[1] KANIS JA, MELTON LR, CHRISTIANSEN C, et al. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9(8):1137-1141.
[2] GIANGREGORIO LM, PAPAIOANNOU A, MACINTYRE NJ, et al. Too Fit To Fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int. 2014;25(3):821-835.
[3] LEBOFF MS, GREENSPAN SL, INSOGNA KL, et al. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022; 33(10):2049-2102.
[4] 中华医学会骨质疏松和骨矿盐疾病分会. 原发性骨质疏松症诊疗指南(2022)[J]. 中华骨质疏松和骨矿盐疾病杂志,2022,15(6): 573-611.
[5] 章振林, 岳华, 李梅, 等. 中国《原发性骨质疏松症诊疗指南(2022版)》要点解读[J]. 诊断学理论与实践,2023,22(3):230-233.
[6] COMPSTON JE, MCCLUNG MR, LESLIE WD. Osteoporosis. Lancet. 2019; 393(10169):364-376.
[7] REID IR, BILLINGTON EO. Drug therapy for osteoporosis in older adults. Lancet. 2022;399(10329):1080-1092.
[8] KENDLER DL, COSMAN F, STAD RK, et al. Denosumab in the Treatment of Osteoporosis: 10 Years Later: A Narrative Review. Adv Ther. 2022; 39(1):58-74.
[9] LIANG B, BURLEY G, LIN S, et al. Osteoporosis pathogenesis and treatment: existing and emerging avenues. Cell Mol Biol Lett. 2022; 27(1):72.
[10] CREMERS S, DRAKE MT, EBETINO FH, et al. Pharmacology of bisphosphonates. Br J Clin Pharmacol. 2019;85(6):1052-1062.
[11] DEEKS ED. Denosumab: A Review in Postmenopausal Osteoporosis. Drugs Aging. 2018;35(2):163-173.
[12] LI J, CAO F, YIN HL, et al. Ferroptosis: past, present and future. Cell Death Dis. 2020;11(2):88.
[13] ZOU DB, MOU Z, WU W, et al. TRIM33 protects osteoblasts from oxidative stress-induced apoptosis in osteoporosis by inhibiting FOXO3a ubiquitylation and degradation. Aging Cell. 2021;20(7):e13367.
[14] YOSHIDA G, KAWABATA T, TAKAMATSU H, et al. Degradation of the NOTCH intracellular domain by elevated autophagy in osteoblasts promotes osteoblast differentiation and alleviates osteoporosis. Autophagy. 2022;18(10):2323-2332.
[15] TAO Z, WANG J, WEN K, et al. Pyroptosis in Osteoblasts: A Novel Hypothesis Underlying the Pathogenesis of Osteoporosis. Front Endocrinol (Lausanne). 2020;11:548812.
[16] KETELUT-CARNEIRO N, FITZGERALD KA. Apoptosis, Pyroptosis, and Necroptosis-Oh My! The Many Ways a Cell Can Die. J Mol Biol. 2022; 434(4):167378.
[17] CHEN L, MIN J, WANG F. Copper homeostasis and cuproptosis in health and disease. Signal Transduct Target Ther. 2022;7(1):378.
[18] LIU S, YAO S, YANG H, et al. Autophagy: Regulator of cell death. Cell Death Dis. 2023;14(10):648.
[19] YU P, ZHANG X, LIU N, et al. Pyroptosis: mechanisms and diseases. Signal Transduct Target Ther. 2021;6(1):128.
[20] WANG X, ZHOU Y, MIN J, et al. Zooming in and out of ferroptosis in human disease. Front Med. 2023;17(2):173-206.
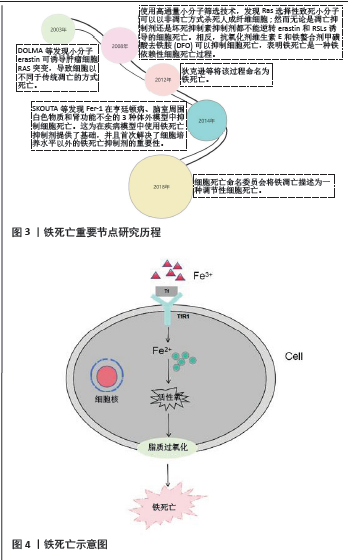
[21] DOLMA S, LESSNICK SL, HAHN WC, et al. Identification of genotype-selective antitumor agents using synthetic lethal chemical screening in engineered human tumor cells. Cancer Cell. 2003;3(3):285-296.
[22] DIXON SJ, LEMBERG KM, LAMPRECHT MR, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5): 1060-1072.
[23] SKOUTA R, DIXON SJ, WANG J, et al. Ferrostatins inhibit oxidative lipid damage and cell death in diverse disease models. J Am Chem Soc. 2014;136(12):4551-4556.
[24] GALLUZZI L, VITALE I, AARONSON SA, et al. Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018;25(3):486-541.
[25] YANG WS, STOCKWELL BR. Synthetic lethal screening identifies compounds activating iron-dependent, nonapoptotic cell death in oncogenic-RAS-harboring cancer cells. Chem Biol. 2008;15(3):234-245.
[26] JIANG X, STOCKWELL BR, CONRAD M. Ferroptosis: mechanisms, biology and role in disease. Nat Rev Mol Cell Biol. 2021;22(4):266-282.
[27] YU H, GUO P, XIE X, et al. Ferroptosis, a new form of cell death, and its relationships with tumourous diseases. J Cell Mol Med. 2017;21(4): 648-657.
[28] XIE Y, SONG X, SUN X, et al. Identification of baicalein as a ferroptosis inhibitor by natural product library screening. Biochem Biophys Res Commun. 2016;473(4):775-780.
[29] HAN C, LIU Y, DAI R, et al. Ferroptosis and Its Potential Role in Human Diseases. Front Pharmacol. 2020;11:239.
[30] LIANG C, ZHANG X, YANG M, et al. Recent Progress in Ferroptosis Inducers for Cancer Therapy. Adv Mater. 2019;31(51):e1904197.
[31] TANG D, CHEN X, KANG R, et al. Ferroptosis: molecular mechanisms and health implications. Cell Res. 2021;31(2):107-125.
[32] CHEN X, LI J, KANG R, et al. Ferroptosis: machinery and regulation. Autophagy. 2021;17(9):2054-2081.
[33] GAO Z, CHEN Z, XIONG Z, et al. Ferroptosis - A new target of osteoporosis. Exp Gerontol. 2022;165:111836.
[34] SU Y, ZHAO B, ZHOU L, et al. Ferroptosis, a novel pharmacological mechanism of anti-cancer drugs. Cancer Lett. 2020;483:127-136.
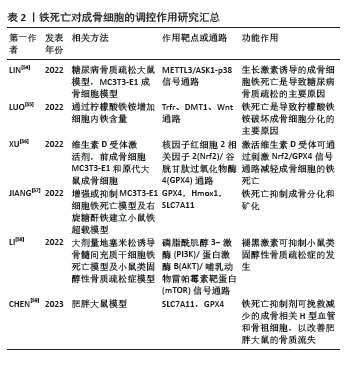
[35] GALY B, CONRAD M, MUCKENTHALER M. Mechanisms controlling cellular and systemic iron homeostasis. Nat Rev Mol Cell Biol. 2024; 25(2):133-155.
[36] WALLACE DF. The Regulation of Iron Absorption and Homeostasis. Clin Biochem Rev. 2016;37(2):51-62.
[37] MAO C, LIU X, ZHANG Y, et al. DHODH-mediated ferroptosis defence is a targetable vulnerability in cancer. Nature. 2021;593(7860):586-590.
[38] SAWICKI KT, De JESUS A, ARDEHALI H. Iron Metabolism in Cardiovascular Disease: Physiology, Mechanisms, and Therapeutic Targets. Circ Res. 2023;132(3):379-396.
[39] BROWN CW, AMANTE JJ, CHHOY P, et al. Prominin2 Drives Ferroptosis Resistance by Stimulating Iron Export. Dev Cell. 2019; 51(5):575-586.
[40] FRIEDMANN AJ, SCHNEIDER M, PRONETH B, et al. Inactivation of the ferroptosis regulator Gpx4 triggers acute renal failure in mice. Nat Cell Biol. 2014;16(12):1180-1191.
[41] HAEGGSTROM JZ, FUNK CD. Lipoxygenase and leukotriene pathways: biochemistry, biology, and roles in disease. Chem Rev. 2011;111(10): 5866-5898.
[42] SHAH R, SHCHEPINOV MS, PRATT DA. Resolving the Role of Lipoxygenases in the Initiation and Execution of Ferroptosis. ACS Cent Sci. 2018;4(3):387-396.
[43] LI S, HUANG Y. Ferroptosis: an iron-dependent cell death form linking metabolism, diseases, immune cell and targeted therapy. Clin Transl Oncol. 2022;24(1):1-12.
[44] ITO F, SONO Y, ITO T. Measurement and Clinical Significance of Lipid Peroxidation as a Biomarker of Oxidative Stress: Oxidative Stress in Diabetes, Atherosclerosis, and Chronic Inflammation. Antioxidants (Basel). 2019;8(3):72.
[45] LIU P, WANG W, LI Z, et al. Ferroptosis: A New Regulatory Mechanism in Osteoporosis. Oxid Med Cell Longev. 2022;2022:2634431.
[46] GAO M, ZHANG Z, SUN J, et al. The roles of circRNA-miRNA-mRNA networks in the development and treatment of osteoporosis. Front Endocrinol (Lausanne). 2022;13:945310.
[47] BALLHAUSE T M, JIANG S, BARANOWSKY A, et al. Relevance of Notch Signaling for Bone Metabolism and Regeneration. Int J Mol Sci. 2021; 22(3):1325.
[48] MAJIDINIA M, SADEGHPOUR A, YOUSEFI B. The roles of signaling pathways in bone repair and regeneration. J Cell Physiol. 2018;233(4): 2937-2948.
[49] LI Y, FENG C, GAO M, et al. MicroRNA-92b-5p modulates melatonin-mediated osteogenic differentiation of bone marrow mesenchymal stem cells by targeting ICAM-1. J Cell Mol Med. 2019;23(9):6140-6153.
[50] LI Y, YANG F, GAO M, et al. miR-149-3p Regulates the Switch between Adipogenic and Osteogenic Differentiation of BMSCs by Targeting FTO. Mol Ther Nucleic Acids. 2019;17:590-600.
[51] PONZETTI M, RUCCI N. Osteoblast Differentiation and Signaling: Established Concepts and Emerging Topics. Int J Mol Sci. 2021;22(13): 6651.
[52] KIM JM, LIN C, STAVRE Z, et al. Osteoblast-Osteoclast Communication and Bone Homeostasis. Cells. 2020;9(9):2073.
[53] ZHANG H, WANG A, LI G, et al. Osteoporotic bone loss from excess iron accumulation is driven by NOX4-triggered ferroptosis in osteoblasts. Free Radic Biol Med. 2023;198:123-136.
[54] LIN Y, SHEN X, KE Y, et al. Activation of osteoblast ferroptosis via the METTL3/ASK1-p38 signaling pathway in high glucose and high fat (HGHF)-induced diabetic bone loss. FASEB J. 2022;36(3):e22147.
[55] LUO C, XU W, TANG X, et al. Canonical Wnt signaling works downstream of iron overload to prevent ferroptosis from damaging osteoblast differentiation. Free Radic Biol Med. 2022;188:337-350.
[56] XU P, LIN B, DENG X, et al. VDR activation attenuates osteoblastic ferroptosis and senescence by stimulating the Nrf2/GPX4 pathway in age-related osteoporosis. Free Radic Biol Med. 2022;193(Pt 2):720-735.
[57] JIANG Z, WANG H, QI G, et al. Iron overload-induced ferroptosis of osteoblasts inhibits osteogenesis and promotes osteoporosis: An in vitro and in vivo study. IUBMB Life. 2022;74(11):1052-1069.
[58] LI M, YANG N, HAO L, et al. Melatonin Inhibits the Ferroptosis Pathway in Rat Bone Marrow Mesenchymal Stem Cells by Activating the PI3K/AKT/mTOR Signaling Axis to Attenuate Steroid-Induced Osteoporosis. Oxid Med Cell Longev. 2022;2022:8223737.
[59] CHEN X, LIU C, YU R, et al. Interaction between ferroptosis and TNF-alpha: Impact in obesity-related osteoporosis. FASEB J. 2023;37(6): e22947.
[60] MOON YJ, ZHANG Z, BANG IH, et al. Sirtuin 6 in preosteoclasts suppresses age- and estrogen deficiency-related bone loss by stabilizing estrogen receptor alpha. Cell Death Differ. 2019;26(11):2358-2370.
[61] LAN C, ZHOU X, SHEN X, et al. Suppression of IRF9 Promotes Osteoclast Differentiation by Decreased Ferroptosis via STAT3 Activation. Inflammation. 2024;47(1):99-113.
[62] NI S, YUAN Y, QIAN Z, et al. Hypoxia inhibits RANKL-induced ferritinophagy and protects osteoclasts from ferroptosis. Free Radic Biol Med. 2021;169:271-282.
[63] XUE C, LUO H, WANG L, et al. Aconine attenuates osteoclast-mediated bone resorption and ferroptosis to improve osteoporosis via inhibiting NF-kappaB signaling. Front Endocrinol (Lausanne). 2023;14:1234563.
[64] JIN Y, WU S, ZHANG L, et al. Artesunate inhibits osteoclast differentiation by inducing ferroptosis and prevents iron overload-induced bone loss. Basic Clin Pharmacol Toxicol, 2023;132(2):144-153.
[65] QU X, SUN Z, WANG Y, et al. Zoledronic acid promotes osteoclasts ferroptosis by inhibiting FBXO9-mediated p53 ubiquitination and degradation. PeerJ. 2021;9:e12510.
[66] ZHANG J, ZHANG L, YAO G, et al. NRF2 is essential for iron-overload stimulated osteoclast differentiation through regulation of redox and iron homeostasis. Cell Biol Toxicol. 2023;39(6):3305-3321.
[67] WANG X, MA H, SUN J, et al. Mitochondrial Ferritin Deficiency Promotes Osteoblastic Ferroptosis Via Mitophagy in Type 2 Diabetic Osteoporosis. Biol Trace Elem Res. 2022;200(1):298-307.
[68] WU D, WEN X, LIU W, et al. Comparison of the effects of deferasirox, deferoxamine, and combination of deferasirox and deferoxamine on an aplastic anemia mouse model complicated with iron overload. Drug Des Devel Ther. 2018;12:1081-1091. |