ovariectomized mice. Int J Mol Sci. 2020;21(2):405.
[67] LIU WJ, CHEN W, XIE M, et al. Traumatic brain injury stimulates sympathetic tone-mediated bone marrow myelopoiesis to favor fracture healing. Signal Transduct Target Ther. 2023;8(1):260.
[68] ZHONG L, WANG J, WANG P, et al. Neural stem cell-derived exosomes and regeneration: cell-free therapeutic strategies for traumatic brain injury. Stem Cell Res Ther. 2023;14(1):198.
[69] 苏友祥,李志超,管华鹏,等.外泌体非编码RNA调控骨折愈合机理的研究进展[J].中国矫形外科杂志,2023,31(24):2260-2263, 2269.
[70] LIN Z, XIONG Y, SUN Y, et al. Circulating miRNA-21-enriched extracellular vesicles promote bone remodeling in traumatic brain injury patients. Exp Mol Med. 2023;55(3):587-596.
[71] HAN Z, SHI F, CHEN Y, et al. Relationship between miRNA-433 and SPP1 in the presence of fracture and traumatic brain injury. Exp Ther Med. 2021;22(3):928.
[72] HU L, LIU J, XUE H, et al. miRNA-92a-3p regulates osteoblast differentiation in patients with concomitant limb fractures and tbi via IBSP/PI3K-AKT inhibition. Mol Ther Nucleic Acids. 2021;23:1345-1359.
[73] SUN Y, XIONG Y, YAN C, et al. Downregulation of microRNA-16-5p accelerates fracture healing by promoting proliferation and inhibiting apoptosis of osteoblasts in patients with traumatic brain injury. Am J Transl Res. 2019;11(8):4746-4760.
[74] XIONG Y, CAO F, HU L, et al. MiRNA-26a-5p accelerates healing via downregulation of PTEN in fracture patients with traumatic brain injury. Mol Ther Nucleic Acids. 2019;17:223-234.
[75] YU G, SHEN P, LEE YC, et al. Multiple pathways coordinating reprogramming of endothelial cells into osteoblasts by BMP4. iScience. 2021;24(4):102388.
[76] GUO GN, GOU YJ, JIANG XY, et al. Long non-coding RNAs in traumatic brain injury accelerated fracture healing. Front Surg. 2021;8:663377.
[77] 高思淼,韩雪,吴晓光,等.电针联合低频经颅超声刺激对创伤性脑损伤大鼠脑电信号的影响[J].中国组织工程研究,2025,29(2):402-408.
[78] AHMED A I, SHTAYA A, ZABEN M, et al. Activation of endogenous neural stem cells after traumatic brain injury. The Lancet. 2014,383(140-6736):S18.
[79] KRUMINA G, BABARYKIN D, KRUMINA Z, et al. Effects of systemically transplanted allogeneic bone marrow multipotent mesenchymal stromal cells on rats’ recovery after experimental polytrauma. J Trauma Acute Care Surg. 2013;74(3):785-791.
[80] LEI SH, GUO L, YUE HY, et al. Marrow stromal stem cell autologous transplantation in denervated fracture healing: an experimental study in rats. Orthop Surg. 2013; 5(4):280-288.
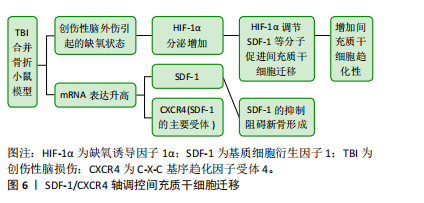
[81] LIU XQ, ZHOU CL, LI YJ, et al. SDF-1 Promotes endochondral bone repair during fracture healing at the traumatic brain injury condition. PLoS One. 2013;8(1): e54077.
[82] XUE YH, LI ZK, WANG Y, et al. Role of the HIF-1α/SDF-1/CXCR4 signaling axis in accelerated fracture healing after craniocerebral injury. Mol Med Rep. 2020; 22(4):2767-2774.
[83] ZHANG L, JIAO G, REN S, et al. Exosomes from bone marrow mesenchymal stem cells enhance fracture healing through the promotion of osteogenesis and angiogenesis in a rat model of nonunion. Stem Cell Res Ther. 2020;11(1):38. |