[1] 吴钒,黄朝靖,邱伟,等.骨质疏松椎体压缩性骨折椎体成形术后伤椎再塌陷的研究进展[J].中国中医骨伤科杂志,2023,31(8):78-81.
[2] SZKODA-POLISZUK K, ZAŁUSKI R. A Comparative Biomechanical Analysis of the Impact of Different Configurations of Pedicle-Screw-Based Fixation in Thoracolumbar Compression Fracture. Appl Bionics Biomech. 2022;2022:3817097.
[3] LUO Y, JIANG T, GUO H, et al. Osteoporotic vertebral compression fracture accompanied with thoracolumbar fascial injury: risk factors and the association with residual pain after percutaneous vertebroplasty. BMC Musculoskelet Disord. 2022;23(1):343.
[4] ZHANG W, LIU S, LIU X, et al. Unilateral percutaneous vertebroplasty for osteoporotic lumbar compression fractures: a comparative study between transverse process root-pedicle approach and conventional transpedicular approach. J Orthop Surg Res. 2021;16(1):73.
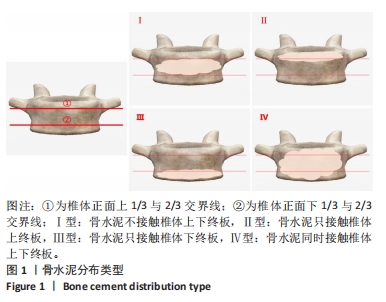
[5] BAO LS, WU W, ZHONG XH, et al. [Effect of bone cement distribution on the clinical outcome of unilateral transpedicular puncture for spinal osteoporotic fractures]. Zhongguo Gu Shang. 2022;35(5):423-429.
[6] WEI Y, BASKARAN N, WANG HY, et al. Study of polymethylmethacrylate/tricalcium silicate composite cement for orthopedic application. Biomed J. 2023;46(3):100540.
[7] MIAO F, ZENG X, WANG W, et al. Percutaneous vertebroplasty with high- versus low-viscosity bone cement for osteoporotic vertebral compression fractures. J Orthop Surg Res. 2020;15(1):302.
[8] 徐敏,张鸿升,王继,等.高黏度与低黏度骨水泥经皮椎体成形治疗骨质疏松椎体压缩性骨折的Meta分析[J].中国组织工程研究, 2017,21(34):5571-5576.
[9] LAI PL, CHEN LH, CHEN WJ, et al. Chemical and physical properties of bone cement for vertebroplasty. Biomed J. 2013;36(4):162-167.
[10] MOLLOY S, RILEY LH 3RD, BELKOFF SM. Effect of cement volume and placement on mechanical-property restoration resulting from vertebroplasty. AJNR Am J Neuroradiol. 2005;26(2):401-404.
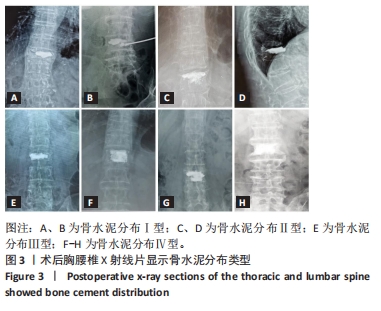
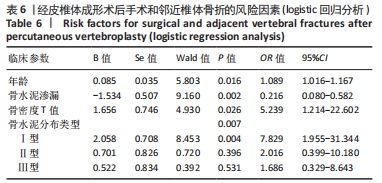
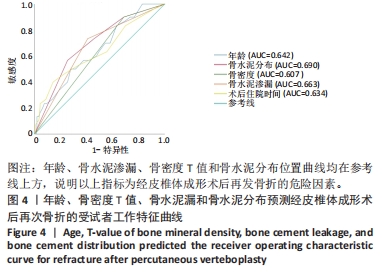
[11] 阿卜杜吾普尔·海比尔,阿里木江·玉素甫,麦麦提敏·阿卜力米提,等.经皮椎体成形术后骨水泥量和分布对手术椎体及邻近椎体再发骨折的影响[J].中国组织工程研究,2024,28(10):1586-1591.
[12] JU G, LIU X. A nomogram prediction model for refracture in elderly patients with osteoporotic vertebral compression fractures after percutaneous vertebroplasty. Eur Spine J. 2023;32(11):3919-3926.
[13] LIANG L, CHEN X, JIANG W, et al. Balloon kyphoplasty or percutaneous vertebroplasty for osteoporotic vertebral compression fracture? An updated systematic review and meta-analysis. Ann Saudi Med. 2016;36(3):165-174.
[14] YU W, XU W, JIANG X, et al. Risk Factors for Recollapse of the Augmented Vertebrae After Percutaneous Vertebral Augmentation: A Systematic Review and Meta-Analysis. World Neurosurg. 2018;111: 119-129.
[15] KWEH BTS, LEE HQ, TAN T, et al. The Role of Spinal Orthoses in Osteoporotic Vertebral Fractures of the Elderly Population (Age 60 Years or Older): Systematic Review. Global Spine J. 2021;11(6):975-987.
[16] NIU J, ZHOU H, MENG Q, et al. Factors affecting recompression of augmented vertebrae after successful percutaneous balloon kyphoplasty: a retrospective analysis. Acta radiol. 2015;56(11): 1380-1387.
[17] ZHANG L, WANG Q, WANG L, et al. Bone cement distribution in the vertebral body affects chances of recompression after percutaneous vertebroplasty treatment in elderly patients with osteoporotic vertebral compression fractures. Clin Interv Aging. 2017;12:431-436.
[18] HAIBIER A, YUSUFU A, LIN H, et al. Effect of different cement distribution in bilateral and unilateral Percutaneous vertebro plasty on the clinical efficacy of vertebral compression fractures. BMC Musculoskelet Disord. 2023;24(1):908.
[19] LIANG X, ZHONG W, LUO X, et al. Risk factors of adjacent segmental fractures when percutaneous vertebroplasty is performed for the treatment of osteoporotic thoracolumbar fractures. Sci Rep. 2020; 10(1):399.
[20] ZHANG Z, FAN J, DING Q, et al. Risk factors for new osteoporotic vertebral compression fractures after vertebroplasty: a systematic review and meta-analysis. J Spinal Disord Tech. 2013;26(4):E150-157.
[21] 吕文,刘艺明,陈光,等.经横突根部单侧穿刺的改良PVP与PCVP技术治疗腰椎骨质疏松性骨折的疗效对比[J].颈腰痛杂志, 2020,41(2):154-157.
[22] 崔志远,毛兆虎,刘玉林,等.单侧PVP术对OVCF术后椎体高度恢复及疼痛程度的效果研究[J].中国医药导报,2021,18(18):92-95.
[23] 罗伟斌,林勇,孙春喜,等.经皮椎体成形术术后新发椎体骨折特点及危险因素分析[J].中国医药科学,2021,11(10):210-212,224.
[24] LIN S, CAI X, CHENG Q, et al. Association between bone turnover markers, BMD and height loss of cemented vertebrae after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Orthop Surg Res. 2022;17(1):202.
[25] AN Z, CHEN C, WANG J, et al. Logistic regression analysis on risk factors of augmented vertebra recompression after percutaneous vertebral augmentation. J Orthop Surg Res. 2021;16(1):374.
[26] HOU Y, YAO Q, ZHANG G, et al. Polymethylmethacrylate distribution is associated with recompression after vertebroplasty or kyphoplasty for osteoporotic vertebral compression fractures: A retrospective study. PLoS One. 2018;13(6):e0198407.
[27] 曹冬子,许正伟,王存良,等.老年骨质疏松性椎体压缩骨折经皮椎体后凸成形术后新发骨折的危险因素分析[J].空军医学杂志, 2018,34(1):41-44.
[28] LI YX, GUO DQ, ZHANG SC, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42(9):2131-2139.
[29] YU W, ZHANG H, YAO Z, et al. Prediction of subsequent vertebral compression fractures after thoracolumbar kyphoplasty: a multicenter retrospective analysis. Pain Med. 2023;24(8):949-956.
|