Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (32): 5178-5183.doi: 10.3969/j.issn.2095-4344.2014.32.016
Previous Articles Next Articles
Effect of Toll-like receptor 4 on the immunological properties of periodontal ligament stem cells
Ding Gang, Wei Li-mei, Zhang Li, Tang Rui-ling
- Department of Stomatology, Yidu Central Hospital, Weifang Medical College, Qingzhou 262500, Shandong Province, China
-
Received:2014-06-17Online:2014-08-06Published:2014-09-18 -
Contact:Ding Gang, M.D., Associate professor, Associate chief physician, Department of Stomatology, Yidu Central Hospital, Weifang Medical College, Qingzhou 262500, Shandong Province, China -
About author:Ding Gang, M.D., Associate professor, Associate chief physician, Department of Stomatology, Yidu Central Hospital, Weifang Medical College, Qingzhou 262500, Shandong Province, China -
Supported by:the National Natural Science Foundation of China, No. 81070799; Research Awards Fund for Young and Middle-Aged Scientists in Shangdong Province, No. BS2010SW033
CLC Number:
Cite this article
Ding Gang, Wei Li-mei, Zhang Li, Tang Rui-ling. Effect of Toll-like receptor 4 on the immunological properties of periodontal ligament stem cells[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(32): 5178-5183.
share this article

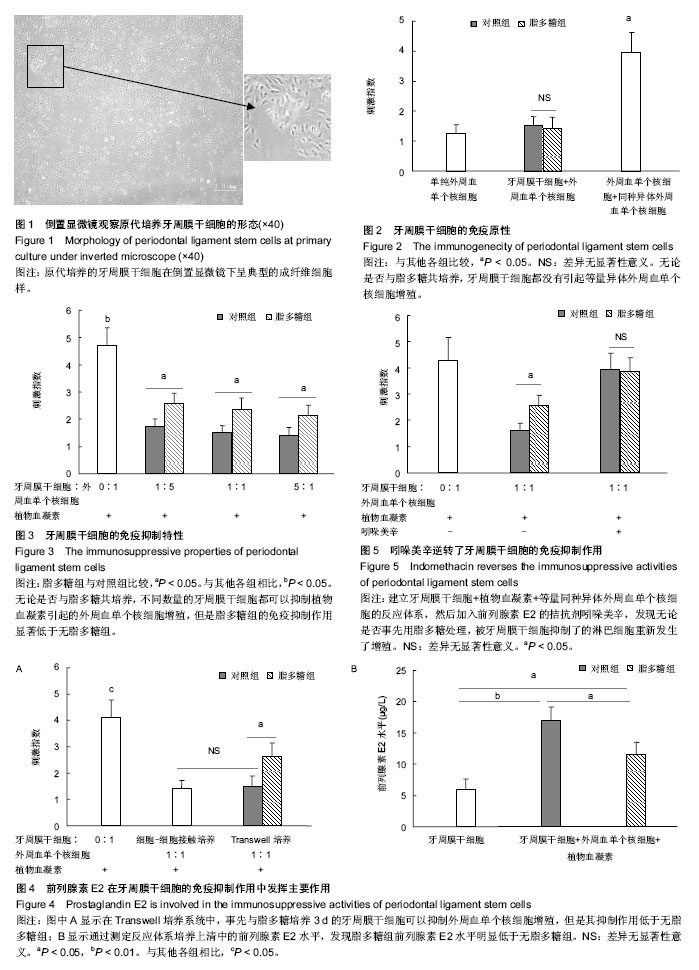
2.1 牙周膜干细胞的形态 原代培养的牙周膜干细胞较小,呈梭状的成纤维细胞样(图1)。传代后细胞生长旺盛,形态规则均一。 2.2 脂多糖对牙周膜干细胞的免疫原性没有影响 无论是否与脂多糖共培养,牙周膜干细胞都没有引起等量异体外周血单个核细胞增殖,而同种异体外周血单个核细胞共培养引起了明显的淋巴细胞增殖,说明脂多糖没有影响牙周膜干细胞的免疫原性(图2)。 2.3 牙周膜干细胞的免疫抑制作用减弱 植物血凝素能够刺激外周血单个核细胞增殖,无论是否事先用脂多糖处理,不同数量的牙周膜干细胞都可以抑制植物血凝素引起的外周血单个核细胞增殖,但是脂多糖组的免疫抑制作用显著低于无脂多糖组,说明脂多糖减弱了牙周膜干细胞的免疫抑制功能(图3)。 2.4 前列腺素E2的分泌减少 在Transwell培养系统中,事先与脂多糖培养3 d的牙周膜干细胞仍然可以抑制外周血单个核细胞增殖,但是其抑制作用低于无脂多糖组(图4A)。通过测定反应体系培养上清中的前列腺素E2水平,发现脂多糖组明显低于无脂多糖组(图4B)。 2.5 吲哚美辛恢复了外周血单个核细胞的增殖 进一步进行中和实验,先建立牙周膜干细胞+植物血凝素+等量同种异体外周血单个核细胞的反应体系,然后加入前列腺素E2的拮抗剂吲哚美辛,5 d后测定淋巴细胞的增殖情况。结果发现,无论是否事先用脂多糖处理,被牙周膜干细胞抑制了的淋巴细胞重新发生了增殖(图5)。"
| [1] West AP, Koblansky AA, Ghosh S.Recognition and signaling by toll-like receptors.Annu Rev Cell Dev Biol. 2006;22:409-437. [2] Miggin SM, O'Neill LA.New insights into the regulation of TLR signaling.J Leukoc Biol. 2006;80(2):220-226. [3] Cooper PR, Holder MJ, Smith AJ.Inflammation and regeneration in the dentin-pulp complex: a double-edged sword.J Endod. 2014;40(4 Suppl):S46-51. [4] Hwa Cho H, Bae YC, Jung JS.Role of toll-like receptors on human adipose-derived stromal cells.Stem Cells. 2006;24(12): 2744-2752. [5] Pevsner-Fischer M, Morad V, Cohen-Sfady M,et al. Toll-like receptors and their ligands control mesenchymal stem cell functions.Blood. 2007;109(4):1422-1432. [6] Yan H, Wu M, Yuan Y,et al.Priming of Toll-like receptor 4 pathway in mesenchymal stem cells increases expression of B cell activating factor.Biochem Biophys Res Commun. 2014; 448(2):212-217. [7] Mempel M, Voelcker V, Köllisch G,et al.Toll-like receptor expression in human keratinocytes: nuclear factor kappaB controlled gene activation by Staphylococcus aureus is toll-like receptor 2 but not toll-like receptor 4 or platelet activating factor receptor dependent.J Invest Dermatol. 2003; 121(6):1389-1396. [8] Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases.Lancet. 2005;366(9499):1809-1820. [9] Kinane DF, Marshall GJ.Periodontal manifestations of systemic disease.Aust Dent J. 2001;46(1):2-12. [10] Nemoto E, Honda T, Kanaya S,et al.Expression of functional Toll-like receptors and nucleotide-binding oligomerization domain proteins in murine cementoblasts and their upregulation during cell differentiation.J Periodontal Res. 2008;43(5):585-593. [11] Sakai A, Ohshima M, Sugano N,et al.Profiling the cytokines in gingival crevicular fluid using a cytokine antibody array.J Periodontol. 2006;77(5):856-864. [12] Song GG, Kim JH, Lee YH.Toll-like receptor (TLR) and matrix metalloproteinase (MMP) polymorphisms and periodontitis susceptibility: a meta-analysis.Mol Biol Rep. 2013;40(8): 5129-5141. [13] 曹采方. 牙周病学[M].2版.北京:人民卫生出版社,2003: 29-32. [14] Seo BM, Miura M, Gronthos S,et al.Investigation of multipotent postnatal stem cells from human periodontal ligament.Lancet. 2004;364(9429):149-155. [15] Ding G, Liu Y, Wang W,et al.Allogeneic periodontal ligament stem cell therapy for periodontitis in swine.Stem Cells. 2010; 28(10):1829-1838. [16] Liu O, Xu J, Ding G,et al.Periodontal ligament stem cells regulate B lymphocyte function via programmed cell death protein 1.Stem Cells. 2013;31(7):1371-1382. [17] Tang R, Wei F, Wei L,et al.Osteogenic differentiated periodontal ligament stem cells maintain their immunomodulatory capacity.J Tissue Eng Regen Med. 2014; 8(3):226-232. [18] Mohangi GU, Singh-Rambirich S, Volchansky A.Periodontal disease: Mechanisms of infection and inflammation and possible impact on miscellaneous systemic diseases and conditions.SADJ. 2013;68(10):462, 464-467. [19] Chamila Prageeth Pandula PK, Samaranayake LP, Jin LJ,et al. Periodontal ligament stem cells: an update and perspectives.J Investig Clin Dent. 2014;5(2):81-90. [20] Iwata T, Yamato M, Ishikawa I,et al.Tissue engineering in periodontal tissue.Anat Rec (Hoboken). 2014;297(1):16-25. [21] Park JY, Jeon SH, Choung PH.Efficacy of periodontal stem cell transplantation in the treatment of advanced periodontitis. Cell Transplant. 2011;20(2):271-285. [22] Seo BM, Miura M, Sonoyama W, et al. Recovery of stem cells from cryopreserved periodontal ligament.J Dent Res. 2005; 84(10):907-912. [23] Sonoyama W, Liu Y, Fang D,et al. Mesenchymal stem cell-mediated functional tooth regeneration in swine.PLoS One. 2006;1:e79. [24] Liu Y, Zheng Y, Ding G,et al.Periodontal ligament stem cell-mediated treatment for periodontitis in miniature swine. Stem Cells. 2008;26(4):1065-1073. [25] Feng F, Akiyama K, Liu Y,et al.Utility of PDL progenitors for in vivo tissue regeneration: a report of 3 cases. Oral Dis. 2010; 16(1):20-28. [26] Tse WT, Pendleton JD, Beyer WM, et al.Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation.Transplantation. 2003;75(3): 389-397. [27] Di Nicola M, Carlo-Stella C, Magni M,et al.Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli.Blood. 2002;99(10):3838-3843. [28] Bartholomew A, Sturgeon C, Siatskas M,et al. Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo.Exp Hematol. 2002; 30(1): 42-48. [29] Krampera M, Glennie S, Dyson J,et al. Bone marrow mesenchymal stem cells inhibit the response of naive and memory antigen-specific T cells to their cognate peptide. Blood. 2003;101(9):3722-3729. [30] 薛瑞,苗一非,杨吉春,等.前列腺素E2对免疫细胞及炎症相关疾病的调控作用[J].生理科学进展,2011,42(3):165-168. [31] Jarvinen L, Badri L, Wettlaufer S,et al. Lung resident mesenchymal stem cells isolated from human lung allografts inhibit T cell proliferation via a soluble mediator.J Immunol. 2008;181(6):4389-4396. [32] Prasanna SJ, Gopalakrishnan D, Shankar SR,et al. Pro-inflammatory cytokines, IFNgamma and TNFalpha, influence immune properties of human bone marrow and Wharton jelly mesenchymal stem cells differentially.PLoS One. 2010;5(2):e9016. [33] Hsu WT, Lin CH, Chiang BL,et al.Prostaglandin E2 potentiates mesenchymal stem cell-induced IL-10+IFN-γ+CD4+ regulatory T cells to control transplant arteriosclerosis.J Immunol. 2013;190(5):2372-2380. [34] Bouffi C, Bony C, Courties G,et al.IL-6-dependent PGE2 secretion by mesenchymal stem cells inhibits local inflammation in experimental arthritis.PLoS One. 2010;5(12): e14247. [35] Sreeramkumar V, Fresno M, Cuesta N.Prostaglandin E2 and T cells: friends or foes?Immunol Cell Biol. 2012;90(6): 579-586. [36] Burr SP, Dazzi F, Garden OA.Mesenchymal stromal cells and regulatory T cells: the Yin and Yang of peripheral tolerance. Immunol Cell Biol. 2013;91(1):12-18. [37] Aggarwal S, Pittenger MF.Human mesenchymal stem cells modulate allogeneic immune cell responses.Blood. 2005; 105(4):1815-1822. [38] Duffy MM, Ritter T, Ceredig R,et al.Mesenchymal stem cell effects on T-cell effector pathways.Stem Cell Res Ther. 2011; 2(4):34. [39] Svobodova E, Krulova M, Zajicova A,et al.The role of mouse mesenchymal stem cells in differentiation of naive T-cells into anti-inflammatory regulatory T-cell or proinflammatory helper T-cell 17 population.Stem Cells Dev. 2012;21(6):901-910. [40] Liu D, Xu J, Liu O,et al.Mesenchymal stem cells derived from inflamed periodontal ligaments exhibit impaired immunomodulation. J Clin Periodontol. 2012;39(12): 1174-1182. |
| [1] | Dang Yi, Du Chengyan, Yao Honglin, Yuan Nenghua, Cao Jin, Xiong Shan, Zhang Dingmei, Wang Xin. Hormonal osteonecrosis and oxidative stress [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1469-1476. |
| [2] | Li Xinyue, Li Xiheng, Mao Tianjiao, Tang Liang, Li Jiang. Three-dimensional culture affects morphology, activity and osteogenic differentiation of human periodontal ligament stem cells [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 846-852. |
| [3] | Wu Yujie, Wan Xiaofang, Wei Mianxing, Peng Shiyuan, Xu Xiaomei. Correlation between autophagy and the Hippo-YAP protein pathway in periodental ligament cells on the pressure side of a mouse model of orthodontic tooth movement [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 683-689. |
| [4] | Li Rui, Liu Zhen, Guo Zige, Lu Ruijie, Wang Chen. Aspirin-loaded chitosan nanoparticles and polydopamine modified titanium sheets improve osteogenic differentiation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 374-379. |
| [5] | Lu Di, Wan Xinyu, Yang Jinxin, Ding Kexin, Zhang Cheng, Duan Rongquan, Liu Zongxiang. Preparation and osteoinductive properties of tricalcium phosphate ceramics with submicron topology [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(16): 2473-2479. |
| [6] | Su Meng, Wang Xin, Zhang Jin, Bei Ying, Huang Yu, Zhu Yanzhao, Li Jiali, Wu Yan. Nanocellular vesicles loaded with curcumin promote wound healing in diabetic mice [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1877-1883. |
| [7] | Wang Zhaoxin, Nijati•Tursun, Dai Huijuan, Wang Junxiang, Xiaheida•Yilaljiang, Li Shuhui. Effect of macrophage inflammatory protein-1 alpha on the biological behavior of human periodontal ligament stem cells [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(10): 1521-1527. |
| [8] | Chen Jiana, Nie Minhai, Hu Xinyue, Liu Xuqian. Platelet-derived growth factor BB promotes proliferation and osteogenic differentiation of human periodontal ligament stem cells [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(10): 1534-1540. |
| [9] | Zhang Min, Bai Shulin, Li Shenghong, Fan Zhibo, Xie Yijia, Xu Xiaomei. Effects of high mobility group box 1 and ERK1/2 pathway on autophagy of human periodontal ligament cells under tensile stress [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(10): 1560-1566. |
| [10] | Ma Munan, Xie Jun, Sang Yuchao, Huang Lei, Zhang Guodong, Yang Xiaoli, Fu Songtao. Electroacupuncture combined with bone marrow mesenchymal stem cells in the treatment of chemotherapy-induced premature ovarian insufficiency in rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(1): 1-7. |
| [11] | Lan Qian, Gu Yangcong, Xiao Xin, Bi Xueting, Li Na. Human periodontal ligament stem cells-derived exosomes interfere with the proliferation and differentiation of MC3T3-E1 cells [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(1): 54-58. |
| [12] | Liu Wentao, Feng Xingchao, Yang Yi, Bai Shengbin. Effect of M2 macrophage-derived exosomes on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-6. |
| [13] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [14] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [15] | Huang Chenwei, Fei Yankang, Zhu Mengmei, Li Penghao, Yu Bing. Important role of glutathione in stemness and regulation of stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1119-1124. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||