Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (12): 2265-2272.doi: 10.3969/j.issn.2095-4344.2013.12.025
Previous Articles Next Articles
Fibrovascularization of different types of hydroxyapatite orbital implants
Wang Xing-li, Liu He-nan, Chen Xiao-long
- Department of Ophthalmology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China
-
Received:2012-12-29Revised:2013-02-19Online:2013-03-19Published:2013-03-19 -
Contact:Chen Xiao-long, Chief physician, Professor, Doctoral supervisor, Department of Ophthalmology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China chenxlcmu@126.com -
About author:Wang Xing-li★, Studying for master’s degree, Department of Ophthalmology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China wangxingli1988@126.com
CLC Number:
Cite this article
Wang Xing-li, Liu He-nan, Chen Xiao-long. Fibrovascularization of different types of hydroxyapatite orbital implants[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(12): 2265-2272.
share this article
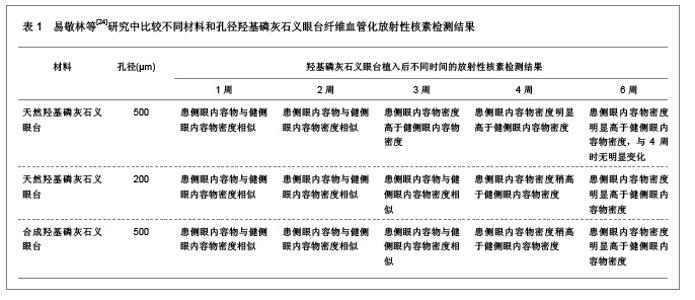
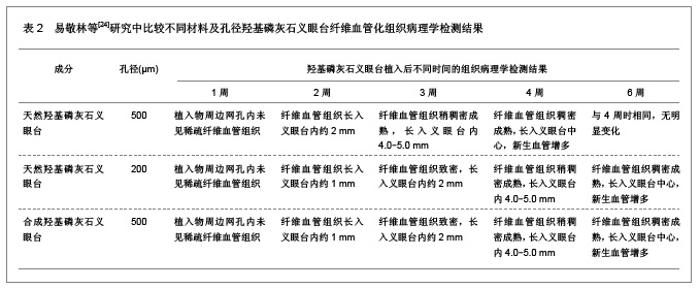
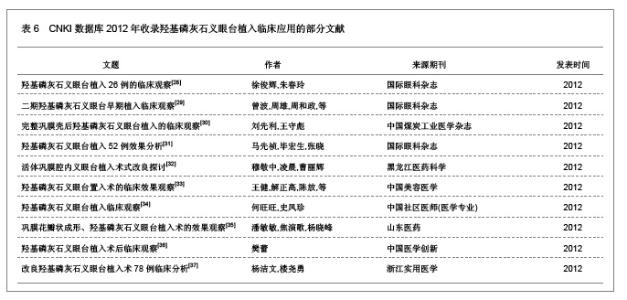
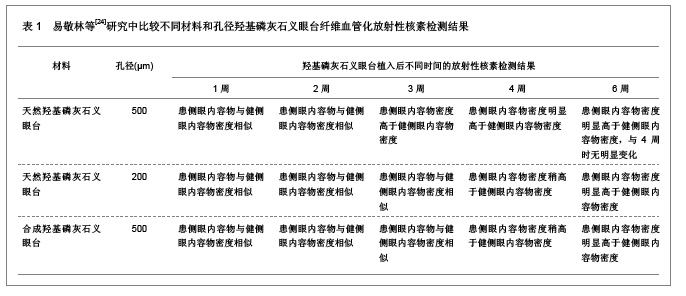
2.1 羟基磷灰石义眼台纤维血管化的检测方法 2.1.1 CT检测羟基磷灰石义眼台纤维血管化 CT是检测眼部疾病常用的方法之一。Sires等[12]提出骨或类似无机物的异体材料可应用定量CT检测其密度的大小,根据这一应用特点,可用定量CT检测羟基磷灰石义眼台的密度,从而预测羟基磷灰石义眼台植入后的纤维血管化程度。但是,Potter等[13]研究认为,CT检测羟基磷灰石义眼台纤维血管化程度与其它检测方法相比较并不占明显的优势,由于羟基磷灰石的物理化学性质以及生物性能,即使应用增强CT进行扫描检测,羟基磷灰石义眼台植入后的密度与眶骨密度重叠,无法增加羟基磷灰石义眼台植入6个月后纤维血管化的发现率。因此,CT不常应用于羟基磷灰石纤维血管化程度的检测。 2.1.2 超声检测羟基磷灰石义眼台纤维血管化 超声在眼内及眼眶疾病的检测已经较为成熟,尤其对眼眶疾病的检测显示出其特有的优势。夏利等[14]在研究中发现,羟基磷灰石义眼台植入早期,纤维血管组织只是长入义眼台植入物周边包围义眼台,而未长入其孔隙内,应用二维超声检测仅见强回声带,彩色多普勒血流显像检测也不能分辨此时的血流信号是来自眼外肌还是结膜血管系统,义眼台植入后7个月,植入物内部的血流信号则明显增加,可延伸至义眼台内部,并能测得典型的动脉血流频谱,说明血管已长入其内,并建立了微循环。但是,Potter等[13]研究认为,在单独使用超声或彩色多普勒血流显像时,随着声波进入植入物的衰减,羟基磷灰石义眼台纤维血管化的程度不易分辨,而且彩色多普勒血流显像的分辨率低,衰减率大,不能很好地显示羟基磷灰石义眼台内部的静脉血流情况。因此,超声在羟基磷灰石义眼台纤维血管化程度的检测应用中受到一定的限制。 2.1.3 MRI检测羟基磷灰石义眼台纤维血管化 MRI影像检测是一种无创伤的检测方法,MRI检测软组织的对比度较好、分辨力强、无骨性伪影干扰。20世纪90年代初,增强MRI被用于羟基磷灰石义眼台纤维血管化程度的检测评估[15]。Klapper等[16]根据MRI检测信号的强弱分布将羟基磷灰石义眼台植入后的纤维血管化程度增强MRI检测显像分为5级,当MRI检测信号显著均匀分布的即为5级,表明羟基磷灰石已完全血管化。众多研究显示,MRI检测可清晰显示羟基磷灰石义眼台在不同时期的纤维血管化程度,是羟基磷灰石义眼台植入后纤维血管化程度理想的检测方法[17-18]。 2.1.4 放射性核素显像检测羟基磷灰石义眼台纤维血管化 放射性核素显像可提供完善准确的信息,研究显示植入羟基磷灰石义眼台1个月后即有眼内容物的放射性分布增强,8个月后眼内容物的放射性明显增强,表明眶内纤维血管长入植入物孔隙内[19-20]。放射性核素显像检测操作简单、方便,是羟基磷灰石义眼台纤维血管化常用的检测方法。 2.2 不同材料和孔径的羟基磷灰石义眼台纤维血管化检测的研究 羟基磷灰石义眼台植入眼眶后,周围的纤维结缔组织沿义眼台孔隙逐渐深入,并长入其中,此过程即为义眼台植入物的纤维血管化[21]。羟基磷灰石义眼台纤维血管化的程度和速度与孔隙的大小和义眼台的直径相关[22]。一般情况下,直径为20-22 mm的义眼台需要6个月或更长时间才能完全血管化,而直径为12-14 mm的义眼台仅需要一两个月即可以完成血管化[23]。易敬林等[24]对天然羟基磷灰石义眼台和人工合成羟基磷灰石义眼台以及不同孔径大小的义眼台纤维血管化的速度进行了比较,结果发现天然羟基磷灰石义眼台比相同孔径大小的人工合成羟基磷灰石义眼台纤维血管化的速度快,并且对于天然羟基磷灰石义眼台而言,孔径越大,纤维血管化的速度越快,具体结果见表1,2。"
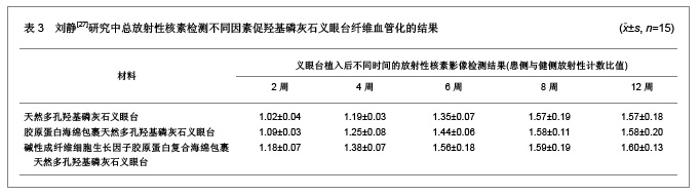
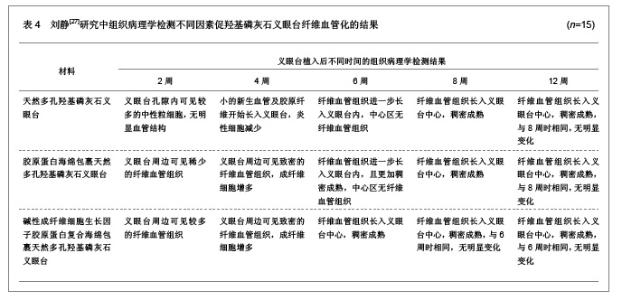
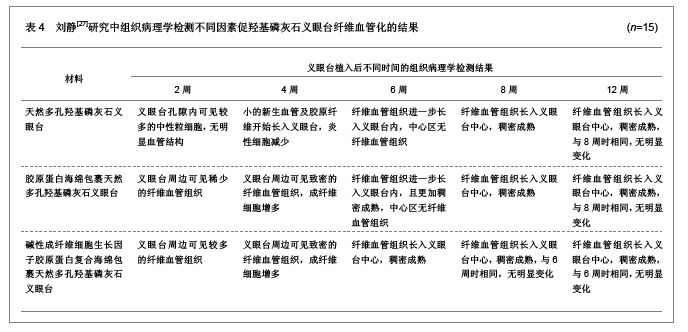
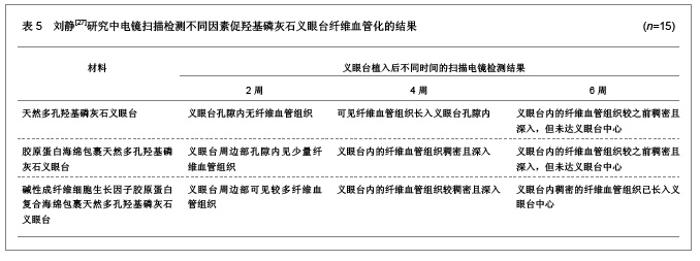
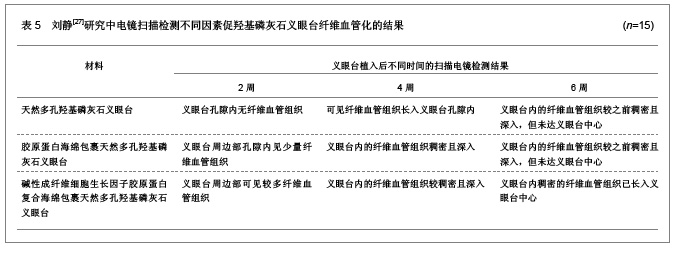
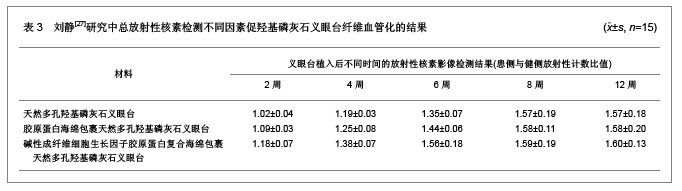
张虹等[25]通过应用不同的植入方法比较羟基磷灰石义眼台纤维血管化的程度,将36只大白兔随机分为4组,每组9只,分别进行羟基磷灰石义眼台半巩膜壳内植入、羟基磷灰石义眼台多孔巩膜壳内植入、羟基磷灰石义眼台全巩膜壳内植入和羟基磷灰石义眼台巩膜瓣遮盖肌锥内植入,植入后分别进行放射性核素和组织病理学检测观察,结果发现羟基磷灰石义眼台植入后1周和2周,各组之间纤维血管化程度无明显差异,植入后4周和6周时半巩膜壳内植入、多孔巩膜壳内植入和巩膜瓣遮盖肌锥内植入义眼台纤维血管化程度明显高于全巩膜壳内植入义眼台的纤维血管化程度,植入后8周时,各组之间植入义眼台纤维血管化程度无明显差异。植入后8周时的组织病理学检测结果显示半巩膜壳内植入义眼台纤维血管化程度为98%,多孔巩膜壳内植入义眼台纤维血管化程度为100%,全巩膜壳内植入义眼台纤维血管化程度为97%,巩膜瓣遮盖肌锥内植入义眼台纤维血管化程度为98%。通过实验分析可以发现羟基磷灰石义眼台多孔巩膜壳内植入是最理想的植入方式,可以使羟基磷灰石义眼台的纤维血管化程度达到100%。 樊建中等[26]通过MRI检测评估羟基磷灰石义眼台纤维血管化的程度,实验结果发现,羟基磷灰石义眼台植入后2周,义眼台周边可见带状强化影,植入后3周时强化影向中心扩大,植入后5,6周时羟基磷灰石义眼台均完全纤维血管化。组织病理学检测结果显示,羟基磷灰石义眼台植入后2周时,纤维血管组织长入义眼台1.0-2.0 mm,植入后4周时,可见纤维血管组织长入义眼台中心,第6周时,羟基磷灰石义眼台完全血管化。 2.3 碱性成纤维细胞生长因子胶原蛋白复合海绵对羟基磷灰石义眼台的促纤维血管化作用 刘静[27]通过应用放射性核素显像检测、组织病理学检测以及电镜扫描检测等方法研究了碱性成纤维细胞生长因子胶原蛋白复合海绵促进羟基磷灰石义眼台纤维血管化的作用,具体结果见表3-5。"
| [1] Perry AC. Advances in enucleation. ophthalmol clin North Am. 1991;4(2):173-182.[2] Albiar E. Hydroxyapatite implants--a new trend in enucleation and orbital reconstructive surgery. Insight. 1992;17(1):25-28. [3] Bi X, Zhou H, Lin M, et al. One-stage replacement surgery of orbital implants with noninfectious complications. J Craniofac Surg. 2012;23(2):e146-149. [4] Mawn LA, Jordan DR, Gilberg S. Proliferation of human fibroblasts in vitro after exposure to orbital implants. Can J Ophthalmol. 2001;36(5):245-251.[5] 仲元奎.羟基磷灰石义眼台Ⅰ期植入18例临床报告[J].眼外伤职业眼病杂志,2005,27(2):137-138.[6] 王晓琴,刘剑萍,聂尚武,等.羟基磷灰石义眼座的临床应用观察[J].中国实用眼科杂志,2005,23(6):628-629.[7] 何庆华,宋琛,马玉龙.羟基磷灰石植入物眼窝成形术[J].中华眼科杂志,1997,33(3):219-221.[8] Massry GG, Holds JB. Coralline hydroxyapatite spheres as secondary orbital implants in anophthalmos. Ophthalmology. 1995;102(1):161-166. [9] Soparkar CN, Wong JF, Patrinely JR, et al. Porous polyethylene implant fibrovascularization rate is affected by tissue wrapping, agarose coating, and insertion site. Ophthal Plast Reconstr Surg. 2000;16(5):330-336. [10] Kirzhner M, Shildkrot Y, Haik BG, et al. Pediatric Anophthalmic Sockets and Orbital Implants: Outcomes with Polymer-Coated Implants. Ophthalmology. 2013.[11] 中国知网.中国学术期刊总库[DB/OL].2013-1-10. https://www.cnki.net[12] Sires BS, Holds JB, Archer CR. Variability of mineral density in coralline hydroxyapatite spheres: study by quantitative computed tomography. Ophthal Plast Reconstr Surg. 1993; 9(4):250-253. [13] De Potter P, Shields CL, Shields JA, et al. Role of magnetic resonance imaging in the evaluation of the hydroxyapatite orbital implant. Ophthalmology. 1992;99(5):824-830. [14] 夏利,向慧娟,林利,等.彩色多普勒超声对羟基磷灰石眶内植入体的观察[J].中华超声影像学杂志,2001,10(3):191.[15] 刘静,廖洪斐.多孔羟基磷灰石义眼台血管化程度的检测方法[J].中国美容整形外科杂志,2007,18(2):134-136.[16] Klapper SR, Jordan DR, Ells A, et al. Hydroxyapatite orbital implant vascularization assessed by magnetic resonance imaging. Ophthal Plast Reconstr Surg. 2003;19(1):46-52. [17] Sarvananthan N, Liddicoat AJ, Fahy GT. Synthetic hydroxyapatite orbital implants: a clinical and MRI evaluation. Eye (Lond). 1999;13 ( Pt 2):205-208.[18] Spirnak JP, Nieves N, Hollsten DA, et al. Gadolinium-enhanced magnetic resonance imaging assessment of hydroxyapatite orbital implants. Am J Ophthalmol. 1995;119(4):431-440.[19] 陈蔷娟,万腊根.102例国产羟基磷灰石眼窝填充术的疗效评价与SPECT观察[J].中国实用眼科杂志,1997,15(2):102-104.[20] 陈璟,吴华,李贵刚,等.99Tcm-MDP显像对羟基磷灰石义眼台血管化的评估[J].中华核医学杂志,2005,25(2):111-112.[21] Galluzzi P, De Francesco S, Giacalone G, et al. Contrast-enhanced magnetic resonance imaging of fibrovascular tissue ingrowth within synthetic hydroxyapatiteorbital implants in children. Eur J Ophthalmol. 2011;21(5):521-528. [22] Rubin PA, Popham JK, Bilyk JR, et al. Comparison of fibrovascular ingrowth into hydroxyapatite and porous polyethylene orbital implants. Ophthal Plast Reconstr Surg. 1994;10(2):96-103. [23] Nasser QJ, Blaydon SM, Connor MA, et al. Re: "comparison of the exposure rate of wrapped hydroxyapatite (Bio-Eye) versus unwrapped porous polyethylene (Medpor) orbital implants in enucleated patients". Ophthal Plast Reconstr Surg. 2011;27(5):391; author reply 391-2. [24] 易敬林,王文娟,徐荣,等.三种义眼座血管化的SPECT和组织病理学实验研究[J].眼外伤职业眼病杂志,2004,26(12): 797-801.[25] 张虹,李贵刚,王军明,等.羟基磷灰石义眼台纤维血管化的实验研究[J].眼外伤职业眼病杂志,2004,26(3):150-153.[26] 樊建中,孔祥泉,史河水,等.兔眼眶植入羟基磷灰石义眼台血管化的MRI评价[J].中华放射学杂志,2007,41(11):1254-1257.[27] 刘静.bFGF胶原蛋白复合海绵促进多孔羟基磷灰石义眼台血管化的实验研究[D].江西:南昌大学,2007:1-45.[28] 徐俊辉,朱春玲.羟基磷灰石义眼台植入26例的临床观察[J].国际眼科杂志,2012,12(2):357-358.[29] 曾波,周雄,周和政,等.二期羟基磷灰石义眼台早期植入临床观察[J].国际眼科杂志,2012,12(12):2417-2418.[30] 刘先利,王守彪.完整巩膜壳后羟基磷灰石义眼台植入的临床观察[J].中国煤炭工业医学杂志,2012,15(11):1699-1700.[31] 马先祯,毕宏生,张晓.羟基磷灰石义眼台植入52例效果分析[J].国际眼科杂志,2012,12(5):988-990.[32] 穆敬中,凌晨,曹丽辉.活体巩膜腔内义眼台植入术式改良探讨[J]. 黑龙江医药科学,2012,35(2):112.[33] 王健,解正高,陈放,等.羟基磷灰石义眼台置入术的临床效果观察[J].中国美容医学,2012,21(07X):117-118.[34] 何旺旺,史凤珍.羟基磷灰石义眼台植入临床观察[J].中国社区医师(医学专业),2012,14(31):152-153.[35] 潘敏敏,焦演歌,杨晓峰.巩膜花瓣状成形、羟基磷灰石义眼台植入术的效果观察[J].山东医药,2012,52(26):66-67.[36] 樊蕾.羟基磷灰石义眼台植入术后临床观察[J].中国医学创新, 2012,9(12):126-127.[37] 杨洁文,楼尧勇.改良羟基磷灰石义眼台植入术78例临床分析[J].浙江实用医学,2012,17(2):128-129.[38] 蔡涛,李毅宏.羟基磷灰石义眼台的生物学特征[J].中国组织工程研究与临床康复,2008,12(44):8754-8757.[39] 夏伟.羟基磷灰石义眼台临床应用16例[J].眼科新进展,2005, 25(4):300.[40] 黄丹平,刘金陵,郑永欣,等.羟基磷灰石义眼台植入后义眼台暴露的处理[J].中国实用眼科杂志,2000,18(11):720-721.[41] 闵燕,李冬梅,赵颖,等.羟基磷灰石义眼台植入术后结膜切口裂开的修复和预防[J].中国实用眼科杂志,2001,19(5):394-395.[42] 王蔚,张孝生,卢弘.羟基磷灰石义眼台眶内植入术及相应并发症的相关分析[J].中国实用眼科杂志,2007,25(9):1019-1021..[43] Noah EM, Chen J, Jiao X, et al. Impact of sterilization on the porous design and cell behavior in collagen sponges prepared for tissue engineering. Biomaterials. 2002;23(14): 2855-2861.[44] Swatschek D, Schatton W, Kellermann J, et al. Marine sponge collagen: isolation, characterization and effects on the skin parameters surface-pH, moisture and sebum. Eur J Pharm Biopharm. 2002;53(1):107-113.[45] 陈晓东,袁即山,祁少海,等.胶原蛋白海绵在多种创面修复中的应用[J].中国临床康复,2004,8(32):7200-7201.[46] 徐杰,左金华.碱性成纤维细胞生长因子促进血管再生的研究进展[J].实用医学杂志,2008,24(24):4317-4318.[47] Böttcher RT, Niehrs C. Fibroblast growth factor signaling during early vertebrate development. Endocr Rev. 2005;26(1): 63-77.[48] Damico FM. Angiogenesis and retinal diseases. Arq Bras Oftalmol. 2007;70(3):547-553. |
| [1] | Shen Jinbo, Zhang Lin. Micro-injury of the Achilles tendon caused by acute exhaustive exercise in rats: ultrastructural changes and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1190-1195. |
| [2] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| [3] | Duan Liyun, Cao Xiaocang. Human placenta mesenchymal stem cells-derived extracellular vesicles regulate collagen deposition in intestinal mucosa of mice with colitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1026-1031. |
| [4] | Liu Jiangfeng. Nano-hydroxyapatite/polyamide 66 composite filling combined with locking plate in the treatment of fibrous dysplasia of femoral bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 542-547. |
| [5] | Li Li, Ma Li. Immobilization of lactase on magnetic chitosan microspheres and its effect on enzymatic properties [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 576-581. |
| [6] | Liu Liu, Zhou Qingzhu, Gong Zhuo, Liu Boyan, Yang Bin, Zhao Xian. Characteristics and manufacturing techniques of collagen/inorganic materials for constructing tissue-engineered bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 607-613. |
| [7] | Chen Lei, Zheng Rui, Jie Yongsheng, Qi Hui, Sun Lei, Shu Xiong. In vitro evaluation of adipose-derived stromal vascular fraction combined with osteochondral integrated scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3487-3492. |
| [8] | He Lin, Wu Xi, He Song, Yang Sen. Hydrophilicity and cell adhesion of hydroxyapatite bioceramics after the coating of polydopamine [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3540-3544. |
| [9] | Zhou Anqi, Tang Yufei, Wu Bingfeng, Xiang Lin. Designing of periosteum tissue engineering: combination of generality and individuality [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3551-3557. |
| [10] | Lang Limin, He Sheng, Jiang Zengyu, Hu Yiyi, Zhang Zhixing, Liang Minqian. Application progress of conductive composite materials in the field of tissue engineering treatment of myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3584-3590. |
| [11] | Wang Hao, Chen Mingxue, Li Junkang, Luo Xujiang, Peng Liqing, Li Huo, Huang Bo, Tian Guangzhao, Liu Shuyun, Sui Xiang, Huang Jingxiang, Guo Quanyi, Lu Xiaobo. Decellularized porcine skin matrix for tissue-engineered meniscus scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3473-3478. |
| [12] | Yang Li, Li Xueli, Song Jinghui, Yu Huiqian, Wang Weixia. Effect of cryptotanshinone on hypertrophic scar of rabbit ear and its related mechanism [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3150-3155. |
| [13] | Zhi Yibo, Zhang Jie, Liu Jian, Li Weiyan. Chemokine CCL21 in anterior cingulate cortex is involved in chronic neuropathic pain in a rat model [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(2): 242-246. |
| [14] | Liu Zhendong, Wang Rui, Li Xiaolei, Wang Jingcheng. Review of interferon alpha-2b inhibiting scar formation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(2): 317-321. |
| [15] | Du Xueting, Yang Yang, Huang Wenhua, Chen Wubiao. Clinical application and breakthrough of three-dimensional printing based on medical imaging technology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2887-2894. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||