[1] 中华医学会骨科学分会脊柱外科学组, 中华医学会骨科学分会骨科康复学组. 腰椎间盘突出症诊疗指南[J]. 中华骨科杂志,2020,40(8):477-487.
[2] POJSKIC M, BISSON E, OERTEL J, et al. Lumbar disc herniation: Epidemiology, clinical and radiologic diagnosis WFNS spine committee recommendations. World Neurosurg X. 2024;22:100279.
[3] MUTHU S, RAMAKRISHNAN E, CHELLAMUTHU G. Is Endoscopic Discectomy the Next Gold Standard in the Management of Lumbar Disc Disease? Systematic Review and Superiority Analysis. Global Spine J. 2021;11(7):1104-1120.
[4] KONG M, XU D, GAO C, et al. Risk Factors for Recurrent L4-5 Disc Herniation After Percutaneous Endoscopic Transforaminal Discectomy: A Retrospective Analysis of 654 Cases. Risk Manag Healthc Policy. 2020;13: 3051-3065.
[5] 莫航沣, 陈亚萍, 韩慧, 等. 临床预测模型研究方法与步骤[J]. 中国循证医学杂志,2024,24(2):228-236.
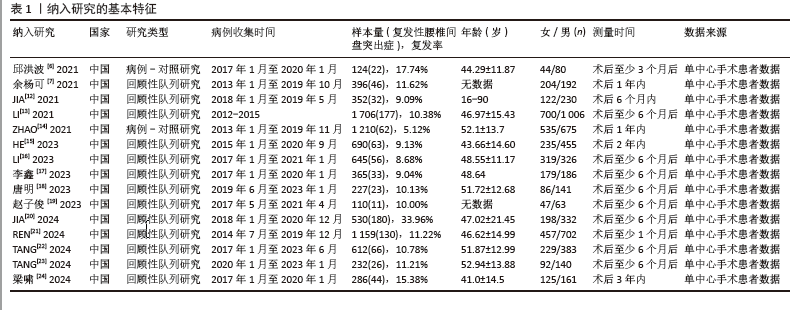
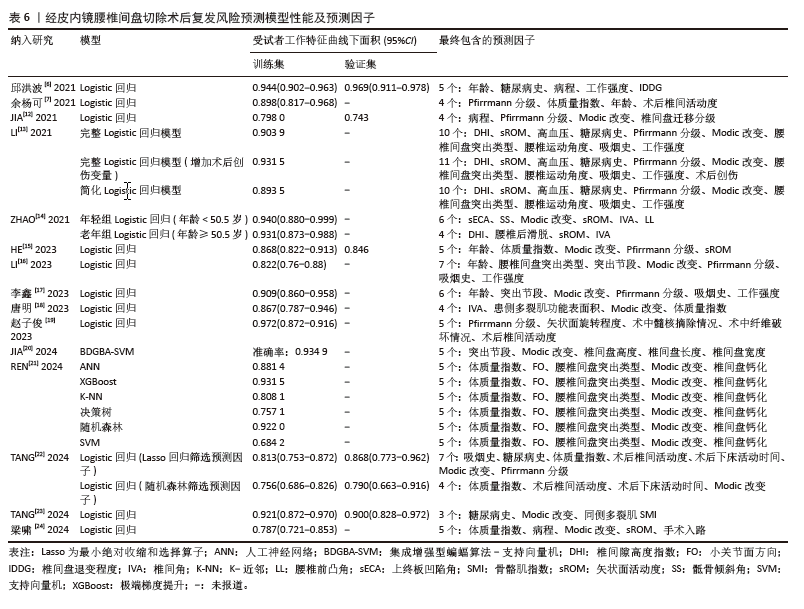
[6] 邱洪波, 唐乐, 何甜, 等. 椎间孔镜治疗腰椎间盘突出症患者术后复发的个体化预警模型的建立[J]. 西安交通大学学报(医学版),2021,42(6):817-822.
[7] 余杨可, 夏磊. 经皮内镜腰椎间盘切除术术后复发的危险因素分析及概率预测[J]. 河南医学研究,2021,30(6):973-977.
[8] GEERSING GJ, BOUWMEESTER W, ZUITHOFF P, et al. Search filters for finding prognostic and diagnostic prediction studies in Medline to enhance systematic reviews. PLoS One. 2012;7(2):e32844.
[9] MOONS KG, DE GROOT JA, BOUWMEESTER W, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. 2014;11(10): e1001744.
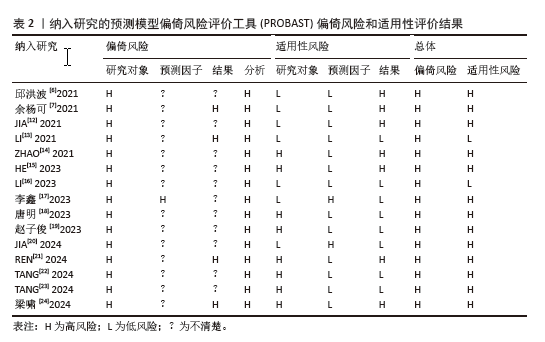
[10] MOONS KGM, WOLFF RF, RILEY RD, et al. PROBAST: A Tool to Assess Risk of Bias and Applicability of Prediction Model Studies: Explanation and Elaboration. Ann Intern Med. 2019;170(1):W1-W33.
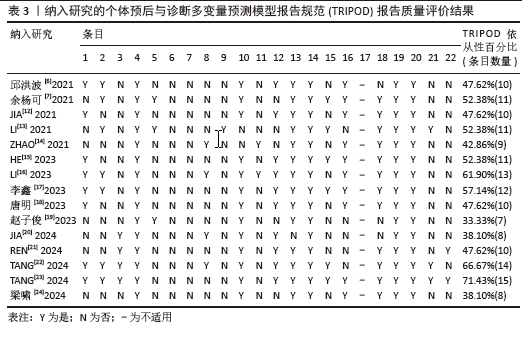
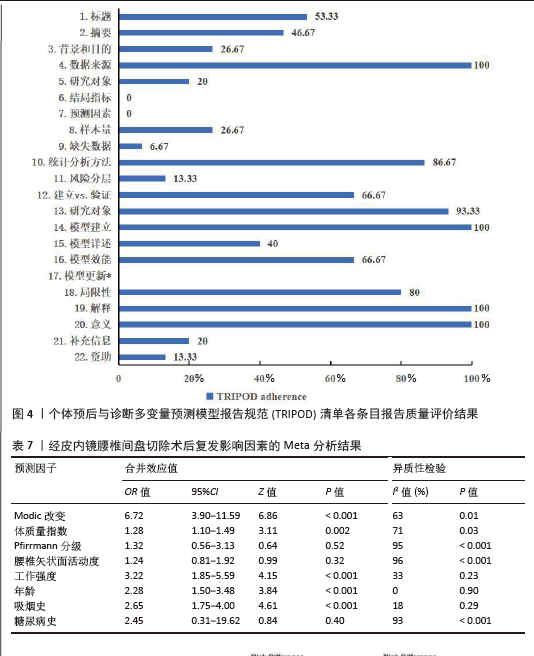
[11] COLLINS GS, REITSMA JB, ALTMAN DG, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594.
[12] JIA M, SHENG Y, CHEN G, et al. Development and validation of a nomogram predicting the risk of recurrent lumbar disk herniation within 6 months after percutaneous endoscopic lumbar discectomy. J Orthop Surg Res. 2021; 16(1):274.
[13] LI Y, WANG B, LI H, et al. Adjuvant surgical decision-making system for lumbar intervertebral disc herniation after percutaneous endoscopic lumber discectomy: a retrospective nonlinear multiple logistic regression prediction model based on a large sample. Spine J. 2021;21(12):2035-2048.
[14] ZHAO C, ZHANG H, WANG Y, et al. Nomograms for Predicting Recurrent Herniation in PETD with Preoperative Radiological Factors. J Pain Res. 2021;14: 2095-2109.
[15] HE H, MA J, XIONG C, et al. Development and Validation of a Nomogram to Predict the Risk of Lumbar Disk Reherniation within 2 Years After Percutaneous Endoscopic Lumbar Discectomy. World Neurosurg. 2023;172:e349-e356.
[16] LI X, PAN B, CHENG L, et al. Development and Validation of a Prognostic Model for the Risk of Recurrent Lumbar Disc Herniation After Percutaneous Endoscopic Transforaminal Discectomy. Pain Physician. 2023;26(1):81-90.
[17] 李鑫, 罗鸣然, 李根, 等. 建立与验证经皮内窥镜腰椎间盘切除后复发风险的预测模型[J]. 中国组织工程研究,2023, 27(13):2087-2092.
[18] 唐明, 曾凡袆, 常新东, 等. 椎旁功能性肌肉横截面积预测腰椎间盘突出症术后复发的Nomogram建立与验证[J]. 暨南大学学报(自然科学与医学版),2023, 44(6):602-611.
[19] 赵子俊, 王轶, 张志强, 等. 老年腰椎间盘突出症患者经皮椎间孔镜髓核摘除术后复发的影响因素及列线图预测模型[J]. 川北医学院学报,2023,38(4): 500-504.
[20] JIA M, LAI J, LI K, et al. Optimizing prediction accuracy for early recurrent lumbar disc herniation with a directional mutation-guided SVM model. Comput Biol Med. 2024;173:108297.
[21] REN G, LIU L, ZHANG P, et al. Machine Learning Predicts Recurrent Lumbar Disc Herniation Following Percutaneous Endoscopic Lumbar Discectomy. Global Spine J. 2024;14(1):146-152.
[22] TANG M, WANG S, WANG Y, et al. Development and Validation of a Nomogram Predicting Postoperative Recurrent Lumbar Disc Herniation Based on Activity Factors. Risk Manag Healthc Policy. 2024;17: 689-699.
[23] TANG M, WANG S, WANG Y, et al. Nomogram Development and Validation for Predicting Postoperative Recurrent Lumbar Disc Herniation Based on Paraspinal Muscle Parameters. J Pain Res. 2024;17:2121-2131.
[24] 梁啸, 李东儒, 陈筱, 等. 内镜腰椎间盘切除术后复发的因素及预测模型[J].中国矫形外科杂志,2024,32(9):775-780.
[25] YEN HK, OGINK PT, HUANG CC, et al. A machine learning algorithm for predicting prolonged postoperative opioid prescription after lumbar disc herniation surgery. An external validation study using 1,316 patients from a Taiwanese cohort. Spine J. 2022;22(7):1119-1130.
[26] BERG B, GOROSITO MA, FJELD O, et al. Machine Learning Models for Predicting Disability and Pain Following Lumbar Disc Herniation Surgery. JAMA Netw Open. 2024; 7(2):e2355024.
[27] AZIMI P, MOHAMMADI HR, BENZEL EC, et al. Use of artificial neural networks to predict recurrent lumbar disk herniation. J Spinal Disord Tech. 2015;28(3):E161-E165.
[28] HARADA GK, SIYAJI ZK, MALLOW GM, et al. Artificial intelligence predicts disk re-herniation following lumbar microdiscectomy: development of the “RAD” risk profile. Eur Spine J. 2021;30(8): 2167-2175.
[29] SHAN ZM, REN XS, SHI H, et al. Machine Learning Prediction Model and Risk Factor Analysis of Reoperation in Recurrent Lumbar Disc Herniation Patients After Percutaneous Endoscopic Lumbar Discectomy. Global Spine J. 2023;10:21925682231173353.
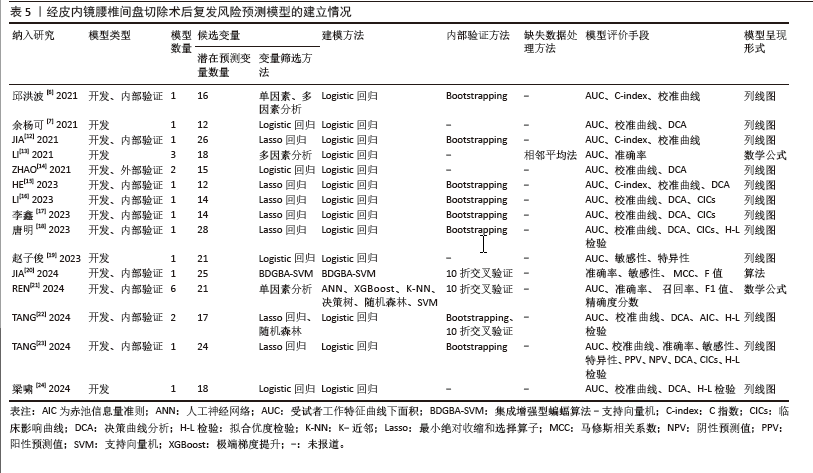
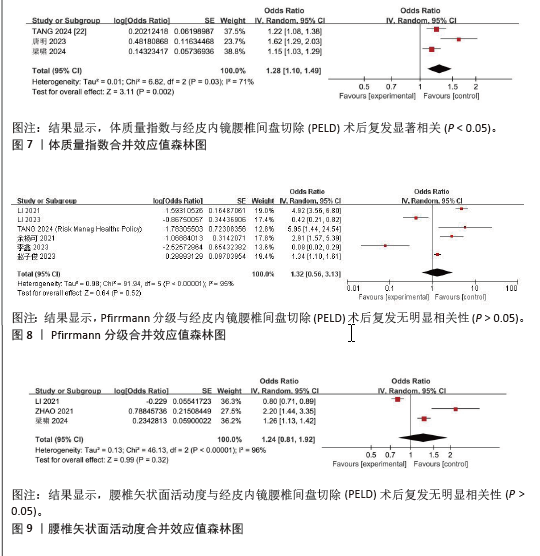
[30] ZHAO J, ZENG L, ZHAO S, et al. Associations of recurrent lumbar disc herniation after percutaneous endoscopic lumbar discectomy with age, body mass index, modic change, disc degeneration and sacral slope: A quantitative review. Exp Ther Med. 2024;27(5):195.
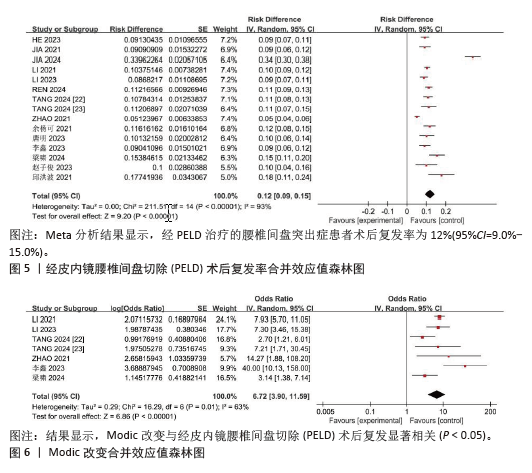
[31] JIANG L, XIE X, HE R, et al. Analysis of risk factors for post-operative recurrence after percutaneous endoscopic lumbar discectomy in patients with lumbar disc herniation: a meta-analysis. J Orthop Surg Res. 2023;18(1):935.
[32] ZHAO Z, QI H, WANG C, et al. Investigating the impact of cartilaginous endplate herniation on recovery from percutaneous endoscopic lumbar discectomy. J Orthop Surg Res. 2024;19(1):264.
[33] FENG X, NIAN S, CHEN J, et al. Modic changes in patients with lumbar disc herniation followed more than 1 year after lumbar discectomy: a systematic review and meta-analysis. PeerJ. 2024;12:e17851.
[34] KE S, HE X, YANG M, et al. The biomechanical influence of facet joint parameters on corresponding segment in the lumbar spine: a new visualization method. Spine J. 2021;21(12):2112-2121.
[35] YANG W, YANG Y, WANG Y, et al. Metformin prevents the onset and progression of intervertebral disc degeneration: New insights and potential mechanisms (Review). Int J Mol Med. 2024;54(2):71.
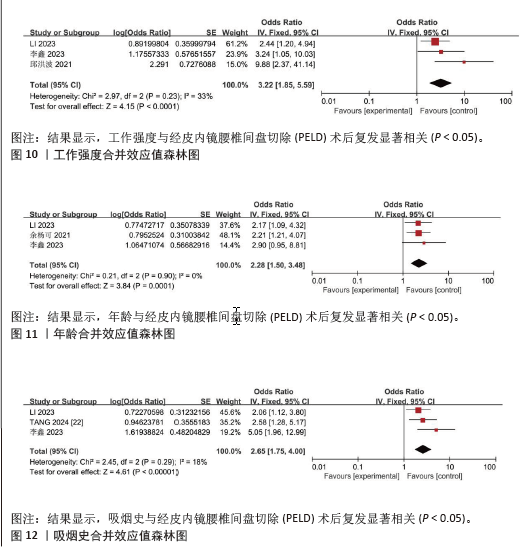
[36] 周顺, 黄品强, 杨勇. 基于病因学角度探究LDH中医证型职业风险的相关性[J]. 浙江中医药大学学报,2021,45(10): 1125-1129.
[37] LAASIK R, LANKINEN P, KIVIMAKI M, et al. Return to work after lumbar disc herniation surgery: an occupational cohort study. Acta Orthop. 2021;92(6):638-643.
[38] WALTER SS, LORBEER R, HEFFERMAN G, et al. Correlation between thoracolumbar disc degeneration and anatomical spinopelvic parameters in supine position on MRI. PLoS One. 2021;16(6):e0252385.
[39] ELMASRY S, ASFOUR S, DE RIVERO VACCARI JP, et al. Effects of Tobacco Smoking on the Degeneration of the Intervertebral Disc: A Finite Element Study. PLoS One. 2015;10(8): e0136137.
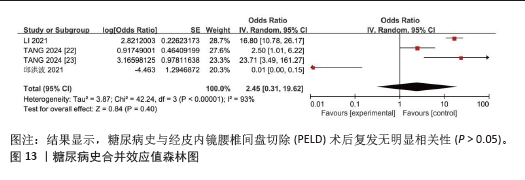
[40] 陈小英. 腰椎间盘突出症术后复发的影响因素研究[J]. 中国全科医学,2020,23(S1): 140-142.
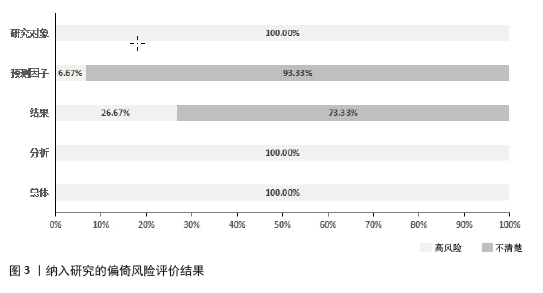
[41] 陈香萍, 张奕, 庄一渝, 等. PROBAST: 诊断或预后多因素预测模型研究偏倚风险的评估工具[J]. 中国循证医学杂志,2020, 20(6): 737-744.
[42] RILEY RD, ENSOR J, SNELL KIE, et al. Calculating the sample size required for developing a clinical prediction model. BMJ. 2020;368:m441.
[43] VAN SMEDEN M, MOONS KG, DE GROOT JA, et al. Sample size for binary logistic prediction models: Beyond events per variable criteria. Stat Methods Med Res. 2019;28(8):2455-2474.
[44] DWAN K, GAMBLE C, WILLIAMSON PR, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias - an updated review. PLoS One. 2013;8(7):e66844. |