Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (47): 7119-7126.doi: 10.3969/j.issn.2095-4344.2016.47.018
Previous Articles Next Articles
Influence of Gluma desensitizing agents on dentin bond strength: a Meta-analysis
- 1Department of Prosthodonitics, Affiliated Hospital of Stomatology, Southwest Medical University, Luzhou 646000, Sichuan Province, China; 2Department of Preventive Medicine, Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Received:2016-09-08Online:2016-11-18Published:2016-11-18 -
Contact:Guo Ling, Associate professor, Master’s supervisor, Department of Preventive Medicine, Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Li Wang-yang, Studying for master’s degree, Department of Prosthodonitics, Affiliated Hospital of Stomatology, Southwest Medical University, Luzhou 646000, Sichuan Province, China -
Supported by:the Project of Sichuan Provincal Department of Education, China, No. 11ZB128
CLC Number:
Cite this article
Li Wang-yang, Zhang Ling, Zhang Hui, Li Ai-ling, Guo Ling. Influence of Gluma desensitizing agents on dentin bond strength: a Meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(47): 7119-7126.
share this article

2.3 风险评估结果 通过Cochrane风险偏倚评估工具评估,纳入文献均排除高风险偏倚。17项评估项目中选择偏倚(随机序列产生)高风险为5%,不清楚40%,低风险为55%;选择偏倚(分配隐藏)高风险为5%,不清楚32.5%,低风险为62.5%;实施偏倚(受试者盲法)高风险为20%,不清楚50%,低风险为30%;测试偏倚(对结果评估的盲法)高风险为0%,不清楚10%,低风险为90%;失访偏倚(数据结果完全)高风险为5%,不清楚10%,低风险为85%;报告偏倚(选择性报告)高风险为0%,不清楚5%,低风险为95%;其他偏倚高风险为0%,不清楚50%,低风险为50%;纳入文献具体风险评估情况见图3。"

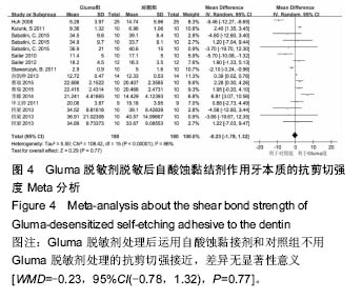
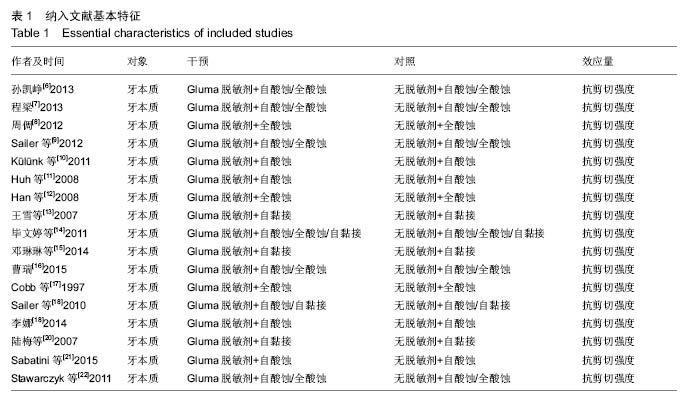
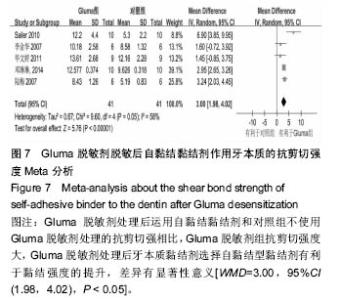
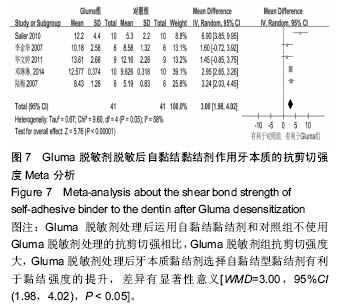
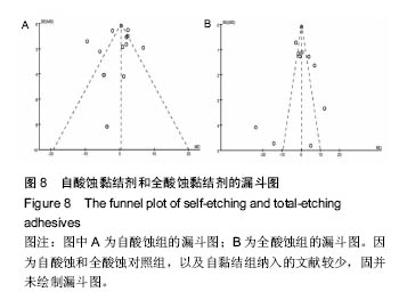
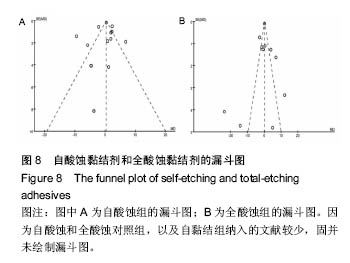
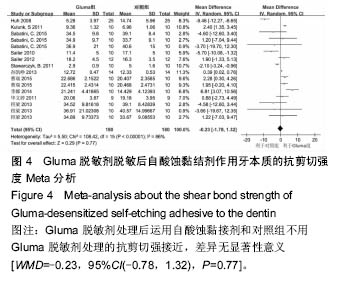
2.4 Meta分析结果 2.4.1 自酸蚀黏结剂对黏结效果的影响 自酸蚀组中,共有11篇文章,其中16个研究符合纳入标准,共有180个样本。结果表明有2个研究中使用Gluma脱敏剂对牙本质后自酸蚀黏接剂强度抗剪切强度大于对照组;有3个研究中表明使用Gluma脱敏剂对牙本质后自酸蚀黏接剂强度抗剪切强度小于对照组;另外,11个研究与无效线相交。Meta分析结果异质性高达86%,最后结果P=0.77,差异无显著性意义。异质性检验χ2=108.42, P < 0.000 01),合并效应量WMD采用随机效应模型,WMD的合并效应量(total)为-0.23,其95%CI为(-1.78, 1.32),合并效应量的检验Z=0.29,P=0.77。根据此结果分析异质性可能存在的原因。纳入的文献中Külünk等[10]、Huh等[11]、李娜[19]、Stawarczyk等[22]的4个研究产生了较大的异质性。若排除这4个研究,异质性则可以降到36%。自酸蚀组中,Sabatini等[21]和程梁[7]均对自酸蚀黏结剂Opti Bond和XenoIV进行分析,结果均是未使用Gluma脱敏剂的对照组比使用Gluma脱敏剂的黏结剂的实验组抗剪切强度大,但是差异无显著性意义。孙凯峥[6]和李娜[19]同时对AdperTMEasy自酸蚀剂进行研究,结果是使用Gluma脱敏剂可以增强牙本质黏结的抗剪切强度。其他研究因为品牌不同会有细微的差别[6,10,21-22],但是主体成分和原理是相近的(图4)。"
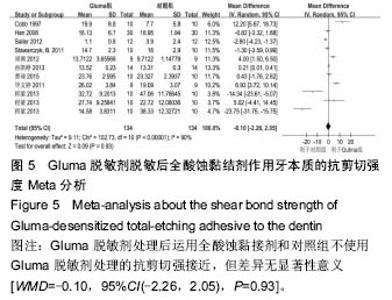
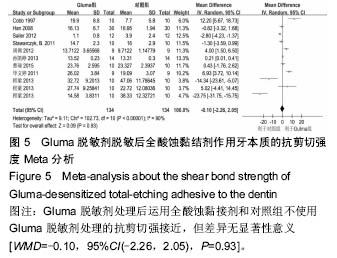
2.4.2 全酸蚀黏结剂对黏结效果的影响 全酸蚀组中,共9篇文章,其中11个研究符合纳入标准,共有134个样本。结果表明有3个研究中使用Gluma脱敏剂对牙本质后全酸蚀黏接剂强度抗剪切强度大于对照组;有3个研究中表明使用Gluma脱敏剂对牙本质后全酸蚀黏接剂强度抗剪切强度小于对照组;另外,5个与无效线相交。Meta分析结果异质性为90%,最后结果P=0.93,差异无显著性意义。异质性检验χ2=102.73,P < 0.000 01,合并效应量WMD采用随机效应模型,WMD的合并效应量(total)为-0.10,其95%CI为(-2.26,2.05),合并效应量的检验Z=0.09,P=0.93。根据此结果分析异质性可能存在的原因,主要是因为Cobb等[17]中Gluma脱敏剂对牙本质后全酸蚀黏接剂强度抗剪切强度明显大于对照组(图5)。"
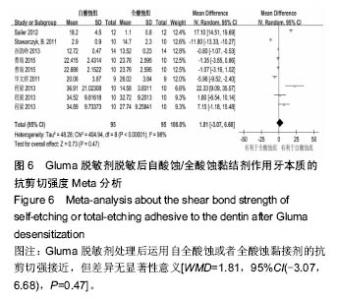
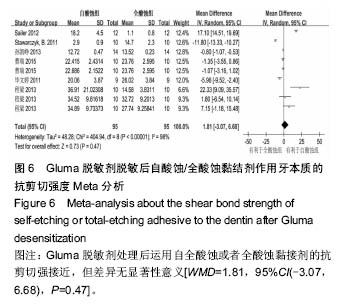
2.4.3 自酸蚀与全酸蚀黏结剂对黏结效果的影响 Gluma脱敏剂对牙本质脱敏后应用自酸蚀和全酸蚀黏结剂的抗剪强度对比,符合纳入标准的文献有6篇,9个研究,63个样本。其中有2个研究表明Gluma脱敏剂对牙本质后自酸蚀黏接剂强度抗剪切强度大于全酸蚀; 有2个研究中表明使用Gluma脱敏剂对牙本质后自酸蚀黏接剂强度抗剪切强度小于全酸蚀组,另外,5个研究与无效线相交。 Meta分析结果异质性为98%,异质性检验χ2= 404.94,P < 0.000 01,合并效应量WMD采用随机效应模型,WMD的合并效应量(total)为1.81,其95%CI为(-3.07,6.68),合并效应量的检验Z=0.73,P=0.47。根据此结果分析异质性可能存在的原因,主要是因为Cobb等[17]中Gluma脱敏剂对牙本质后全酸蚀黏接剂强度抗剪切强度明显大于对照组。Sailer等[18]和程梁[7]的研究中,自酸蚀组明显大于全酸蚀组(图6)。"
| [1]Bhatia S, Krishnaswamy MM. Effect of two different dentin desensitizers on shear bond strength of two different bonding agents to dentin: an in vitro study. Indian J Dent Res. 2012;23(6):703-708. [2]Shafiei F, Memarpour M, Doozandeh M. Effect of oxalate desensitizer on the bonding durability of adhesive resin cements to dentin. J Prosthodont Res. 2012;56(3):187-193. [3]Silva SM, Malacarne-Zanon J, Carvalho RM, et al. Effects of potassium oxalate on knoop hardness of etch-and-rinse adhesives. Oper Dent. 2012;37(4):356-362. [4]Di Hipólito V, Rodrigues FP, Piveta FB, et al. Effectiveness of self-adhesive luting cements in bonding to chlorhexidine-treated dentin. Dent Mater. 2012;28(5):495-501. [5]Can-Karabulut DC, Karabulut B. The effect of dentin hypersensitivity treatments on the shear bond strength to dentin of a composite material. Gen Dent. 2011; 59(1): e12-17. [6]孙凯峥.抗菌剂在基托树脂中应用的研究进展[J].西南军医,2012,14(6):879-882. [7]程梁.三种脱敏剂对牙本质粘接强度影响的实验研究[D].长春:吉林大学,2013. [8]周倜.牙本质脱敏剂对粘结材料粘结强度的影响[D].长春:吉林大学,2012. [9]Sailer I, Oendra AE, Stawarczyk B,et al. The effects of desensitizing resin, resin sealing, and provisional cement on the bond strength of dentin luted with self-adhesive and conventional resincements. J Prosthet Dent. 2012;107(4):252-260. [10]Külünk S, Saraç D, Külünk T, et al. The effects of different desensitizing agents on the shear bond strength of adhesive resin cement to dentin. J Esthet Restor Dent. 2011;23(6):380-387. [11]Huh JB, Kim JH, Chung MK, et al. The effect of several dentin desensitizers on shear bond strength of adhesive resin luting cement using self-etching primer. J Dent. 2008;36(12):1025-1032. [12]Han XY, Zhu HS, Liu QY. Effect of different treatments of dentin surface on sheer bond strength between different bonding agents and dentin. Hua Xi Kou Qiang Yi Xue Za Zhi. 2008;26(2):125-128. [13]王雪,李金华,牟建钢,等.脱敏剂封闭牙本质小管的微结构特征及其对树脂粘接剂粘接强度的影响[J].华西口腔医学杂志,2008,26(3):233-236. [14][14] 毕文婷,高平,陈利民,等.不同脱敏方法对牙本质表面微结构形态及树脂粘接剂粘接力的影响[J].实用口腔医学杂志,2011,27(1):88-91. [15]邓琳琳,王璐,邱雨,等.脱敏及脱敏后酸蚀对牙本质与氧化锆粘结强度的影响[J].重庆医科大学学报, 2014(12): 1763-1766. [16]曹瑞.Gluma脱敏剂对牙本质粘接界面纳米渗漏和剪切强度的影响[D].石家庄:河北医科大学,2015. [17]Cobb DS, Reinhardt JW, Vargas MA. Effect of HEMA-containing dentin desensitizers on shear bond strength of a resin cement. Am J Dent. 1997;10(2):62-65. [18]Sailer I, Tettamanti S, Stawarczyk B, et al. In vitro study of the influence of dentin desensitizing and sealing on the shear bond strength of two universal resin cements. J Adhes Dent. 2010;12(5):381-392. [19]李娜.三种衬垫材料对自酸蚀粘接剂剪切强度和窝洞边缘封闭性的影响[D].石家庄:河北医科大学,2014. [20]陆梅,高宁,岑远坤,等.Gluma脱敏剂对不同粘接剂粘接拉伸和剪切强度的影响[J].山东大学学报(医学版), 2007, 45(6):629-631. [21]Sabatini C, Wu Z. Effect of Desensitizing Agents on the Bond Strength of Mild and Strong Self-etching Adhesives. Oper Dent. 2015;40(5):548-557. [22]Stawarczyk B, Hartmann R, Hartmann L, et al. The effect of dentin desensitizer on shear bond strength of conventional and self-adhesive resin luting cements after aging. Oper Dent. 2011;36(5):492-501. [23]Ding M, Shin SW, Kim MS, et al. The effect of a desensitizer and CO2 laser irradiation on bond performance between eroded dentin and resin composite. J Adv Prosthodont. 2014;6(3):165-170. [24]Kobler A, Schaller HG, Gernhardt CR. Effects of the desensitizing agents Gluma and Hyposen on the tensile bond strength of dentin adhesives. Am J Dent. 2008;21(6):388-392. [25]Akca T, Yazici AR, Celik C, et al. The effect of desensitizing treatments on the bond strength of resin composite to dentin mediated by a self-etching primer. Oper Dent. 2007;32(5):451-456. [26]Maeda FA, Fukushima KA, Tedesco TK, et al. Effect of erosive challenge and Nd:YAG laser irradiation on bond strength of adhesive systems to dentin. Int J Adh Adhes. 2016;64:60-64. [27]Makkar S, Goyal M, Kaushal A, et al. Effect of desensitizing treatments on bond strength of resin composites to dentin - an in vitro study. J Conserv Dent. 2014;17(5):458-461. [28]Hong S, Park N, Park Y, et al. The effects of desensitizing agents, bonding resin and tooth brushing on dentin permeability, in vitro. J Korean Acad Prosthodont. 2014;52(3):165-176. [29]Jia R, Lu Y, Yang CW, et al. Effect of generation 4.0 polyamidoamine dendrimer on the mineralization of demineralized dentinal tubules in vitro. Arch Oral Biol. 2014;59(10):1085-1093. [30]Pei D, Liu S, Huang C, et al. Effect of pretreatment with calcium-containing desensitizer on the dentin bonding of mild self-etch adhesives. Eur J Oral Sci. 2013;121(3 Pt 1):204-210. [31]Cortiano FM, Rached RN, Mazur RF, et al. Effect of desensitizing agents on the microtensile bond strength of two-step etch-and-rinse adhesives to dentin. Eur J Oral Sci. 2016;124(3):309-315. [32]Sengun A, Koyuturk AE, Sener Y, et al. Effect of desensitizers on the bond strength of a self-etching adhesive system to caries-affected dentin on the gingival wall. Oper Dent. 2005;30(4):430-435. [33]Shafiei F, Alavi AA, Karimi F, et al. Effects of oxalate desensitizer with different resin cement-retained indirect composite inlays on fracture resistance of teeth. J Prosthodont. 2013;22(4):268-274. [34]Chermont AB, Carneiro KK, Lobato MF, et al. Clinical evaluation of postoperative sensitivity using self-etching adhesives containing glutaraldehyde. Braz Oral Res. 2010;24(3):349-354. |
| [1] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [2] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [5] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [6] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [7] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [8] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [9] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [10] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [11] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [12] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [13] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [14] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [15] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||