Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (20): 3216-3223.doi: 10.3969/j.issn.2095-4344.2017.20.017
Previous Articles Next Articles
Gap arthroplasty versus interpositional arthroplasty for temporomandibular joint ankylosis: a Meta-analysis
Yishakejiang•Maimaiti1, Wu Jun1, Maimaitituxun•Tuerdi2
- 1Department of Alveolus Surgery, Urumqi Stomatological Hospital, Urumqi 830002, Xinjiang Uygur Autonomous Region, China; 2Department of Maxillofacial Trauma and Orthoganthic Surgery, the First Affiliated Hospital of Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous Region, China
-
Revised:2017-02-11Online:2017-07-18Published:2017-07-28 -
Contact:Maimaitituxun?Tu’erdi, M.D., Associate chief physician, Associate professor, Master’s supervisor, Department of Maxillofacial Trauma and Orthoganthic Surgery, the First Affiliated Hospital of Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous Region, China -
About author:Yishakejiang?Maimaiti, Master, Attending physician, Department of Alveolus Surgery, Urumqi Stomatological Hospital, Urumqi 830002, Xinjiang Uygur Autonomous Region, China -
Supported by:the Open Project of Key Laboratory of Xinjiang Medical Animal Model Research, No. XJDX1103-2013-05
CLC Number:
Cite this article
Yishakejiang•Maimaiti, Wu Jun, Maimaitituxun•Tuerdi. Gap arthroplasty versus interpositional arthroplasty for temporomandibular joint ankylosis: a Meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(20): 3216-3223.
share this article

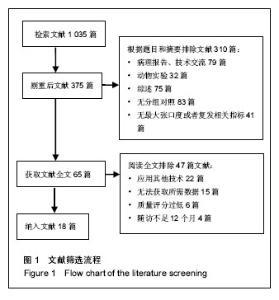
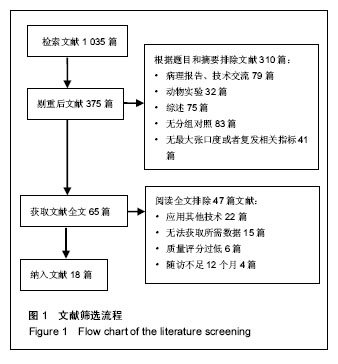
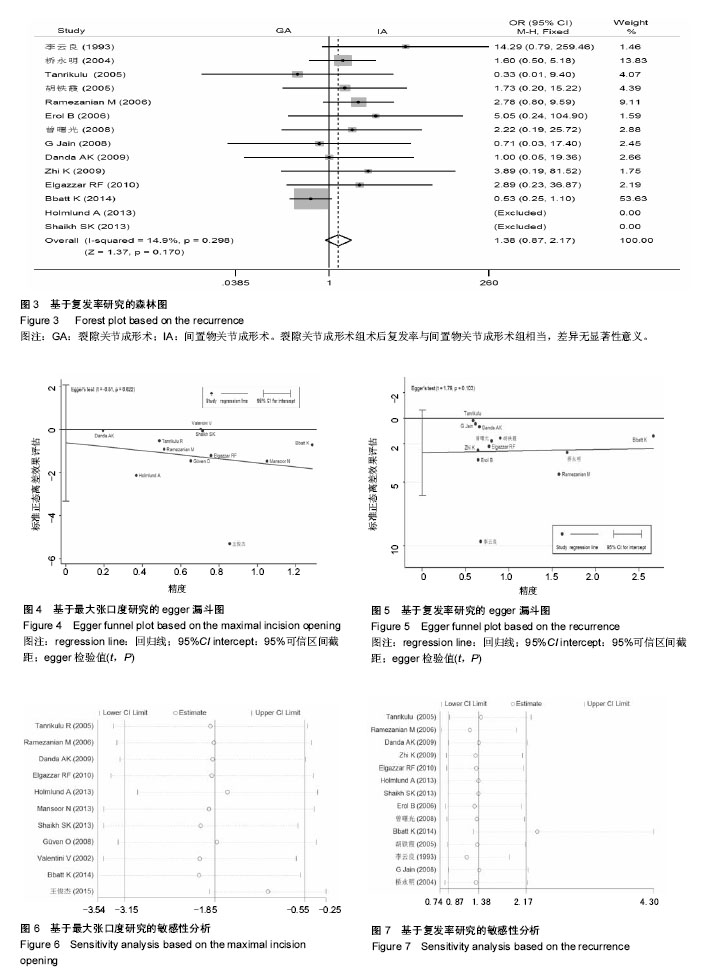
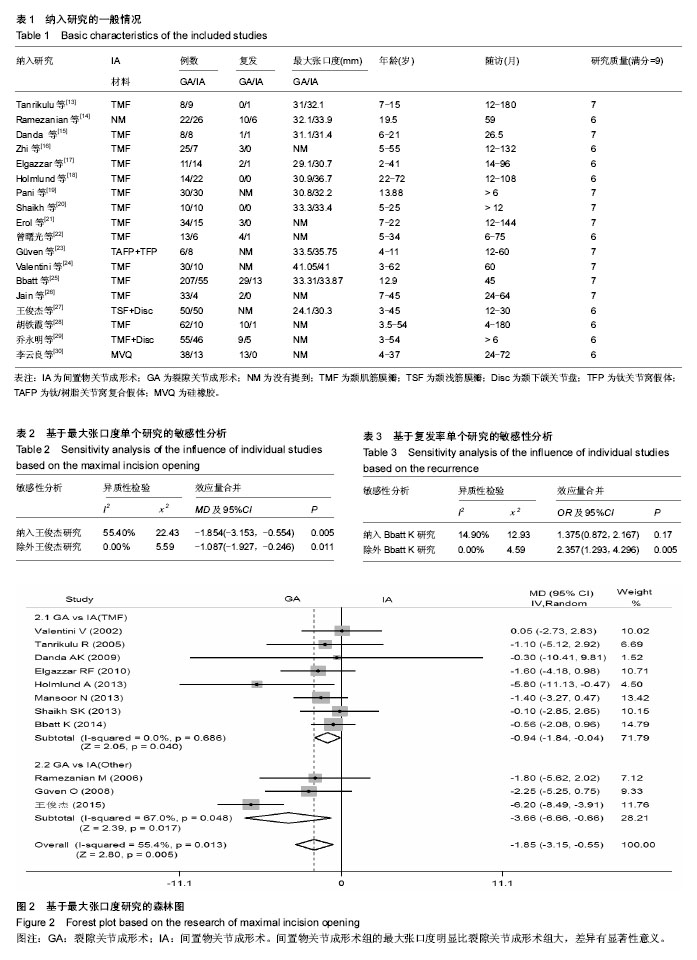
2.2 纳入研究的基本特征与质量评价 纳入研究的基本特征以及质量评分结果均见表1。其中13篇研究应用了颞肌筋膜瓣(temporomandibular myofascial flap,TMF)作为间置物材料。 NOS量表评分结果显示:在病例选择方面,18个研究均基本符合标准,组间可比性与结果评价方面,9个研究均较好。 2.3 Meta分析结果 2.3.1 最大张口度 共纳入11个研究[13-15,17-20,23-25,27],638例患者。随机效应模式Meta分析结果显示,间置物关节成形术组的最大张口度明显比裂隙关节成形术组大,且差异有显著性意义,研究资料有中度异质性[MD=-1.85,95%CI:(-3.15,-0.55),Z=2.80,P=0.005,I2=55.4%]。以间置材料不同,分颞肌筋膜瓣组和其他材料组进行亚组分析,其分析结果显示间置物关节成形术组的最大张口度明显比裂隙关节成形术组大,且差异有显著性意义,具体值为颞肌筋膜瓣组:[ MD= -0.94,95%CI:(-1.84,-0.04),Z=2.05,P=0.040,I2=0.0%];其他材料组:[MD= -3.36,95%CI:(-6.66,-0.66),Z=2.39,P=0.017,I2=67.0%],见图2。 2.3.2 复发 共纳入14个研究[13-18,20-22,25-26,28-30],885例患者。固定效应模式Meta分析结果显示,裂隙关节成形术组术后复发率与间置物关节成形术组相当,差异无显著性意义,研究资料不存在异质性,具体值为[OR=1.38,95%CI:(0.87,2.17),Z=1.37,P=0.170,I2=14.9%],见图3。 2.4 发表偏倚分析 对最大张口度和复发率指标均进行发表偏倚检测,egger检验结果显示:最大张口度组t=0.51, P,复发率组t=1.79,P=0.103,表明最大张口度和复发率指标上,Meta分析结果无明显的发表偏倚,见图4,5。=0.622 2.5 敏感性分析 基于最大张口度单个研究的分析结果显示:王俊杰等[27]的研究对Meta分析合并后总异质性检验有明显的影响,如果删除它,合并后的异质性检验结果由I2=55.4%,χ2=22.43,P=0.005变为I2=0.0%,χ2= 5.59,P=0.011,但是对于效应量合并后的结果无显著影响。基于复发率单个研究的分析结果示:Bbatt等[25]的研究对总合并后的异质性检验无影响,但是对总的合并效应量有一定的影响,如果删除它,合并效应量由1.375(0.872,2.167),P=0.170变为2.357(1.293,4.296),P=0.005,由差异无显著性意义变为差异有显著性意义。其余研究资料对Meta分析合并效应量结果未见明显影响(图6,7和表2,3)。"
| [1] Akama MK, Guthua S, Chindia ML, et al. Management of bilateral temporomandibular joint ankylosis in children: case report. East Afr Med J. 2009;86(1):45-48. [2] Babu L, Jain MK, Ramesh C, et al. Is aggressive gap arthroplasty essential in the management of temporomandibular joint ankylosis?-a prospective clinical study of 15 cases. Br J Oral Maxillofac Surg. 2013;51(6): 473-478.[3] Sidebottom AJ, Salha R. Management of the temporomandibular joint in rheumatoid disorders. Br J Oral Maxillofac Surg. 2013;51(3):191-198.[4] Thangavelu A, Santhosh Kumar K, Vaidhyanathan A, et al. Versatility of full thickness skin-subcutaneous fat grafts as interpositional material in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2011;40(1):50-56.[5] Su-Gwan K. Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. Int J Oral Maxillofac Surg. 2001;30(3):189-193.[6] Ortak T, Ulusoy MG, Sungur N, et al. Silicon in temporomandibular joint ankylosis surgery. J Craniofac Surg. 2001;12(3):232-236.[7] Akhtar MU, Abbas I, Ali Shah A. Use of silastic as interpositional material in the management of unilateral temporomandibular joint ankylosis. J Ayub Med Coll Abbottabad. 2006;18(2):73-76.[8] Katsnelson A, Markiewicz MR, Keith DA, et al. Operative management of temporomandibular joint ankylosis: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2012;70(3):531-536.[9] Salins PC. New perspectives in the management of cranio-mandibular ankylosis. Int J Oral Maxillofac Surg. 2000; 29(5):337-340.[10] Mehrotra D, Pradhan R, Mohammad S, et al. Random control trial of dermis-fat graft and interposition of temporalis fascia in the management of temporomandibular ankylosis in children. Br J Oral Maxillofac Surg. 2008;46(7):521-526.[11] Vasconcelos BC, Bessa-Nogueira RV, Cypriano RV. Treatment of temporomandibular joint ankylosis by gap arthroplasty. Med Oral Patol Oral Cir Bucal. 2006;11(1): E66-69.[12] Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 20009;283(15): 2008-2012.[13] Tanrikulu R, Erol B, Görgün B, et al. The contribution to success of various methods of treatment of temporomandibular joint ankylosis (a statistical study containing 24 cases). Turk J Pediatr. 2005;47(3):261-265.[14] Ramezanian M, Yavary T. Comparison of gap arthroplasty and interpositional gap arthroplasty on the temporomandibular joint ankylosis. Acta Medica Iranica. 2006; 44(6): 391-394.[15] Danda AK, S R, Chinnaswami R. Comparison of gap arthroplasty with and without a temporalis muscle flap for the treatment of ankylosis. J Oral Maxillofac Surg. 2009;67(7): 1425-1431.[16] Zhi K, Ren W, Zhou H, et al. Management of temporomandibular joint ankylosis: 11 years' clinical experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(5):687-692.[17] Elgazzar RF, Abdelhady AI, Saad KA, et al. Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg. 2010;39(4):333-342.[18] Holmlund A, Lund B, Weiner CK. Mandibular condylectomy with osteoarthrectomy with and without transfer of the temporalis muscle. Br J Oral Maxillofac Surg. 2013;51(3): 206-210.[19] Pani SC, Mubaraki SA, Ahmed YT, et al. Parental perceptions of the oral health-related quality of life of autistic children in Saudi Arabia. Spec Care Dentist. 2013;33(1):8-12.[20] Shaikh SK,Mishra M,Tiwari AK,et al. Comparative evaluation of gap arthroplasty and interpositional arthroplasty using temporalis fascia in the management of temporomandibular joint ankylosis. Journal of Orofacial Research. 2013; 3(3): 170-174.[21] Erol B, Tanrikulu R, Görgün B. A clinical study on ankylosis of the temporomandibular joint. J Craniomaxillofac Surg. 2006; 34(2):100-106.[22] 曾曙光,吴世卿,艾伟健,等.手术治疗颞下颌关节强直34例效果观察[J].广东医学, 2008, 29(7):1206-1207.[23] Güven O. A clinical study on temporomandibular joint ankylosis in children. J Craniofac Surg. 2008;19(5): 1263-1269.[24] Valentini V, Vetrano S, Agrillo A, et al. Surgical treatment of TMJ ankylosis: our experience (60 cases). J Craniofac Surg. 2002;13(1):59-67.[25] Bhatt K, Roychoudhury A, Bhutia O, et al. Functional outcomes of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 2014;72(12):2434-2439.[26] Jain G, Kumar S, Rana AS, et al. Temporomandibular joint ankylosis: a review of 44 cases. Oral Maxillofac Surg. 2008; 12(2):61-66.[27] 王俊杰. 裂隙式关节成形术、关节盘复位+关节成形术治疗单侧颞下颌关节强直的长期疗效比较[J]. 医学理论与实践, 2015, 28(7): 851-852.[28] 胡铁霞,李祖兵,于永红,等.175例颞下颌关节强直手术治疗回顾性分析[J].中华整形外科杂志,2005,21(6):408-411.[29] 乔永明,龙星,程勇,等. 颞下颌关节强直的手术方法与复发[J]. 口腔颌面外科杂志, 2005, 14(4): 338-341.[30] 李运良,陈运美.不同手术方法治疗颞下颌关节强直疗效评价[J]. 口腔颌面外科杂志, 1993,2(1): 10-12.[31] Topazian RG. Gap versus interposition arthroplasty for ankylosis of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(4):388-389.[32] Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48(11):1145-1151.[33] Matsuura H, Miyamoto H, Ogi N, et al. The effect of gap arthroplasty on temporomandibular joint ankylosis: an experimental study. Int J Oral Maxillofac Surg. 2001;30(5): 431-437.[34] Güven O. A clinical study on temporomandibular joint ankylosis. Auris Nasus Larynx. 2000;27(1):27-33.[35] Ma J, Liang L, Jiang H, et al. Gap Arthroplasty versus Interpositional Arthroplasty for Temporomandibular Joint Ankylosis: A Meta-Analysis. PLoS One. 2015;10(5): e0127652.[36] Balaji SM. Modified temporalis anchorage in craniomandibular reankylosis. Int J Oral Maxillofac Surg. 2003;32(5):480-485.[37] Bajpai H, Saikrishna D. The versatility of temporalis myofascial flap in maxillo-facial reconstruction: a clinical study. J Maxillofac Oral Surg. 2011;10(1):25-31. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [3] | Zhang Lichuang, Xu Hao, Ma Yinghui, Xiong Mengting, Han Haihui, Bao Jiamin, Zhai Weitao, Liang Qianqian. Mechanism and prospects of regulating lymphatic reflux function in the treatment of rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1459-1466. |
| [4] | Jing Jinpeng, Zhang Yue, Liu Xiaomin, Liu Yi. Traditional Chinese medicine injection for promoting blood circulation in prevention of deep vein thrombosis after orthopedic surgery: network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1467-1476. |
| [5] | Wu Min, Zhang Yeting, Wang Lu, Wang Junwei, Jin Yu, Shan Jixin, Bai Bingyi, Yuan Qiongjia. Effect of concurrent training sequences on body composition and hormone response: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1305-1312. |
| [6] | Liu Gang, Ma Chao, Wang Le, Zeng Jie, Jiao Yong, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Ankle-foot orthoses improve motor function of children with cerebral palsy: a Meta-analysis based on 12 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1299-1304. |
| [7] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [8] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [9] | Huang Hao, Hong Song, Wa Qingde. Finite element analysis of the effect of femoral component rotation on patellofemoral joint contact pressure in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 848-852. |
| [10] | Yuan Jing, Sun Xiaohu, Chen Hui, Qiao Yongjie, Wang Lixin. Digital measurement and analysis of the distal femur in adults with secondary knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 881-885. |
| [11] | Zhou Jianguo, Liu Shiwei, Yuan Changhong, Bi Shengrong, Yang Guoping, Hu Weiquan, Liu Hui, Qian Rui. Total knee arthroplasty with posterior cruciate ligament retaining prosthesis in the treatment of knee osteoarthritis with knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 892-897. |
| [12] | Liu Yiyi, Qiu Junqiang, Yi Longyan, Zhou Cailiang. Effect of resistance training on interleukin-6 and C-reactive protein in middle-age and elderly people: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 804-812. |
| [13] | Wang Nan, Qian Yuzhang, Xie Lin. Network Meta-analysis of different acupuncture methods for the treatment of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 813-820. |
| [14] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [15] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||