[1] 罗杰,魏戌,李家金.项韧带钙化的临床意义及其生物力学探讨[J]. 中国骨伤,2010,23(4):305-307.
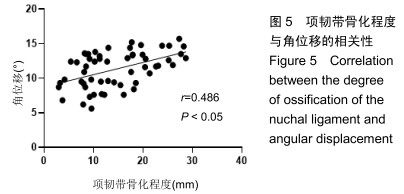
[2] YING J, TENG H, QIAN Y, et al.Radiographic analysis of the correlation between ossification of the nuchal ligament and sagittal alignment and segmental stability of the cervical spine in patients with cervical spondylotic myelopathy.Acta Radiol. 2019;60(2):196-203.
[3] 于胜波,苑晓鹰,隋鸿锦.人类项韧带的结构及其意义[J].中国临床解剖学杂志,2015,33(5):612-614.
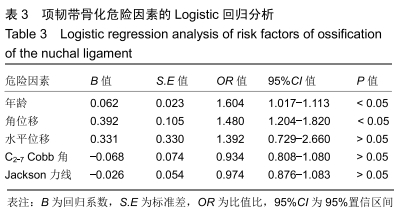
[4] JUN HS, KIM JH, AHN JH, et al. T1 slope and degenerative cervical spondylolisthesis. Spine. 2015;40:220-226.
[5] TSAI YL, WENG MC, CHEN TW, et al. Correlation between the ossification of nuchal ligament and clinical cervical disorders. Kaohsiung J Med Sci. 2012;28(10):538-544.
[6] WANG YJ, SHI Q, LU WW, et al. Cervical intervertebral disc degeneration induced by unbalanced dynamic and static forces: a novel in vivo rat model. Spine. 2006; 31(14): 1532-1538.
[7] FUJIMORI T, WATABE T, IWAMOTO Y, et al. Prevalence, concomitance, and distribution of ossification of the spinal ligaments: results of whole spine CT scans in 1500 Japanese patients. Spine. 2016;41(21):1668-1676.
[8] WANG H, ZOU F, JIANG J, et al. Analysis of radiography findings of ossification of nuchal ligament of cervical spine in patients with cervical spondylosis.Spine. 2014;39(1): E7-E11.
[9] GAO K, ZHANG J, LAI J, et al.Correlation between cervical lordosis and cervical disc herniation in young patients with neck pain.Medicine. 2019;98(31):e16545.
[10] GROB D ,FRAUENFELDER H. The association between cervical spine curvature and neck pain. Eur Spine J. 2007; 16(5):669-678.
[11] XU-HUI Z, JIA-HU F, LIAN-SHUN J, et al. Clinical significance of cervical vertebral flexion and extension spatial alignment change. Spine. 2009;34(1):21-26.
[12] 洪浩.项韧带骨化的X线表现及与颈椎退变关系的探讨[D].杭州:浙江大学,2011.
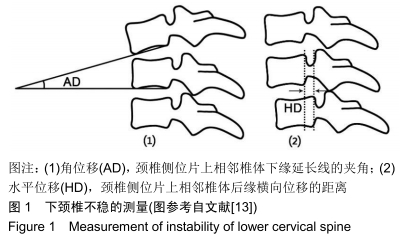
[13] 路宽,丁文元,杨大龙,等.单节段脊髓型颈椎病伴下颈椎不稳的影像学表现及预后因素分析[J].中华骨科杂志,2014,34(3): 273-279.
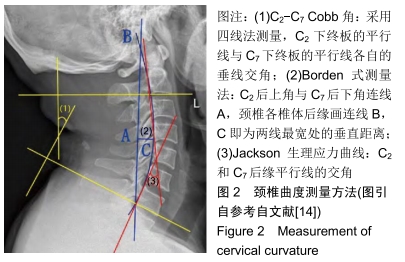
[14] 刘湘,龙耀武,王锋,等.颈椎病严重程度与颈椎曲度相关性的影像学研究[J].临床放射学杂志,2018,37(6):1021-1024.
[15] 蒋爱民,杨晨明,于胜波,等.人类项韧带的精细解剖结构[J].中国组织工程研究与临床康复,2007,11(10):1887-1891.
[16] TAKESHITA K, PETERSON ET, BYLSKI-AUSTROW D, et al. The nuchal ligament restrains cervical spine flexion. Spine. 2004;29:388-393.
[17] BOZKURT Y, ÇIÇEK EI,SANAL HT. Finger-shaped sesamoid bones aligned within the nuchal ligament.Spine J. 2016; 16(11):e743-e744.
[18] SHEDID D, BENZEL EC. Cervical spondylosis anatomy: Pathophysiology and biomechanics. Neurosurgery. 2007; 60(1):7-13.
[19] LIU B, LIU Z, VANHOOF T, et al. Kinematic study of the relation between the instantaneous center of rotation and degenerative changes in the cervical intervertebral disc. Eur Spine J. 2014; 23(11):2307-2313.
[20] BO Y, ZHIWEI W, YIN Z, et al. Radiographic features and correlation analysis of location of ossification in patients with cervical ossification of the posterior longitudinal ligament combined with ossification of the nuchal ligament. World Neurosurg. 2018;116:e929-e933.
[21] KIM DG, OH YM, EUN JP. The clinical significance of ossification of ligamentum nuchae in simple lateral radiograph: a correlation with cervical ossification of posterior longitudinal ligament. J Korean Neurosurg Soc. 2015;58(5):442-447.
[22] YOSHII T, HIRAI T, IWANAMI A, et al. Co-existence of ossification of the nuchal ligament is associated with severity of ossification in the whole spine in patients with cervical ossification of the posterior longitudinal ligament -A multi-center CT study. J Orthop Sci. 2019;24(1):35-41.
[23] GOKCE E, BEYHAN M. Evaluating ossifications of the nuchal ligament with cervical computed tomography. Eurasian J Med. 2018;50(1):23-27.
[24] KIM KW, OH YM. Increased prevalence of ossification of posterior longitudinal ligament and increased bone mineral density in patients with ossification of nuchal ligament. Korean J Spine. 2016;13(3):139-143.
[25] YU M, ZHAO WK, LI M, et al. Analysis of cervical and global spine alignment under Roussouly sagittal classification in Chinese cervical spondylotic patients and asymptomatic subjects. Eur Spine J. 2015;24(6):1265-1273.
[26] YOON SY, MOON HI, LEE SC, et al.Association between cervical lordotic curvature and cervical muscle cross-sectional area in patients with loss of cervical lordosis. Clin Anat. 2018; 31(5):710-715.
[27] SEONG HY, LEE MK, JEON SR, et al. Prognostic factor analysis for management of chronic neck pain: can we predict the severity of neck pain with lateral cervical curvature? J Korean Neurosurg Soc.2017;60(4):456-464.
[28] ALIZADA M, LI RR. Cervical instability in cervical spondylosis patients: Significance of the radiographic index method for evaluation.Der Orthopäde. 2018;47(12):977-985.
[29] HARRISON DE, HARRISON DD, CAILLIET R, et al. Cobb method or harrison posterior tangent method. Spine. 2000; 25(16):2072-2078.
[30] 任龙喜,何玉宝,郭函,等.颈部疼痛程度与颈椎曲度相关性的临床观察[J]. 中国脊柱脊髓杂志,2011,21(9):750-753.
[31] 张玉婷,王翔,詹红生.颈椎曲度的测量方法及其临床意义[J].中国骨伤,2014,27(12):1062-1064.
[32] LEE SH, SON ES, SEO EM, et al. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J. 2015;15(4):705-712.
[33] TAMAI K, BUSER Z, PAHOLPAK P, et al.MRI kinematic analysis of T1 sagittal motion between cervical flexion and extension positions in 145 patients. Eur Spine J. 2018;27(5): 1034-1041.
[34] TAMAI K, BUSER Z, PAHOLPAK P, et al. Can C7 slope substitute the T1 slope? An analysis using cervical radiographs and kinematic MRIs. Spine. 2018;43(7):520-525.
[35] SCHEER JK, TANG JA, SMITH JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications. J Neurosurg Spine. 2013;19(2):141-159.
[36] TANG JA, SCHEER JK, SMITH JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Spine J. 2012;12(9): S65-S65.
[37] 侯文根,梁秋冬,徐海斌.退行性下颈椎不稳定症的诊断与治疗[J]. 中国医药导刊,2011,13(1):23-24.
[38] LIANG H, LIU G, LU S, et al.Epidemiology of ossification of the spinal ligaments and associated factors in the Chinese population: a cross-sectional study of 2000 consecutive individuals. BMC Musculoskel Dis. 2019;20(1):253.
[39] 程亭秀,毕玉春.项韧带损伤与颈椎病关系探讨[J].脊柱外科杂志, 2004,2(4):241-242.
[40] MORI K, YOSHII T, HIRAI T, et al.Prevalence and distribution of ossification of the supra/interspinous ligaments in symptomatic patients with cervical ossification of the posterior longitudinal ligament of the spine: a CT-based multicenter cross-sectional study. BMC Musculoskel Dis. 2016;17(1):492.
|