Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (27): 4310-4317.doi: 10.3969/j.issn.2095-4344.2014.27.009
Previous Articles Next Articles
Individualized treatment prevents patient-prosthesis mismatch after aortic valve replacement with small aortic annulus
Han Jin-song1, Wang Hui-shan1, Yin Zong-tao1, Wang Ting-ting2, Han Hong-guang1, Song Heng-chang1, Jin Yan1
- 1 Department of Cardiovascular Surgery, 2 Library, General Hospital of Shenyang Military Area Command of Chinese PLA, Shenyang 110016, Liaoning Province, China
-
Online:2014-06-30Published:2014-06-30 -
Contact:Wang Hui-shan, M.D., Chief physician, Professor, Doctoral supervisor, Department of Cardiovascular Surgery, General Hospital of Shenyang Military Area Command of Chinese PLA, Shenyang 110016, Liaoning Province, China -
About author:Han Jin-song, Studying for doctorate, Associate chief physician, Department of Cardiovascular Surgery, General Hospital of Shenyang Military Area Command of Chinese PLA, Shenyang 110016, Liaoning Province, China
CLC Number:
Cite this article
Han Jin-song, Wang Hui-shan, Yin Zong-tao, Wang Ting-ting, Han Hong-guang, Song Heng-chang, Jin Yan . Individualized treatment prevents patient-prosthesis mismatch after aortic valve replacement with small aortic annulus[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(27): 4310-4317.
share this article

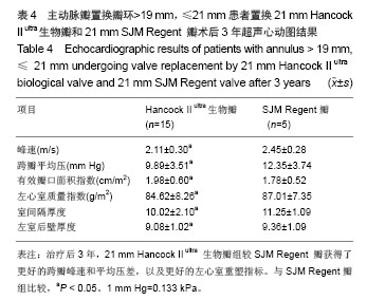
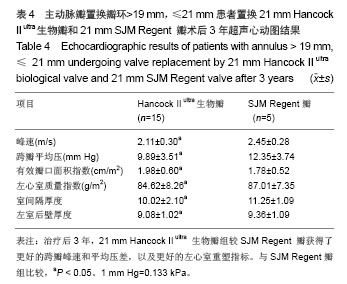
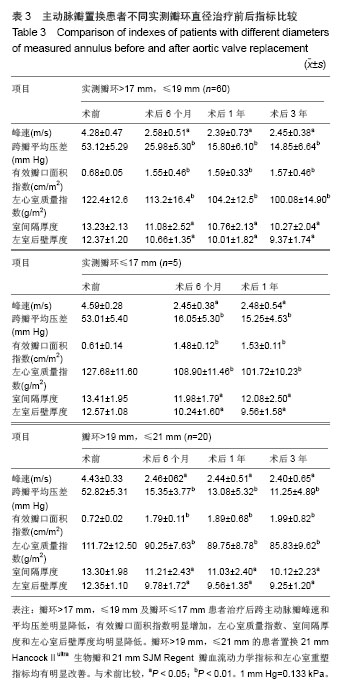
2.3 随访结果 81例获随访,随访时间为6个月-3年,其中瓣环≤17 mm的患者随访1年,余组最长随访3年。NYHA心功能分级Ⅰ级65例,Ⅱ级16例。 瓣环>17 mm,≤19 mm的患者治疗后效果:治疗后6个月、治疗后1年和治疗后3年,跨主动脉瓣峰速和平均压差明显降低,有效瓣口面积指数明显增加,左心室重量指数、室间隔厚度和左心室后壁厚度均明显降低(表3)。 瓣环≤17 mm的患者治疗后效果:治疗后6个月和术后1年,跨主动脉瓣峰速和平均压差明显降低,有效瓣口面积指数明显增加,左心室重量指数、室间隔厚度和左心室后壁厚度均明显降低(表3)。未发生牛心包补片的不良反应。 瓣环>19 mm,≤21 mm的患者治疗后效果:置换 21 mm Hancock II ultra生物瓣和21 mm SJM Regent瓣血流动力学指标和左心室重塑指标均明显改善(表3),而再对两种瓣膜组间比较提示,治疗后3年,21 mm Hancock II ultra生物瓣组较SJM Regent瓣获得了更好的跨瓣峰速和平均压差,以及更好的左心室重塑指标(表4)。"
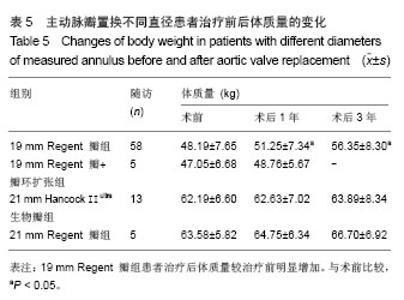
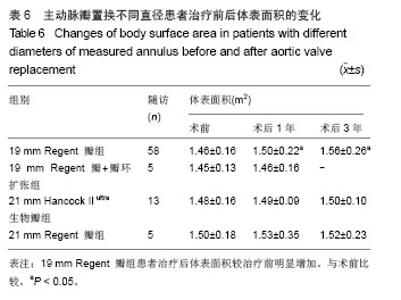
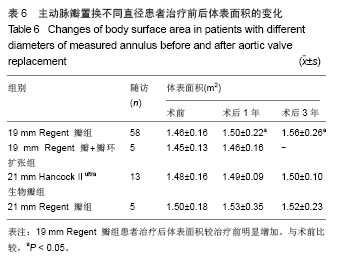
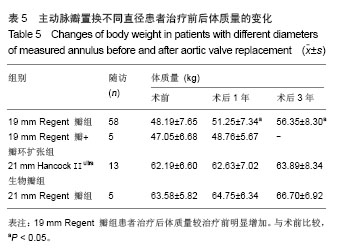
体质量和体表面积的变化:19 mm Regent瓣组治疗后较治疗前明显增加(P < 0.05),其余组比较差异无显著性意义(表5,6)。其中1例置换19 mm Regent瓣的患者,治疗后半年体质量增加到70 kg(治疗前为50 kg),复查超声心动图示有效瓣口面积指数为0.70 cm2/m2,有活动量受限的表现,瞩患者合理饮食、控制体质量,3个月后再次复查超声心动图示有效瓣口面积指数为1.20 cm2/m2,患者运动耐力明显改善,随访至今无不适症状。 2.4 并发症及不良反应 并发症情况:瓣环直径>17 mm,≤19 mm组60例中,治疗后发生低心排综合征1例、二次开胸止血1例。瓣环直径≤17 mm组5例中,治疗后发生低心排综合征1例和呼吸机依赖(呼吸机辅助时间>72 h)1例。瓣环直径>19 mm,≤21 mm组20例中,治疗后出现肺内感染1例、呼吸机依赖1例和气胸1例。所有患者均未出现脑栓塞或脑出血等脑部并发症。 不良反应情况:无瓣膜功能失调或卡瓣。未发现牛心包补片撕裂、瘤样膨出、钙化、血栓形成、免疫反应和感染等情况。"
| [1]Svensson LG, Adams DH, Bonow RO, et al.Aortic valve and ascending aorta guidelines for management and quality measures. Ann Thorac Surg.2013;95(6 Suppl):S1-S66.
[2]David TE. Surgical treatment of aortic valve disease. Nat Rev Cardiol.2013;10(7):375-386.
[3]Bianco JC, Qizilbash B, Carrier M, et al.Is patient-prosthesis mismatch a perioperative predictor of long-term mortality after aortic valve replacement?. J Cardiothorac Vasc Anesth. 2013; 27(4):647-653.
[4]李先华,徐志云,曹翔.环上瓣植入与瓣环扩大在成人小主动脉瓣环换瓣术中的应用效果观察[J].山东医药,2011,51(6):90-92.
[5]Ghosh P, Kumar S, Pandey S, et al. Small aortic annulus: a functional definition. Ann Thorac Cardiovasc Surg.1998; 4(5): 251-261.
[6]Peterson MD, Borger MA, Feindel CM, et al. Aortic annular enlargement during aortic valve replacement:improving results with time.Ann Thorac Surg.2007; 83(6):2044-2049.
[7]David TE, Uden DE. Aortic valve replacement in adult patients with small aortic annuli.Ann Thorac Surg.1983;36(5):577-583.
[8]Ghavidel AA, Omrani G, Chitsazan M, et al. Long-term results of aortic valve replacement with posterior root enlargement. Asian Cardiovasc Thorac Ann.2014 Mar 25. [Epub ahead of print]
[9]Coutinho GF, Correia PM, Paupério G, et al.Aortic root enlargement does not increase the surgical risk and short-term patient outcome? Eur J Cardiothorac Surg.2011;40(2):441-447.
[10]Wang B, Yang H, Wang T, et al.Impact of obesity on long-term survival after aortic valve replacement with a small prosthesis. Interact CardioVasc Thorac Surg.2013;17(1):66-72.
[11]Shrestha M, Maeding I, Höffler K, et al. Aortic valve replacement in geriatric patients with small aortic roots: are sutureless valves the future? Interact Cardiovasc Thorac Surg. 2013;17(5):778-782.
[12]Urbanski PP, Dinstak W, Rents W, et al.Long-term results after aortic root replacement using self-assembled valve composite grafts in patients with small aortic annulus. Interact Cardiovasc Thorac Surg.2014;18(2):159-163.
[13]Rahimtoola SH. The problem of valve prosthesis-patient mismatch. Circulation.1978;58(1):20-24.
[14]Minardi G, Manzara C, Creazzo V, et al. Evaluation of 17-mm St.Jude medical regent prosthetic aortic heart valves by rest and dobutamine stress echocardiography. J Cardiothorac Surg. 2006;1(1):27.
[15]Mohty D, Malouf JF, Girard SE, et al.Impact of prosthesis–patient mismatch on long-term survival in patients with small St Jude Medical mechanical prostheses in the aortic position. Circulation.2006;113(3):420-426.
[16]Pibarot P, Dumesnil JG. Prosthesis-patient mismatch: definition, clinical impact, and prevention. Heart.2006;92(8):1022-1029.
[17]Mohty D, Dumesnil JG, Echahidi N, et al. Impact of prosthesispatient mismatch on long-term survival after aortic valve replacement: influence of age, obesity, and left ventricular dysfunction. J Am Coll Cardiol.2009;53(1):39-47.
[18]Walther T, Rastan A, Falk V, et al. Patient prosthesis mismatch affects short- and long-term outcomes after aortic valve replacement. Eur J Cardiothorac Surg.2006;30(1):15-19.
[19]Ardal H, Toker ME, Rabu? MB, et al. Does aortic root enlargement impair the outcome of patients with small aortic root? J Card Surg.2006;21(5):449-453.
[20]Finkelstein A, Schwartz AL, Uretzky G, et al. Hemodynamic performance and outcome of percutaneous versus surgical stentless bioprostheses for aortic stenosis with anticipated patient-prosthesis mismatch.J Thorac Cardiovasc Surg.2013. pii: S0022-5223(13)00768-X. doi: 10.1016/j.jtcvs.2013.07.008. [Epub ahead of print].
[21]Chacko SJ, Ansari AH, McCarthy PM, et al. Prosthesis-patient mismatch in bovine pericardial aortic valves:evaluation using 3 different modalities and associated medium-term outcomes. Circ Cardiovasc Imaging.2013; 6(5):776-783.
[22]Urso S, Sadaba R, Aldamiz-Echevarria G.Is patient-prosthesis mismatch an independent risk factor for early and mid-term overall mortality in adult patients undergoing aortic valve replacement? Interact CardioVasc Thorac Surg. 2009;9(3):510-518.
[23]Mannacio VA, De Amicis V, Di Tommaso L, et al. Influence of prosthesis-patient mismatch on exercise-induced arrhythmias: a further aspect after aortic valve replacement.J Thorac Cardiovasc Surg.2009;138(3):632-638.
[24]Bridges CR, O’Brian SM, Cleveland JC, et al. Association between indices of prosthesis internal orifice size and operative mortality after isolated aortic valve replacement. J Thorac Cardiovasc Surg.2007;133(4):1012-1021.
[25]Kohsaka S, Mohan S, Variani S, et al. Prosthesis-patient mismatch affects long-term survival after mechanical valve replacement. J Thorac Cardiovasc Surg.2008;135(5):1076-1080.
[26]Konno S, Imai Y, Iida Y, et al.A new method for prosthetic valve replacement in congenital aortic stenosis associated with hypoplasia of the aortic ring. J Thorac Cardiovasc Surg. 1975;70(5):909-917.
[27]Manouguian S, Seybold-Epting W. Patch enlargement of the aortic valve ring by extending the aortic incision into the anterior mitral leaflet. J Thorac Cardiovasc Surg.1979;78(3): 402-412.
[28]Dhareshwar J, Sundt TM 3rd, Dearani JA, et al. Aortic root enlargement: what are the operative risks? J Thorac Cardiovasc Surg.2007;134(4):916-924.
[29]Kulik A, Al-Saigh M, Chan V, et al. Enlargement of the small aortic root during aortic valve replacement: is there a benefit? Ann Thorac Surg.2008;85(1):94-100.
[30]Celiento M, Saccocci M, De Martino A, et al.Stability of aortic annulus enlargement during aortic valve replacement using a bovine pericardial patch: an 18-year clinical, echocardiographic, and angio-computed tomographic follow-up. J Thorac Cardiovasc Surg.2014;147(3):977-983.
[31]Prakash S, Agarwal S, Dutta N, et al. A comparative study of surgical treatment of small aortic root with or without aortic root enlargement using a single prosthesis type. J Cardiovasc Med (Hagerstown).2010;11(11):836-842.
[32]夏冰,文冰,许华山,等.自体心包补片修补主动脉瓣环辅助主动脉瓣置换[J].中国组织工程研究,2013,17(5):761-768.
[33]Penaranda JG, Greason KL, Pislaru SV, et al. Aortic Root Enlargement in Octogenarian Patients Results in Less Patient Prosthesis Mismatch. Ann Thorac Surg.2014 Mar 18. pii: S0003-4975(13)02813-0.
[34]庞中一, 李继勇. 十九毫米主动脉瓣环机械瓣置换80例中期效果分析[J].中国组织工程研究与临床康复,2008,12(35):6888-6890.
[35]王亮,王晓明,韩志伟,等. 17-mm Regent瓣治疗狭小主动脉瓣环患者术后临床观察[J].中国心血管病研究,2010,8(9):648-649.
[36]苗齐,刘兴荣,马国涛,等. St.Jude Medical Regent主动脉瓣应用于小主动脉瓣环患者的初步经验[J].中国心血管病研究,2006, 4(6):404-406.
[37]赵东,王春生,洪涛,等.小主动脉瓣环患者应用Regent机械瓣术后心功能变化的评价[J].复旦学报(医学版),2006,33(2): 251-253.
[38]于涛,谢定雄,董燕.CarboMedics Top Hat Supra-Annular Aortic机械瓣在小主动脉瓣环成年患者中的应用[J].中国组织工程研究与临床康复,2008,12(9):1632-1634.
[39]陈卫民,王奇,刘媛.小主动脉瓣环患者应用ATS.AP瓣置换20例效果分析[J].中国临床新医学,2010,3(12):1235-1237.
[40]申红亚.人工瓣膜置换对血流动力学影响的系统分析[J].中国组织工程研究与临床康复,2009,13(26):5141-5144.
[41]Nouette K, Richeb6 P, Calderon J, et al. Perioperative anticOagulatiOn management for prosthetic heart valves. Ann Fr Aneslh Reanim.2005;24(6):621-631.
[42]褚衍林,李鲁,吴英渝,等.风湿性心脏瓣膜替换术后远期疗效观察[J].中国循环杂志,2006,21(2):140-142.
[43]尹宗涛,王辉山,汪曾炜,等.Hancock II Ultra生物瓣行主动脉置换术后早期患者的血流动力学评价[J].中华胸心血管外科杂志, 2011,27(12):720-723.
[44]Flameng W, Herregods MC, Vercalsteren M, et al. Prosthesis-patient mismatch predicts structural valve degeneration in bioprosthetic heart valves. Circulation. 2010; 121(19):2123-2129.
[45]Shrestha M, Folliguet T, Meuris B, et al. Sutureless Perceval S aortic valve replacement: a multicenter prospective pilot trial. J Heart Valve Dis.2009;18(6):698-702.
[46]Villa E, Messina A, Cirillo M, et al. Perceval sutureless valve in freestyle root: new surgical valve-in-valve therapy. Ann Thorac Surg.2013;96(6):e155-e157.
[47]Wu Z, Cao H, Zhu D, et al.Replacement of the st jude medical regent valve in the aortic position with a continuous suture technique in the small aortic root. J Card Surg.2014;29(2):170-174.
[48]Kitamura T, Torii S, Hanayama N, et al. Moderate prosthesis-patient mismatch may be negligible in elderly patients undergoing conventional aortic valve replacement for aortic stenosis. Int Heart J.2013;54(1):11-14.
[49]Kato Y, Hattori K, Motoki M, et al. Optimal results of aortic valve replacement with small mechanical valves (< 19 mm). J Heart Valve Dis.2013;22(4):468-475. |
| [1] | Yang Xin, Jin Zhe, Feng Xu, Lu Bing. The current situation of knowledge and attitudes towards organ, eye tissue, body donation of residents in Shenyang [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 779-784. |
| [2] |
Ma Chao, Wang Huishan, Han Jinsong, Yin Zongtao, Zhang Xiling.
Cardiac valve prosthesis implantation and surgical maze ablation for the treatment of valvular disease with atrial fibrillation [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(28): 4580-4587. |
| [3] | Peng Xianjiang1, Liu Bozhi2, Duan Haifeng1, Yang Qianzi1, Hu Sheng1 . Anesthesia management for aortic valve plus mitral valve replacement in Small-Tailed Han sheep [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(7): 1052-1056. |
| [4] | Yin Peiyong, Cui Xiaohong, Xiong Ting, Li Sufang, He Ximin. Efficacy of transcatheter aortic vavle repalcement and surgical aortic vavle replacement for aortic stenosis: a Meta analysis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(30): 4905-4912. |
| [5] | Cai Qiucheng, Fan Hongkai, Xiong Rihui, Jiang Yi. Intravenous administration of bone marrow mesenchymal stem cells protects liver function following fatty liver transplantation from donors after cardiac death [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(17): 2625-2629. |
| [6] | Zhu Hongwei, Yuan Quan, Liu Xingming, Cong Hua. Fluid structure interaction analysis of transcatheter aortic valve implantation [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(10): 1599-1604. |
| [7] | Jiang Shanshan, Wang Feng, Yu Limei. Immunomodulatory properties of mesenchymal stem cells and their application in organ transplantation [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(1): 103-109. |
| [8] | Liu Teng-fei, Zhou Jian-kang, Huang Tuan-jie, Xing Qu, Cheng Kang, Li Peng, Li Dong-peng, Yang Bo, Ma Shan-shan, Guan Fang-xia . MG53 protein protects against multiorgan ischemia/reperfusion injury: present and future [J]. Chinese Journal of Tissue Engineering Research, 2017, 21(20): 3248-3254. |
| [9] | Li Ling, Li Ning, Ai Zi-ye, Yao Ya-jun, Wei Wan-hui, He Wei-yang, Wang Yan-feng, Ye Qi-fa. Intra-patient variability of tacrolimus concentration in transplant recipients: a prognostic predictor post transplantation [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(49): 7437-7422. |
| [10] | Lin Jing-xia, Su Fan, Luo Hong-shan. Transfusion of blood components in liver transplantation and abdominal multiple organ transplantation [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(33): 4957-4962. |
| [11] | Dong Jian-hui, Li Hai-bin, Sun Xu-yong, Qin Ke, Liao Ji-xiang, Li Mei-si, Huang Xiao-dan, Huang Chen, Huang Ying, Cao Song, Gao Zhao, Li Zhuang-jiang, Nie Feng, Yang Jian-jun. Clinical effects of renal transplantation with kidneys from donors dying of organophosphate poisoning [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(29): 4311-4318. |
| [12] | Zhang Wen-xin, Teng Sha, Peng Xiao, Lin Xiao-hong, Liu Hong-xia. Systematic review of the effects of education on medical students’ knowledge and attitudes toward organ donation and transplantation [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(5): 810-814. |
| [13] | Hu Xiao-yan, Wang Yan-feng, Ye Qi-fa, Chen Zhi-quan, Fan Xiao-li, Guo Yi, Li Ning. Effects of hypothermic machine perfusion versus static cold storage of kidney allografts on transplant outcomes: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(42): 6882-6888. |
| [14] | Zhang Li-ping, Bai Jian. Cytomegalovirus nosocomial infection following organ transplantation: detection and monitoring [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(20): 3258-3263. |
| [15] | Cao Cui-ping, Huang Hai. Construction strategy of human organ donation social mission system in China [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(2): 300-304. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||