中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (21): 3299-3305.doi: 10.12307/2024.614
• 骨科植入物 orthopedic implant • 上一篇 下一篇
三角肌结节指数联合术前因素构建老年肱骨近端骨折锁定钢板内固定失效的风险预测模型
徐大星1,2,纪木强2,涂泽松2,3,许伟鹏3,徐伟龙4,牛 维5
- 1广州中医药大学同等学力申请博士学位人员,广东省广州市 510006;2佛山市中医院三水医院骨科,广东省佛山市 528100;3佛山市中医院骨科,广东省佛山市 528000;4深圳平乐骨科医院骨科,广东省深圳市 518122;5广东省中医院关节外科,广东省广州市 510120
Constructing a risk prediction model for failure after locking plate fixation for proximal humeral fractures in the elderly by combining the deltoid tuberosity index with preoperative factors
Xu Daxing1, 2, Ji Muqiang2, Tu Zesong2, 3, Xu Weipeng3, Xu Weilong4, Niu Wei5
- 1Applicant with Equivalent Academic Qualifications for Doctoral Degree, Guangzhou University of Chinese Medicine, Guangzhou 510006, Guangdong Province, China; 2Department of Orthopedics, Sanshui Branch of Foshan Hospital of TCM, Foshan 528100, Guangdong Province, China; 3Department of Orthopedics, Foshan Hospital of TCM, Foshan 528000, Guangdong Province, China; 4Department of Orthopedics, Shenzhen Pingle Orthopedics Hospital, Shenzhen 518122, Guangdong Province, China; 5Department of Articular Surgery, Guangdong Provincial Hospital of Chinese Medicine, Guangzhou 510120, Guangdong Province, China
摘要:

文题释义:
三角肌结节指数:三角肌粗隆平面上,骨皮质外侧横径与骨皮质内侧横径的比值。测量三角肌结节指数是评估肱骨头骨密度的简便和有效方法。文献报道三角肌结节指数< 1.44考虑肱骨近端骨质疏松或骨质不良。临床预测模型:其原理是基于模型中纳入的风险因素对因变量的影响程度量化并赋值,得到各个因素的总分后换算成结局变量的风险概率。此文采用列线图作为预测模型,将预测风险可视化,便于临床筛选高风险患者和采取个性化治疗。
背景:老年肱骨近端骨折是三大骨质疏松性骨折之一,解剖锁定钢板内固定是国内大部分医生治疗难以复位和复杂骨折类型的首选,但术后发生复位失效的概率较高,严重影响患者生活质量。
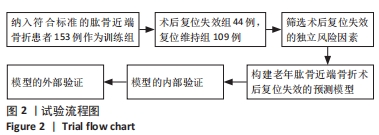
目的:探讨三角肌结节指数与老年肱骨近端骨折术后复位失效的相关性,分析筛选出老年肱骨近端骨折术后复位失效的术前独立风险因素,并构建和验证临床预测模型的有效性。方法:收集2012年6月至2021年6月佛山市中医院符合标准的接受切开复位锁定钢板治疗的153例老年肱骨近端骨折患者的临床资料,根据其是否发生术后复位失效分为复位失效亚组和复位维持亚组。采用先单因素后多因素Logistic回归分析筛选独立风险因素,通过R语言构建列线图,内部验证采用Bootstrap法重抽样1 000次后,通过Hosmer-Lemeshow拟合优度关联检验、绘制受试者工作特征曲线、校准曲线、临床决策和影响曲线评价其拟合优度、区分度、校准能力和临床应用价值。选择2013年6月至2021年8月收治的55例老年肱骨近端骨折患者作为模型外部验证组,评价预测模型的稳定性和准确度。
结果与结论:①训练组153例患者中,44例患者出现钢板内固定术后复位失效,失效率为28.8%;多因素Logistic回归分析结果显示,三角肌结节指数[OR=9.782,95%CI(3.798,25.194)]、骨折端内翻成角移位[OR=4.209, 95%CI(1.472,12.031)]、肱骨内侧柱粉碎[OR=4.278,95%CI(1.670,10.959)]是老年肱骨近端骨折术后复位失效的独立风险因素(P < 0.05);②基于独立风险因素构建预测模型并绘制列线图,训练组Hosmer-Lemeshow检验结果显示,χ2=0.812(P=0.976),曲线下面积=0.830[95%CI(0.762,0.898)];校准图结果表明模型预测风险和实际发生风险有较好的一致性;决策曲线和临床影响曲线结果表明列线图具有较好的临床适用性;③预测模型在验证组预测术后复位失效总正确率86%,曲线下面积=0.902[95%CI(0.819,0.985)];④提示三角肌结节指数< 1.44、肱骨内侧柱粉碎、骨折端内翻成角移位是老年肱骨近端骨折术后复位失效的独立风险因素;⑤此次研究构建的风险预测模型内、外部验证表明该模型区分度、准确度和临床适用度较高,可用于个性化预测和筛选老年肱骨近端骨折术后复位失效的高危人群,模型的阈值风险概率高于65%时的预测高风险人数和实际发生人数高度匹配,临床医生应采用针对性治疗。
https://orcid.org/0000-0001-7021-2752 (徐大星)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: