中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (36): 5846-5851.doi: 10.12307/2024.678
• 骨与关节图像与影像 bone and joint imaging • 上一篇 下一篇
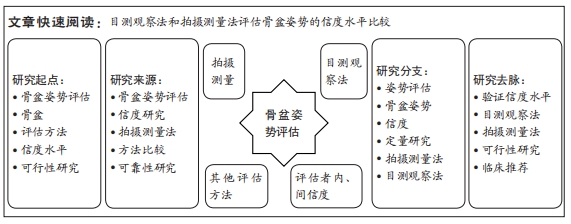
拍摄测量技术评估健康人体骨盆姿势的信度
董苗苗,李 想,解佳妮,张立新,王悦曦
- 中国医科大学附属盛京医院康复中心,辽宁省沈阳市 110134
Reliability of photogrammetry for evaluating pelvic posture in healthy individuals
Dong Miaomiao, Li Xiang, Xie Jiani, Zhang Lixin, Wang Yuexi
- Second Department of Rehabilitation, Shengjing Hospital Affiliated to China Medical University, Shenyang 110134, Liaoning Province, China
摘要:
文题释义:
拍摄测量法:是一种通过拍摄图像或视频来进行测量和分析的方法。它通常用于医学、工程、科学研究等领域,用于获取物体的尺寸、形状、角度等信息。通过拍摄图像或视频,可以使用计算机软件进行测量和分析,从而得出所需的数据和结论。拍摄测量法可以提供非接触式的测量方式,具有快速、准确、方便等优点,被广泛应用于各个领域。骨盆姿势:是指骨盆在立位或坐位时的位置和倾斜角度。骨盆姿势通常包括前后倾、左右倾等方面的变化。前后倾是指骨盆在前后方向上的倾斜程度,正常情况下应该保持适度的前倾。左右倾是指骨盆在左右方向上的倾斜程度,正常情况下应该保持平衡。不正确的骨盆姿势可能导致身体姿态的不稳定,造成肌肉不平衡、脊柱曲度异常、运动功能障碍等问题。因此,保持正确的骨盆姿势对于维持身体健康和预防运动损伤非常重要。
背景:在临床中通常使用触诊方法定位髂前上棘、髂后上棘,通过目测观察法或拍摄测量法来确定骨盆的倾斜情况。其中目测观察法只能有定性的结论,且其信度较差;而拍摄测量法不仅更方便、快捷,还能给出较精确的定量数据,是最佳的临床评估方法之一。但是国内尚无针对使用拍摄测量法评估骨盆姿势的信度研究。
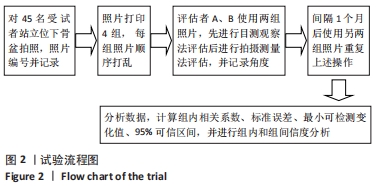
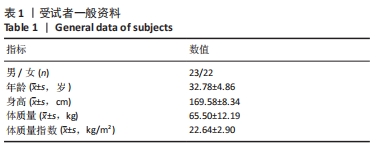
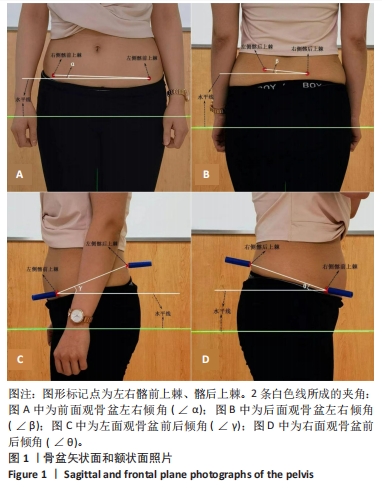
目的:采用目测观察法和拍摄测量法对骨盆姿势进行评估,比较两种方法的信度水平以指导临床应用。方法:选择45例健康受试者,在双侧髂前上棘及髂后上棘处作红色标记,从受试者前面、后面(额状面)、左面、右面(矢状面)进行骨盆姿势的拍照。从前面观、后面观选取骨盆左右倾角(ɑ、β角),即双侧髂前上棘连线或双侧髂后上棘连线与水平线的夹角;从侧面观选取骨盆前后倾角(γ、θ角),即同侧髂前上棘和髂后上棘连线与水平面的夹角,表示矢状面骨盆前后倾的情况。评估方法包括目测观察法和拍摄测量法,2位评估者进行独立评估,先使用目测观察法记录骨盆α、β、γ、θ角,再使用拍摄测量法记录骨盆α、β、γ、θ角。间隔1个月后再次进行目测观察法和拍摄测量法,分别记录骨盆α、β、γ、θ角。采用相关系数分析2种评估方法及前后测量所得数据,0.90-0.99为相关性优秀,0.80-0.89为相关性良好,0.70-0.79为相关性中度,≤0.69为相关性较差;并且通过计算得到测量标准误及最小可检测变化值以评价评估者间和评估者内部信度。
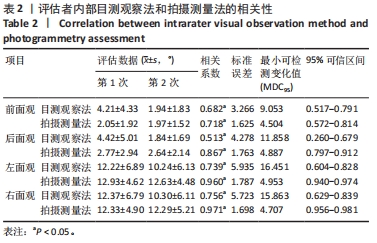
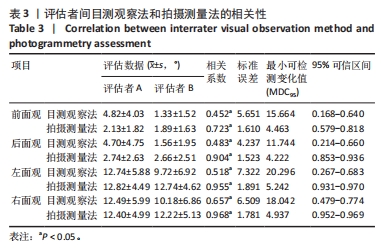
结果与结论:①评估者内部相关系数,目测观察法和拍摄测量法的相关系数:前面观为0.682和0.718,后面观为0.513和0.867,左面观为0.739和0.960,右面观为0.756和0.971;目测观察法前面观和后面观的相关性较差,左面和右面观的相关性为中度;拍摄测量法前面观的相关性为中度,后面观的相关性良好,左面和右面观的相关性均为优秀。测量标准误方面:前面观为3.266和1.625,后面观为4.278和1.763,左面观为5.935和1.787,右面观为5.723和1.698。最小可检测变化值方面:前面观为9.053和4.504,后面观为11.858和4.887,左面观为16.451和4.953,右面观为15.863和4.707。②评估者间相关系数,目测观察法和拍摄测量法的相关系数:前面观为0.452和0.723,后面观为0.483和0.904,左面观为0.518和0.955,右面观为0.657和0.968;目测观察法4个方向的的相关性均较差;拍摄测量法除前面观的相关性为中度,其他3个方面的相关性均位优秀。测量标准误方面:前面观为5.651和1.610;后面观为4.237和1.523;左面观为7.322和1.891;右面观为6.509和1.781。最小可检测变化值方面:前面观为15.664和4.463;后面观为11.744和4.222;左面观为20.296和5.242;右面观为18.042和4.937。③结果证实拍摄测量法评估矢状面、额状面骨盆姿势的评估者内部、评估者间信度均很好,尤其是通过拍摄测量法的数据稳定性较好;该方法简单、快捷、高效、准确、成本低廉、无X射线损害,能定性、定量地反映出患者骨盆的实际情况,适合在临床中推广使用。
https://orcid.org/0000-0002-3556-6894 (董苗苗)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号:
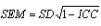 [21]。根据最小可检测变化值MDC95评估测量变异性,测量MDC95的意义在于,在测量中发现大于MDC95的变化被认为是真实变化,而不是由测量误差引起的,其计算公式为:
[21]。根据最小可检测变化值MDC95评估测量变异性,测量MDC95的意义在于,在测量中发现大于MDC95的变化被认为是真实变化,而不是由测量误差引起的,其计算公式为: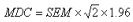 [22]。文章统计学方法已经中国医科大学附属盛京医院生物统计学专家审核。
[22]。文章统计学方法已经中国医科大学附属盛京医院生物统计学专家审核。