Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (35): 5691-5696.doi: 10.3969/j.issn.2095-4344.2017.35.019
Previous Articles Next Articles
Finite element analysis of posterior anatomical locking plate for distal tibia
Wang Hai-yan1, Xu Gui-cun2, Cai Yong-qiang1, Li Zhi-jun1, Zhang Shao-jie1, Gao Shang1, Wang Xing1, Li Xiao-he1
- 1Department of Anatomy, School of Basic Medicine, Inner Mongolia Medical University, Hohhot 010110, Inner Mongolia Autonomous Region, China; 2Department of Emergency Surgery, the Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010110, Inner Mongolia Autonomous Region, China
-
Online:2017-12-18Published:2018-01-02 -
Contact:Xu Gui-cun, Master, Chief physician, Department of Emergency Surgery, the Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010110, Inner Mongolia Autonomous Region, China Li Xiao-he, M.D., Professor, Department of Anatomy, School of Basic Medicine, Inner Mongolia Medical University, Hohhot 010110, Inner Mongolia Autonomous Region, China -
About author:Wang Hai-yan, Master, Associate professor, Master’s supervisor, Department of Anatomy, School of Basic Medicine, Inner Mongolia Medical University, Hohhot 010110, Inner Mongolia Autonomous Region, China -
Supported by:the Overseas Science and Technology Project of Inner Mongolia Autonomous Region in 2016; the Science and Technology Project of Inner Mongolia Autonomous Region in 2016
CLC Number:
Cite this article
Wang Hai-yan, Xu Gui-cun, Cai Yong-qiang, Li Zhi-jun, Zhang Shao-jie, Gao Shang, Wang Xing, Li Xiao-he. Finite element analysis of posterior anatomical locking plate for distal tibia[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(35): 5691-5696.
share this article
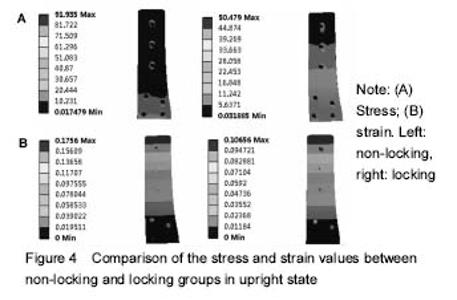
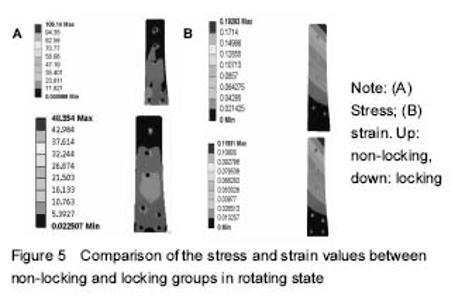
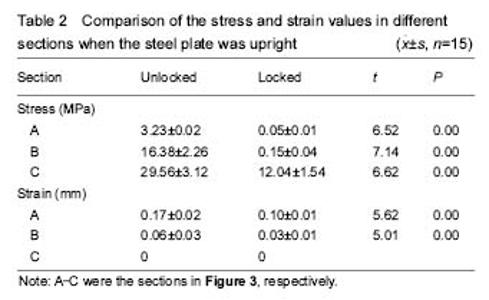
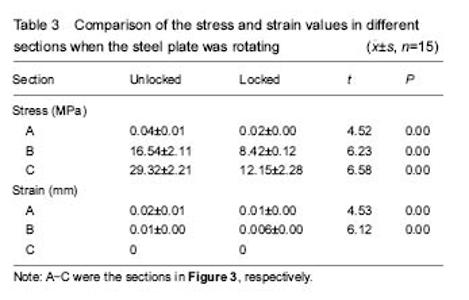
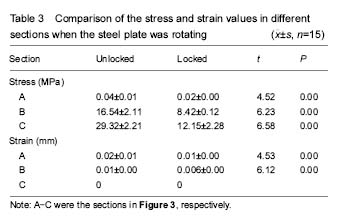
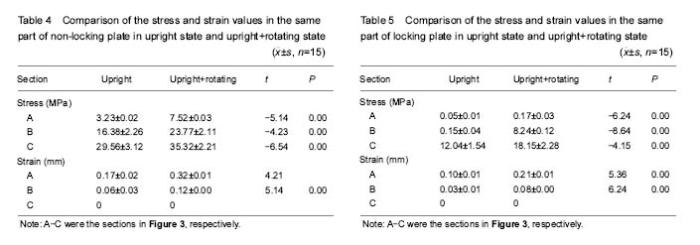
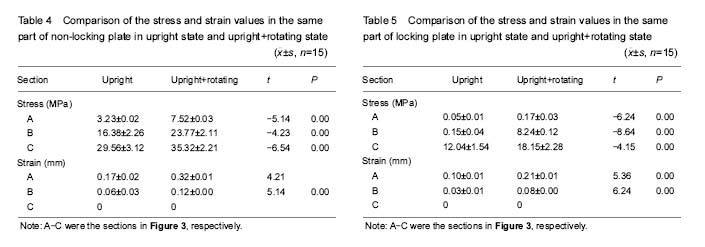
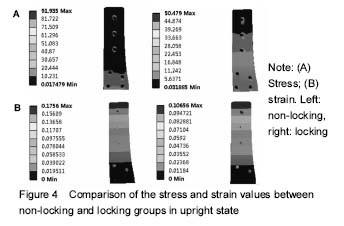
The finite element models of posterior anatomical locking plate for distal tibia A finite element model of posterior anatomical locking plate fixation for distal tibia was successfully established using three-dimensional reconstruction software Mimics16.01 and finite element software Ansys11.0. There were totally 43 536 units and 41 256 nodes, and the established finite element model showed good geometrical similarity with the real structure. Verification of the finite element model of posterior anatomical locking plate for distal tibia The model in this research was established based on the verified method by Shih et al[8], and therefore this model was qualified. The stress and strain comparison of the finite element models of posterior anatomical locking plate for distal tibia With the increasing of section (From A to C), the stress was increasing under upright + rotating state or upright, there was a positive correlation between stress and section (r=0.966, P < 0.001; r=0.945, P < 0.001). The unlocked and locked steel plate stresses under upright + rotating state were significantly larger than those under the upright state (P < 0.05). The stress and strain values of the unlocked steel plate were significantly larger than those of the locked steel plate (P < 0.05) (Figures 4, 5, Tables 2-5). "
| [1] Höntzsch D, Blauth M, Attal R. Angle-stable fixation of intramedullary nails using the Angular Stable Locking System® (ASLS). Oper Orthop Traumatol. 2011;23(5):387-396.[2] Ehlinger M, Adam P, Arlettaz Y, et al. Minimally-invasive fixation of distal extra-articular femur fractures with locking plates: limitations and failures. Orthop Traumatol Surg Res. 2011;97(6):668-674.[3] Nayak RM, Koichade MR, Umre AN, et al. Minimally invasive plate osteosynthesis using a locking compression plate for distal femoral fractures. J Orthop Surg (Hong Kong). 2011;19(2):185-190.[4] Malviya A, Reed MR, Partington PF. Acute primary total knee arthroplasty for peri-articular knee fractures in patients over 65 years of age. Injury. 2011;42(11):1368-1371.[5] Lopes JB, Figueiredo CP, Caparbo VF, et al. Osteoporotic fractures in the Brazilian community-dwelling elderly: prevalence and risk factors. J Clin Densitom. 2011;14(3):359-366.[6] Weil YA, Rivkin G, Safran O, et al. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011;71(1):186-190.[7] Hierholzer C, von Rüden C, Pötzel T, et al. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: A retrospective analysis. Indian J Orthop. 2011;45(3):243-250.[8] Shih KS, Hsu CC, Hsu TP. A biomechanical investigation of the effects of static fixation and dynamization after interlocking femoral nailing: a finite element study. J Trauma Acute Care Surg. 2012; 72(2):e46-53.[9] Salas C, Mercer D, DeCoster TA, et al. Experimental and probabilistic analysis of distal femoral periprosthetic fracture: a comparison of locking plate and intramedullary nail fixation. Part A: experimental investigation. Comput Methods Biomech Biomed Engin. 2011;14(2):157-164. [10] Han QT, Wang YJ, Tang HW. Biomechanical comparison of three methods of internal fixation for distal femoral fractures. Zhongguo Gu Shang. 2010;23(8):601-604.[11] Efstathopoulos N, Nikolaou VS, Xypnitos FN, et al. Investigation on the distal screw of a trochanteric intramedullary implant (Fi-nail) using a simplified finite element model. Injury. 2010;41(3):259-265. [12] Chang CY, Rupp JD, Reed MP, et al. Predicting the effects of muscle activation on knee, thigh, and hip injuries in frontal crashes using a finite-element model with muscle forces from subject testing and musculoskeletal modeling. Stapp Car Crash J. 2009;53: 291-328.[13] Bougherara H, Zdero R, Miric M, et al. The biomechanics of the T2 femoral nailing system: a comparison of synthetic femurs with finite element analysis. Proc Inst Mech Eng H. 2009;223(3):303-314.[14] Chen SH, Yu TC, Chang CH, et al. Biomechanical analysis of retrograde intramedullary nail fixation in distal femoral fractures. Knee. 2008;15(5):384-389. [15] Mann KA, Lee J, Arrington SA, et al. Predicting distal femur bone strength in a murine model of tumor osteolysis. Clin Orthop Relat Res. 2008;466(6):1271-1278. [16] Shih KS, Tseng CS, Lee CC, et al. Influence of muscular contractions on the stress analysis of distal femoral interlocking nailing. Clin Biomech (Bristol, Avon). 2008;23(1):38-44.[17] Mahaisavariya B, Sitthiseripratip K, Suwanprateeb J. Finite element study of the proximal femur with retained trochanteric gamma nail and after removal of nail. Injury. 2006;37(8):778-785.[18] Cegoñino J, García Aznar JM, Doblaré M, et al. A comparative analysis of different treatments for distal femur fractures using the finite element method. Comput Methods Biomech Biomed Engin. 2004;7(5):245-256.[19] Dubov A, Kim SY, Shah S, et al. The biomechanics of plate repair of periprosthetic femur fractures near the tip of a total hip implant: the effect of cable-screw position. Proc Inst Mech Eng H. 2011;225(9):857-865.[20] Shah S, Kim SY, Dubov A, et al. The biomechanics of plate fixation of periprosthetic femoral fractures near the tip of a total hip implant: cables, screws, or both? Proc Inst Mech Eng H. 2011;225(9):845-856.[21] Wilson LJ, Richards CJ, Irvine D, et al. Risk of periprosthetic femur fracture after anterior cortical bone windowing: a mechanical analysis of short versus long cemented stems in pigs. Acta Orthop. 2011;82(6):674-678. [22] Gutbrod A, Vincenti S, Kühn K, et al. An anatomical study of plate-rod fixation in feline tibiae. Vet Surg. 2017. in press. [23] Daolagupu AK, Mudgal A, Agarwala V, et al. A comparative study of intramedullary interlocking nailing and minimally invasive plate osteosynthesis in extra articular distal tibial fractures. Indian J Orthop. 2017;51(3):292-298. [24] Strotman PK, Karunakar MA, Seymour R, et al. Any cortical bridging predicts healing of supracondylar femur fractures after treatment with locked plating. J Orthop Trauma. 2017. in press.[25] Garg S, Khanna V, Goyal MP, et al. Comparative prospective study between medial and lateral distal tibial locking compression plates for distal third tibial fractures. Chin J Traumatol. 2017;20(3): 151-154.[26] Akra GA, Lazarides S, Nanu AM. Early results of minimally invasive percutaneous plate osteosynthesis for fractures of the distal tibia: a retrospective case series and review of the literature. Clin Med Insights Arthritis Musculoskelet Disord. 2017;10: 1179544117701724. [27] Busel GA, Watson JT. Plating of pilon fractures based on the orientation of the fibular shaft component: A biomechanical study evaluating plate stiffness in a cadaveric fracture model. J Orthop. 2017;14(2):308-312. [28] Lin C, Lin L, Vinesh L, et al. Distal tibial nonunion using a contralateral anterior L-shaped locking compression plate through a posterior-lateral approach: a retrospective case series. Injury. 2017;48(6):1224-1228. [29] Wenger R, Oehme F, Winkler J, et al. Absolute or relative stability in minimal invasive plate osteosynthesis of simple distal meta or diaphyseal tibia fractures? Injury. 2017;48(6):1217-1223. [30] Imren Y, Desteli EE, Erdil M, et al. Mid-term results of minimally invasive plate osteosynthesis and circular external fixation in the treatment of complex distal tibia fractures. J Am Podiatr Med Assoc. 2017;107(1):3-10.[31] Tosun HB, Agir I, Gumustas S, et al. Tibial lengthening using a fixator-assisted lengthening plate: a new technique. Trauma Mon. 2016;21(5):e25340. [32] Muzaffar N, Bhat R, Yasin M. Complications of minimally invasive percutaneous plating for distal tibial fractures. Trauma Mon. 2016;21(3):e22131. [33] Park KH, Kim JW, Kim HJ, et al. Corrective osteotomy of the distal femur with fixator assistance: A novel technique of minimally invasive osteosynthesis. J Orthop Sci. 2017;22(3):474-480.[34] Sivakumar R, Mohideen MG, Chidambaram M, et al. Management of large bone defects in diaphyseal fractures by induced membrane formation by masquelet’s technique. J Orthop Case Rep. 2016;6(3):59-62. [35] Liu W, Yang L, Kong X, et al. Stiffness of the locking compression plate as an external fixator for treating distal tibial fractures: a biomechanics study. BMC Musculoskelet Disord. 2017;18(1):26.[36] Lee AK, Wagner BR, McPhillips K, et al. Locking compression pilon plate for fixation of comminuted posterior wall acetabular fractures: a novel technique. J Orthop Trauma. 2017;31(1):e32-36. [37] Kolp D, Ziebarth K, Slongo T. Rotation or derotation osteotomy of the tibia. Oper Orthop Traumatol. 2017;29(2):163-172. [38] Mcphillamy A, Gurnea TP, Moody AE, et al. The clinical and economic impact of generic locking plate utilization at a level II trauma center. J Orthop Trauma. 2016;30 Suppl 5:S32-36.[39] Vallier HA. Current evidence: plate versus lntramedullary nail for fixation of distal tibia fractures in 2016. J Orthop Trauma. 2016;30 Suppl 4:S2-6.[40] Augat P, Hoegel F, Stephan D, et al. Biomechanical effects of angular stable locking in intramedullary nails for the fixation of distal tibia fractures. Proc Inst Mech Eng H. 2016;230(11):1016-1023.[41] Switaj PJ, Fuchs D, Alshouli M, et al. A biomechanical comparison study of a modern fibular nail and distal fibular locking plate in AO/OTA 44C2 ankle fractures. J Orthop Surg Res. 2016;11(1):100. |
| [1] | Wei Guoqiang, Li Yunfeng, Wang Yi, Niu Xiaofen, Che Lifang, Wang Haiyan, Li Zhijun, Shi Guopeng, Bai Ling, Mo Kai, Zhang Chenchen, Xu Yangyang, Li Xiaohe. Biomechanical analysis of non-uniform material femur under different loads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1318-1322. |
| [2] | Zhang Yufang, Lü Meng, Mei Zhao. Construction and verification of a full spine biomechanical model of adolescent scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1351-1356. |
| [3] | Zhang Jichao, Dong Yuefu, Mou Zhifang, Zhang Zhen, Li Bingyan, Xu Xiangjun, Li Jiayi, Ren Meng, Dong Wanpeng. Finite element analysis of biomechanical changes in the osteoarthritis knee joint in different gait flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1357-1361. |
| [4] | Wen Mingtao, Liang Xuezhen, Li Jiacheng, Xu Bo, Li Gang. Mechanical stability of Sanders II type calcaneal fractures fixed by two internal fixation methods [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 838-842. |
| [5] | Wang Hailong, Li Long, Maihemuti·Yakufu, Chen Hongtao, Liu Xu, Yilihamu·Tuoheti. Finite element analysis of stress distribution of acetabular prosthesis in the Lewinnek safety zone [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 843-847. |
| [6] | Wei Bing, Chang Shan. Finite element analysis of different angles of nail placement in sagittal plane of spinal fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 864-869. |
| [7] | Li Guijun, Fang Xiaohui, Kong Weifeng, Yuan Xiaoqing, Jin Rongzhong, Yang Jun. Finite element analysis of the treatment of hallux valgus deformity by microplate combined with super strong suture elastic fixation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 938-942. |
| [8] | Baibujiafu·Yelisi, Renaguli·Maihemuti, Aizimaitijiang·Saiyiti, Wang Junxiang, Nijiati·Tuerxun. Stress analysis of maxillary central incisor crown implant restoration in different occlusal modes [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 567-572. |
| [9] | Wang Can, Gu Weiping, Jiang Yubin, Zhu Lin, Chen Gang. Finite element analysis of the influence of different implant designs on the stress of mandibular edentulous jaw [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 573-578. |
| [10] | Zhang Jianguo, Chen Chen, Hu Fengling, Huang Daoyu, Song Liang. Design and biomechanical properties of dental implant pore structure based on three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 585-590. |
| [11] | Lin Boying, Shen Mao. Biomechanical stability of endoscopic transforaminal lumbar interbody fusion with unilateral pedicle screw combined with contralateral translaminar facet screw fixation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 329-333. |
| [12] | Nie Wenzhong, Li Xiaoxuan, Zeng Jiayi, Shi Changqiang. Biomechanical changes in different implantation and fixation methods of lumbar fusion cage [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1505-1509. |
| [13] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [14] | Cai Qunbin, Zou Xia, Hu Jiantao, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei. Relationship between tip-apex distance and stability of intertrochanteric femoral fractures with proximal femoral anti-rotation nail: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 831-836. |
| [15] | Song Chengjie, Chang Hengrui, Shi Mingxin, Meng Xianzhong. Research progress in biomechanical stability of lateral lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 923-928. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||