Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (31): 4937-4944.doi: 10.12307/2024.704
Previous Articles Next Articles
Erythropoietin-overexpressed umbilical cord mesenchymal stem cells inhibit neuroapoptosis in ischemic-hypoxic SH-SY5Y and its mechanism
Li Ruibo1, 2, Kong Ning1, 2, Sun Lei3, Ma Baodong3, Jin Ranran3, Zhang Wenjin2, Yue Han4, Zhang Hui2
- 1Xinxiang Medical University, Xinxiang 453003, Henan Province, China; 2Department of Neurosurgery, Zhengzhou Central Hospital Affiliated to Zhengzhou University, Zhengzhou 450007, Henan Province, China; 3Stem Cell Regenerative Medicine Translational Center, Zhengzhou Central Hospital Affiliated to Zhengzhou University, Zhengzhou 450007, Henan Province, China; 4Stem Cell Regenerative Medicine Center, Henan Provincial People’s Hospital, Zhengzhou 463599, Henan Province, China
-
Received:2023-08-15Accepted:2023-09-25Online:2024-11-08Published:2024-01-22 -
Contact:Zhang Hui, Master, Chief physician, Department of Neurosurgery, Zhengzhou Central Hospital Affiliated to Zhengzhou University, Zhengzhou 450007, Henan Province, China Yue Han, MD, Chief physician, Stem Cell Regenerative Medicine Center, Henan Provincial People’s Hospital, Zhengzhou 463599, Henan Province, China -
About author:Li Ruibo, Master candidate, Physician, Xinxiang Medical University, Xinxiang 453003, Henan Province, China; Department of Neurosurgery, Zhengzhou Central Hospital Affiliated to Zhengzhou University, Zhengzhou 450007, Henan Province, China -
Supported by:Henan Medical Science and Technology Research Program Joint Construction Project, No. LHGJ20191045 (to ZH); Key Research & Development and Promotion Project of Henan Province, No. 222102310032 (to YH); Henan Medical Science and Technology Research Program Joint Construction Project, No. LHGJ20220858 (to ZWJ)
CLC Number:
Cite this article
Li Ruibo, Kong Ning, Sun Lei, Ma Baodong, Jin Ranran, Zhang Wenjin, Yue Han, Zhang Hui. Erythropoietin-overexpressed umbilical cord mesenchymal stem cells inhibit neuroapoptosis in ischemic-hypoxic SH-SY5Y and its mechanism[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(31): 4937-4944.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

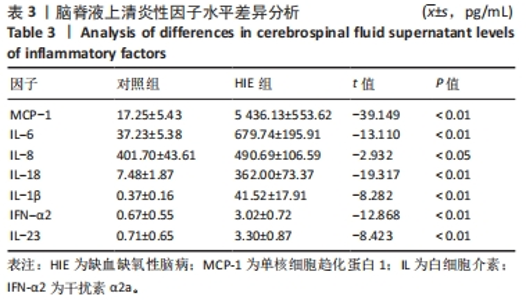
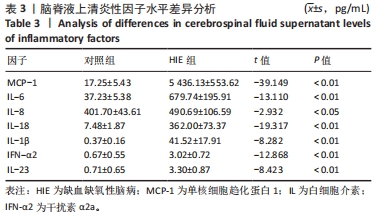
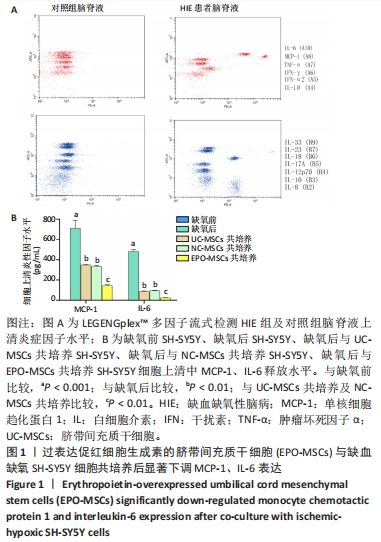
共培养细胞上清中炎性因子分泌情况,见图1B。缺氧后SH-SY5Y组细胞上清MCP-1、IL-6表达水平较缺氧前SH-SY5Y组明显增多[MCP-1:(711.24±79.38) pg/mL vs. (0.00±0.00) pg/mL;IL-6:(482.43±2.84) pg/mL vs. (0.00±0.00) pg/mL,均P < 0.01];缺氧后UC-MSCs共培养组细胞上清MCP-1、IL-6表达水平较缺氧后SH-SY5Y组明显减少[MCP-1:(347.78±6.54) pg/mL vs. (711.24±79.38) pg/mL;IL-6:(86.74±4.92) pg/mL vs. (482.43±2.84) pg/mL,均P < 0.01];缺氧后NC-MSCs共培养组细胞上清MCP-1、IL-6表达水平与缺氧后UC-MSCs共培养组无差异(P > 0.05);缺氧后EPO-MSCs共培养组MCP-1、IL-6表达水平较缺氧后NC-MSCs共培养组明显减少[MCP-1:(144.38±9.21) pg/mL vs. (332.76±9.07) pg/mL;IL-6:(24.61±1.32) pg/mL vs. (95.23±3.10) pg/mL,均P < 0.01]。"
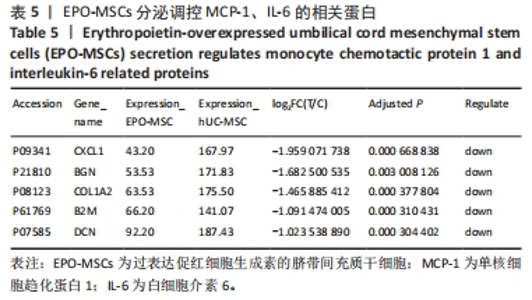
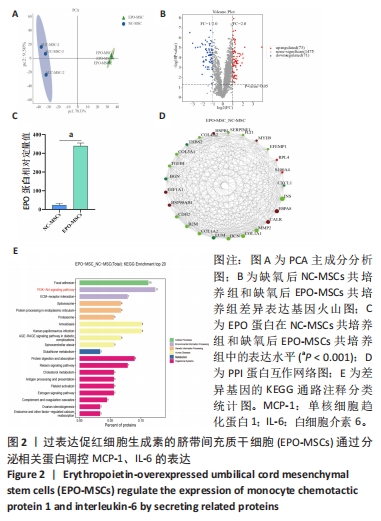
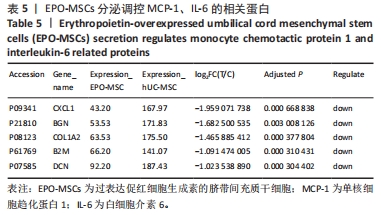
2.2 蛋白组学分析NC-MSCs、EPO-MSCs蛋白差异表达 对NC-MSCs、EPO-MSCs进行主成分聚类分析,见图2A,通过RNA-seq在EPO-MSCs组与NC-MSCs组鉴定出144个差异表达蛋白,其中上调73个、下调71个,对144个差异表达蛋白以火山图的方式进行可视化,见图2B。EPO-MSCs组与NC-MSCs组比较,EPO蛋白表达显著增高(P < 0.01),见图2C。发现与调控MCP-1、IL-6表达相关的蛋白如 CXCL1、BGN、DCN等,见表5,与影响凋亡相关的蛋白如B2M、COL1A2、CALR等,见图2D。KEGG富集结果发现,PI3K/AKT信号通路相关基因显著富集,见图2E。"

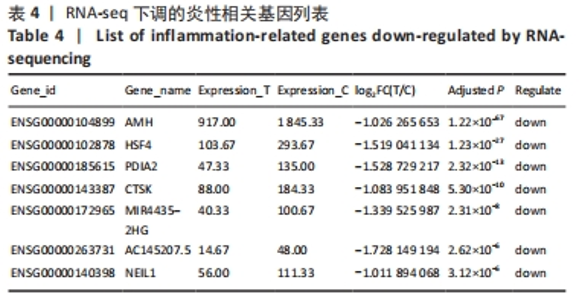
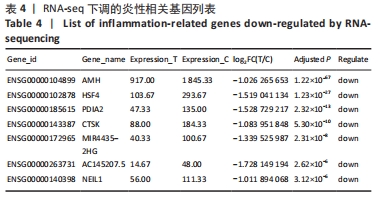
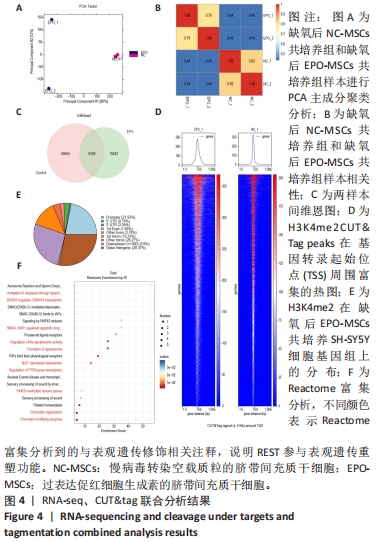
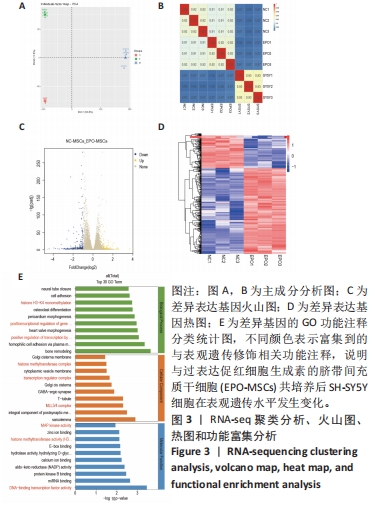
2.3 EPO-MSCs共培养后在表观遗传水平发生变化 通过转录组测序,对缺氧后SH-SY5Y组、缺氧后NC-MSCs共培养组、缺氧后EPO-MSCs共培养组样本进行主成分聚类分析,见图3A,各组样本间相关性进行可视化处理,见图3B,通过RNA-seq在缺氧后EPO-MSCs共培养组和缺氧后NC-MSCs共培养组之间鉴定了405个差异表达基因,其中117个下调基因、288个上调基因,以火山图和热图的方式进行可视化,见图3C,D。差异表达基因GO功能富集聚类分析,结果发现生物过程富集分析存在H3K4甲基化、基因转录后调控;细胞成分富集分析存在组蛋白甲基转移酶复合物、转录调节因子复合物、MLL3/4复合体;分子功能富集分析存在MAPK激酶活性、H3组蛋白甲基转移酶活性、DNA结合转录因子的活性,见图3E。"
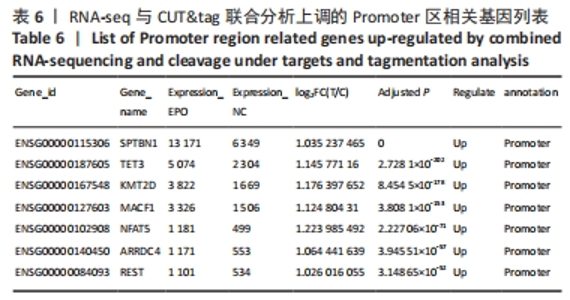
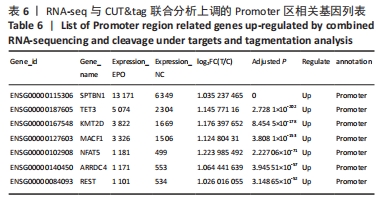
2.4 RNA-seq、CUT&tag联合分析,明确REST参与表观遗传重塑功能 对缺氧后NC-MSCs共培养组和缺氧后EPO-MSCs共培养组样本进行主成分聚类分析,见图4A,各组样本间相关性进行可视化处理,见图4B。由于生物过程富集分析发现H3K4甲基化,并且H3K4me2是转录激活型的表观调控信号,因此该研究选择H3K4me2为靶向分子,应用CUT&Tag测序技术检测基因组H3K4me2修饰情况,分析可能的转录激活基因,探讨EPO-MSCs神经保护机制。两组样本间差异基因表达情况见图4C,两组间在基因转录起始位点(TSS)周围富集情况以及H3K4me2在缺氧后EPO-MSCs共培养组结合区域分布,见图4D,E,结果发现REST、TET3在启动子区有丰富的组蛋白H3K4me2修饰。由此可见,H3K4me2结合在REST、TET3基因启动子区,见表6。Reactome富集分析结果提示调控区域差异基因在转录调节,以及染色质组织、染色质修饰酶高度富集,见图4F。"

2.5 REST缺失SH-SY5Y细胞构建及其表型验证 为了明确EPO-MSCs通过调控REST的神经保护机制,应用慢病毒载体感染构建稳定敲低REST的SH-SY5Y细胞。经流式细胞术分析,约99.24%与99.33%的慢病毒转染的SH-SY5Y细胞为GFP阳性,转染效率高,见图5A,B。RT-qPCR分析证实REST基因在mRNA上的表达水平,pLKO.1-Vector组表达量明显高于pLKO.1-sh1组和pLKO.1-sh2组(P < 0.001),见图5C。Western blot分析证实REST基因在蛋白上的表达水平,pLKO.1-Vector组表达量明显高于pLKO.1-sh1组和pLKO.1-sh2组(P < 0.01),见图5D。而EPO-MSCs与NC-MSCs、UC-MSCs的 REST mRNA表达没有明显差异(P > 0.05),见图5E。"
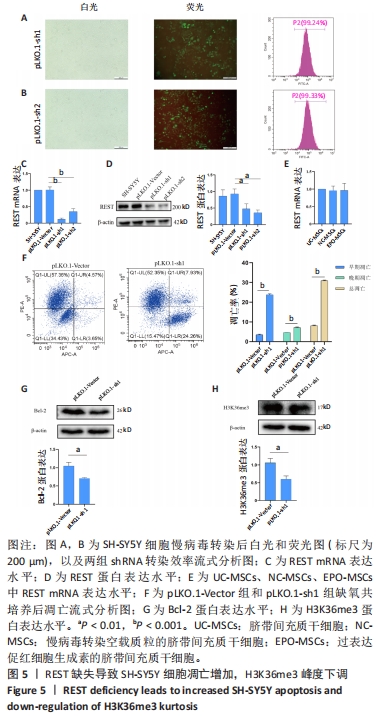

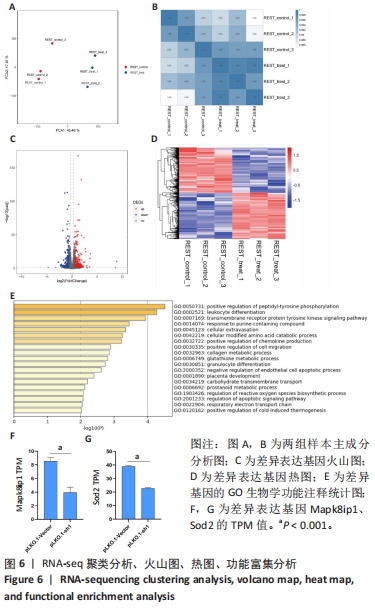
为了探索转录因子REST在凋亡保护中的作用,该研究将pLKO.1-Vector组和pLKO.1-sh1组细胞缺血缺氧24 h后与EPO-MSCs共培养48 h。流式细胞仪检测结果可见,pLKO.1-sh1组早期凋亡率、晚期凋亡率、总凋亡率均显著增加(P < 0.001),见图5F。Western blot分析证实Bcl-2以及H3K36me3在蛋白上的表达水平,pLKO.1-sh1组表达量明显低于pLKO.1-Vector组(P < 0.01),见图5G,H。 2.6 转录组测序分析缺血缺氧处理后敲低REST的SH-SY5Y细胞、敲低REST的SH-SY5Y细胞与EPO-MSCs共培养后基因表达谱 对各组样本进行主成分聚类分析,见图6A,各组样本间相关性进行可视化处理,见图6B,通过RNA-seq筛选出461个差异表达基因,其中229个下调基因、232个上调基因,以火山图和热图的方式进行可视化,见图6C,D。GO功能富集分析提示,生物学功能中调节凋亡信号通路显著下调,见图6E,筛选出与凋亡保护相关基因(Camk2b、Csf2、G0s2、Cd74、Lck、Mapk8ip1、Sod2、Mpv17l、Cth)显著下调,见图6F,G。显著下调TOP10的基因中有5个基因(Cth、Sod2、Aqp1 、Cdsn、Cd74)与炎症相关。其中Mapk8ip1、Sod2直接受REST调控。"
| [1] 王文广,王斌,胡颖杰,等.MRI与CT对新生儿缺血缺氧性脑病诊断价值的分析[J].中国妇幼保健,2015,30(4):639-641. [2] WANG W, JIA L. Regulatory Mechanism of MicroRNA-30b on Neonatal Hypoxic-Ischemic Encephalopathy (HIE). J Stroke Cerebrovasc Dis. 2021;30(3):105553. [3] LIU CY, AL-WARD H, NGAFFO MEKONTSO F, et al. Experimental Study on the Correlation between miRNA-373 and HIF-1α, MMP-9, and VEGF in the Development of HIE. Biomed Res Int. 2021;2021:5553486. [4] EDMONDS CJ, HELPS SK, HART D, et al. Minor neurological signs and behavioural function at age 2 years in neonatal hypoxic ischaemic encephalopathy (HIE). Eur J Paediatr Neurol. 2020;27:78-85. [5] LI JB, WU WS, DU B, et al. Impact of mild hypothermia therapy on hemodynamics during the induction stage in neonates with moderate to severe hypoxic-ischemic encephalopathy. Zhongguo Dang Dai Er Ke Za Zhi. 2021;23(2):133-137. [6] YE L, FENG Z, DOYCHEVA D, et al. CpG-ODN exerts a neuroprotective effect via the TLR9/pAMPK signaling pathway by activation of autophagy in a neonatal HIE rat model. Exp Neurol. 2018;301(Pt A):70-80. [7] HU X, LI S, DOYCHEVA DM, et al. Rh-CSF1 Attenuates Oxidative Stress and Neuronal Apoptosis via the CSF1R/PLCG2/PKA/UCP2 Signaling Pathway in a Rat Model of Neonatal HIE. Oxid Med Cell Longev. 2020;2020:6801587. [8] MASSARO AN, MURTHY K, ZANILETTI I, et al. Short-term outcomes after perinatal hypoxic ischemic encephalopathy: a report from the Children’s Hospitals Neonatal Consortium HIE focus group. J Perinatol. 2015;35(4):290-296. [9] 余静,薛伟,李亚萍.亚低温联合促红细胞生成素对HIE患儿脑部生理和神经系统发育的改善作用[J].临床研究,2023,31(5):65-68. [10] LI F, ZHANG K, LIU H, et al. The neuroprotective effect of mesenchymal stem cells is mediated through inhibition of apoptosis in hypoxic ischemic injury. World J Pediatr. 2020;16(2):193-200. [11] LI T, LIU Y, YU L, et al. Human Umbilical Cord Mesenchymal Stem Cells Protect Against SCA3 by Modulating the Level of 70 kD Heat Shock Protein. Cell Mol Neurobiol. 2018;38(3):641-655. [12] FRENETTE PS, PINHO S, LUCAS D, et al. Mesenchymal stem cell: keystone of the hematopoietic stem cell niche and a stepping-stone for regenerative medicine. Annu Rev Immunol. 2013;31:285-316. [13] PARK WS, SUNG SI, AHN SY, et al. Hypothermia augments neuroprotective activity of mesenchymal stem cells for neonatal hypoxic-ischemic encephalopathy. PLoS One. 2015;10(3):e0120893. [14] PARK M, KIM HM, SHIN HA, et al. Human Pluripotent Stem Cell-Derived Neural Progenitor Cells Promote Retinal Ganglion Cell Survival and Axon Recovery in an Optic Nerve Compression Animal Model. Int J Mol Sci. 2021;22(22):12529. [15] AHMAD KA, BENNETT MM, JUUL SE, et al. Utilization of Erythropoietin within the United States Neonatal Intensive Care Units from 2008 to 2017. Am J Perinatol. 2021;38(7):734-740. [16] ZHOU H, HE Y, XIONG W, et al. MSC based gene delivery methods and strategies improve the therapeutic efficacy of neurological diseases. Bioact Mater. 2022;23: 409-437. [17] BELL KF, BENT RJ, MEESE-TAMURI S, et al. Calmodulin kinase IV-dependent CREB activation is required for neuroprotection via NMDA receptor-PSD95 disruption. J Neurochem. 2013;126(2):274-287. [18] 班跃耀,孙蕾,马保东,等.促红细胞生成素基因修饰的人脐带间充质干细胞对神经元周期和凋亡的调控作用及机制[J].新乡医学院学报,2023,40(10): 909-916. [19] HWANG JY, ZUKIN RS. REST, a master transcriptional regulator in neurodegenerative disease. Curr Opin Neurobiol. 2018;48:193-200. [20] DAY JJ. Genetic and epigenetic editing in nervous system. Dialogues Clin Neurosci. 2019;21(4):359-368. [21] ALY H, KHASHABA MT, EL-AYOUTY M, et al. IL-1beta, IL-6 and TNF-alpha and outcomes of neonatal hypoxic ischemic encephalopathy. Brain Dev. 2006;28(3): 178-182. [22] 邹良,何秋红,陈秋杨,等. IL-17/IL-23炎症轴在新生儿缺氧缺血性脑病发病中的作用机制探究[J].河北医科大学学报,2023,44(3):305-309. [23] KUMAR H, KAWAI T, AKIRA S. Pathogen recognition by the innate immune system. Int Rev Immunol. 2011;30(1):16-34. [24] SINGH S, ANSHITA D, RAVICHANDIRAN V. MCP-1: Function, regulation, and involvement in disease. Int Immunopharmacol. 2021;101(Pt B):107598. [25] 许云鹤,刘永刚,赵小妹,等.血清SAA、RBP4、MCP-1与缺血性脑卒中脑损伤及梗死程度的关系研究[J].临床和实验医学杂志,2018,17(3):255-258. [26] 张艳华,孔慧霞,张嘉雯,等.血清及脑脊液IL-1β、PCT、MCP-1水平变化在化脓性脑膜炎患儿病情评估及预后判断中的应用价值[J].中国临床实用医学,2017,8(3):45-47. [27] GROH J, HEINL K, KOHL B, et al. Attenuation of MCP-1/CCL2 expression ameliorates neuropathy in a mouse model for Charcot-Marie-Tooth 1X. Hum Mol Genet. 2010;19(18):3530-3543. [28] KOLATTUKUDY PE, NIU J. Inflammation, endoplasmic reticulum stress, autophagy, and the monocyte chemoattractant protein-1/CCR2 pathway. Circ Res. 2012; 110(1):174-189. [29] HUANG XY, HU QP, SHI HY, et al. Everolimus inhibits PI3K/Akt/mTOR and NF-kB/IL-6 signaling and protects seizure-induced brain injury in rats. J Chem Neuroanat. 2021;114:101960. [30] HOU SM, CHEN PC, LIN CM, et al. CXCL1 contributes to IL-6 expression in osteoarthritis and rheumatoid arthritis synovial fibroblasts by CXCR2, c-Raf, MAPK, and AP-1 pathway. Arthritis Res Ther. 2020;22(1):251. [31] ZHANG X, ZHANG F, YAO F, et al. Bergenin has neuroprotective effects in mice with ischemic stroke through antioxidative stress and anti-inflammation via regulating Sirt1/FOXO3a/NF-κB signaling. Neuroreport. 2022;33(13):549-560. [32] ZHONG Q, ZOU Y, LIU H, et al. Toll-like receptor 4 deficiency ameliorates β2-microglobulin induced age-related cognition decline due to neuroinflammation in mice. Mol Brain. 2020;13(1):20. [33] CHENG Y, WANG G, ZHAO L, et al. Periplocymarin Induced Colorectal Cancer Cells Apoptosis Via Impairing PI3K/AKT Pathway. Front Oncol. 2021;11:753598. [34] TIAN Q, GUO Y, FENG S, et al. Inhibition of CCR2 attenuates neuroinflammation and neuronal apoptosis after subarachnoid hemorrhage through the PI3K/Akt pathway. J Neuroinflammation. 2022;19(1):312. [35] NIE Y, SHU C, SUN X. Cooperative binding of transcription factors in the human genome. Genomics. 2020;112(5):3427-3434. [36] WANG S, MEYER DH, SCHUMACHER B. H3K4me2 regulates the recovery of protein biosynthesis and homeostasis following DNA damage. Nat Struct Mol Biol. 2020;27(12):1165-1177. [37] SOLLINGER C, LILLIS J, MALIK J, et al. Erythropoietin Signaling Regulates Key Epigenetic and Transcription Networks in Fetal Neural Progenitor Cells. Sci Rep. 2017;7(1):14381. [38] KAYA-OKUR HS, WU SJ, CODOMO CA, et al. CUT&Tag for efficient epigenomic profiling of small samples and single cells. Nat Commun. 2019;10(1):1930. [39] RYAN BJ, BENGOA-VERGNIORY N, WILLIAMSON M, et al. REST Protects Dopaminergic Neurons from Mitochondrial and α-Synuclein Oligomer Pathology in an Alpha Synuclein Overexpressing BAC-Transgenic Mouse Model. J Neurosci. 2021;41(16):3731-3746. [40] LAM XJ, MANIAM S, CHEAH PS, et al. REST in the Road Map of Brain Development. Cell Mol Neurobiol. 2023;43(7):3417-3433. [41] PERERA A, EISEN D, WAGNER M, et al. TET3 is recruited by REST for context-specific hydroxymethylation and induction of gene expression. Cell Rep. 2015; 11(2):283-294. [42] ABDERRAHMANI A, STEINMANN M, PLAISANCE V, et al. The transcriptional repressor REST determines the cell-specific expression of the human MAPK8IP1 gene encoding IB1 (JIP-1). Mol Cell Biol. 2001;21(21):7256-7267. [43] MARTIN D, ALLAGNAT F, GESINA E, et al. Specific silencing of the REST target genes in insulin-secreting cells uncovers their participation in beta cell survival. PLoS One. 2012;7(9):e45844. [44] KINUGAWA S, WANG Z, KAMINSKI PM, et al. Limited exercise capacity in heterozygous manganese superoxide dismutase gene-knockout mice: roles of superoxide anion and nitric oxide. Circulation. 2005;111(12):1480-1486. |
| [1] | Qiu Xiaoyan, Li Bixin, Li Jingdi, Fan Chuiqin, Ma Lian, Wang Hongwu. Differentiation of insulin-producing cells from human umbilical cord mesenchymal stem cells infected by MAFA-PDX1 overexpressed lentivirus [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1000-1006. |
| [2] | Liu Qiwei, Zhang Junhui, Yang Yuan, Wang Jinjuan. Role and mechanism of umbilical cord mesenchymal stem cells on polycystic ovary syndrome [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1015-1020. |
| [3] | He Yuanjie, Chen Yuheng, Zhao Yongchao, Wang Zhenglong. Progress in epigenetic regulation of vascular smooth muscle cell remodeling in the occurrence and development of aortic aneurysms [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 602-608. |
| [4] | Han Xia, Zhao Ruidong, Yang Junli. Targeted induction of human umbilical cord mesenchymal stem cells cultured with human peripheral blood serum into neural stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(25): 4000-4004. |
| [5] | Chen Mingxue, Niu Jianhua, Lin Haiyan, Wu Gang, Wan Ben. Physicochemical properties and cytocompatibility of biomimetically precipitated nanocrystalline calcium phosphate granules [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(22): 3502-3508. |
| [6] | Pan Xiaoying, Xu Yongde, Liu Zhiqiang, Xing Xiaowen, Yang Yong. Differential effects of hypoxia and oxidative stress on paracrine of mesenchymal stem cells from different sources [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(19): 3024-3030. |
| [7] | He Bo, He Zhijun, Li Jinpeng, Liu Tao, Ma Suilu, Wei Xiaotao, Wang Weiwei, Xie Jing. Improving the strategy of mesenchymal stem cells in treatment of flap ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(19): 3097-3103. |
| [8] | Wu Yaru, Mi Yan, Wei Kaiyue, Gao Heping, Zhang Dingyu, Wang Caili. Regulatory effect of human umbilical cord mesenchymal stem cells on intestinal barrier function in diabetic nephropathy rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(19): 2967-2973. |
| [9] | Xie Ting, Liu Tingting, Zeng Xuehui, Li Yamin, Zhou Panghu, Yi Nianhua. Vitamin D3 attenuates high-glucose exposure-induced oxidative stress to promote osteogenic differentiation of human umbilical cord mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(19): 2981-2987. |
| [10] | Liu Zhong, Li Kewei, Wang Min, Liu Wenhui, Zhang Leilei, Guo Song, Qian Hui, Fu Qiang. Effects of micro-electric field on proliferation and osteogenic differentiation of human umbilical cord mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 1983-1988. |
| [11] | Deng Guodong, Yang Jia, Liu Yang. Preparation and characterization of chitosan biguanide hydrochloride hydrogels loading mouse umbilical cord mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 1989-1995. |
| [12] | Yuan Yuanyuan, Pan Lu, Zhou Shaolan, Liang Yan, Xu Jianwei, Xu Wen. Effect of miR-26b on proliferation, migration and osteogenic differentiation of stem cells from human exfoliated deciduous teeth and human umbilical cord mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 2017-2023. |
| [13] | Zhang Wenhui, Pei Xiaohang, Kong Dai, Liu Zhongwen. Efficacy of umbilical cord mesenchymal stem cells replacing donor bone marrow cells in haploidentical hematopoietic stem cell transplantation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 2042-2046. |
| [14] | Zheng Mingkui, Xue Chenhui, Guan Xiaoming, Ma Xun. Human umbilical cord mesenchymal stem cell-derived exosomes reduce the permeability of blood-spinal cord barrier after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 50-55. |
| [15] | Cui Lianxu, Jiang Wenkang, Lu Dahong, Xu Junrong, Liu Xiaocui, Wang Bingyun. Clinical-grade human umbilical cord mesenchymal stem cells affect the improvement of neurological function in rats with traumatic brain injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 835-839. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||