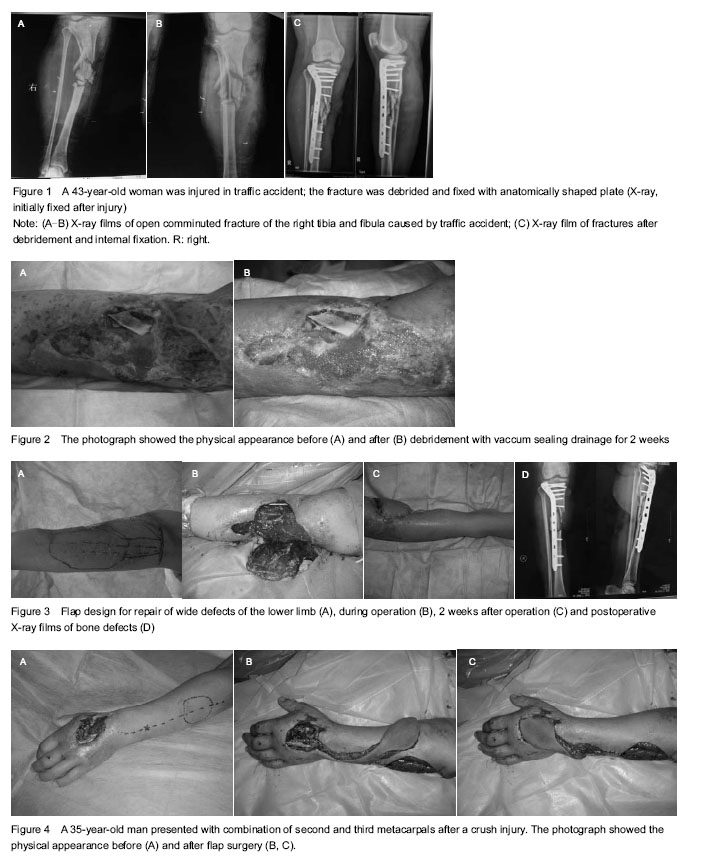
The design of flap shape and size must be in accordance with the defect at the recipient site. Generally, flap size depends on the blood supply capacity of the vascular pedicle, which may be estimated according to the diameter of the pedicle vessel, age, general patient condition,
etc [7]. The flap should be sized slightly larger than the measured width of the defect and be long enough so that excessive tension is not placed on the flap after it is sutured
[2-4, 6]. The flaps are coagulated with bipolar coagulation under suction-irrigation, and closed suction drainage tubes are placed underneath the flap until the bacterial culture is negative (
Figure 5). The priorities include closing the wounds as soon as possible by primary or secondary closure, restoring anatomy, and restoring function. The approaches from simple to complex are: primary closure, local flaps, skin grafting, pedicle flaps, and finally free flaps
[8-11].
Debridement of bone
Cortical bone is a dense type of bone tissue, and avascular necrosis is the death of bone tissue due to a lack of blood supply. Therefore, necrotic bone should be aggressively removed[12]. Cortical bone exposure, without an underlying fracture, may lead to bone necrosis and sequester formation leading to infection and osteomyelitis. The necrosis of cortical bone is almost always progressive: due to interruption of the blood supply, the bone structures then collapse, resulting in bone destruction.
Cierny and Mader classified osteomyelitis based on the affected portion of the bone, the physiologic status of the host and the local environment[13]. All dystrophic and inflammatory soft tissues surrounding the open wound should be excised unto healthy tissues. In all 94 cases of this study, all pathological and infected tissues were removed during debridement until healthy, hard and bleeding bone was encountered.
In pedicled flaps, a real individual vascular pattern is included as well as a nourishing pedicle. Some of them are skin flaps or fasciocutaneous flaps while others are muscular or musculocutaneous[14]. A free flap also contains a tissue unit vascularised by a nourishing pedicle but it is usually situated far from the receptor site[15].
In this study, the segment of necrotic bone was removed to prevent further steoporotic fractures and fracture instability, and free-flap coverage of such small soft-tissue defects also became revascularized. The removal of the sequestrum is preferred when the sequestrum is causing the patient to be painful, when the lesion is large and disrupting the surface of the fracture, or when it is causing significant inflammation of the wound.
Wound irrigation is the steady flow of a solution across an open wound surface to achieve wound hydration, to remove deeper debris, and to assist with the visual examination[16-17]. When performed properly, wound irrigation can aid in wound healing from the inside tissue layers outward to the skin surface. Choosing an appropriate solution is a critical step in wound irrigation.
Solutions intended for topical use include topical cleansers, antibiotics, antifungals, antiseptics and anesthetics. Current literature generally favors use of normal saline (rinsing at a low pressure for several times)[18-19]. In the case of more contaminated wounds, the wounds should be irrigated until all visible debris is removed[20].
Debridement of tendon, joint capsule and articular cartilage
Tendon nutrition is provided indirectly via synovial fluid and directly via vascular inflow through mesenteric folds called vinculae, and long-term survival of the tendon grafts appears to be dependent on the revascularization of the transplanted tissues. Like any other connective tissue, tendon does not undergo neovascularisation under normal circumstances. The vascularisation of autogenic tendon grafts is vital to allow the tendon to function as a ligamentous structure or as an alternative tendon[21].
Tendons are capable of healing and recovering from injuries in a process that is controlled by the tenocytes (basic tendon generating cells and their surrounding cells). Transplanted autogenous tendon grafts undergo a process of inflammation, revascularization, proliferation, and remodeling[21]. Infected necrotic tendon looks dull, soft, and partially liquefied, and it should be debrided to clean hard normal-looking tendon[22]. For debridement of joint capsule, the joint is thoroughly irrigated and all abscesses are debrided.
The articular cartilage is normally a dense, smooth, white structure that provides a very smooth, pain-free gliding surface for knee motion. The debridement of articular cartilage involves the mechanical removal of separating, unstable parts of diseased cartilage and flushing the inflamed synovial fluid mediators. These can be useful palliative treatments to reduce pain, mechanical irritation and inflammatory mediators but any benefits tend to be short-term only. Arthroscopic abrasion, drilling, and microfracture should be employed to improve the long-term results of debridement and lavage[23].
The retention or removal of metal implants
Having hardware (metal implants) poses an extra risk because the implanted material is avascular and therefore not protected by the host’s immune system[9, 11]. Antibiotics can only reach infected area by diffusion from the surrounding tissues. The absence of vascularized tissue and the presence of metal hardware near the wound create the environment for postoperative infection[24]. Unfilled dead space, such as the space that develops around hardware and bones when significant soft tissue damage occurs, increases the chance for infection[25].
As there are no evidence-based guidelines to dictate whether the hardware should be removed or retained in the presence of an acute infection, the management requires flexibility in the treatment plan while trying to avoid a poor outcome such as infected non-union[26]. According to the available literature, it is recommendable to maintain the hardware in place until osseous union has occurred[27-29]. But metal implants can loosen, fracture, corrode, migrate, cause pain even after a fracture has healed[30-31].
We recommend that whenever possible and practical for the individual patient, fixation devices should be removed once their service as an aid to healing is accomplished. Implant removal should be followed by adequate postoperative management to avoid refractures.
Perioperative management in traumatic soft tissue defects using revascularized flaps should arouse common concern and systematic research. Careful and aggressive early debridement, a large number of washing, a reasonable choice of flap, adequate drainage, and appropriate use of antibiotics are critical to flap survival. Foreign materials such as bone fragments, necrotic tendons, unstable parts of diseased cartilage and metal implants should be handled properly.
.jpg)