Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (27): 4340-4345.doi: 10.12307/2024.555
Previous Articles Next Articles
Relationship between statin drugs and bone density: a drug target-mediated Mendelian randomization study
Ma Weiwei1, Xiong Yong1, Chen Honggu2, Huang Wenzhuo1, Huang Xin1, Zhou Xiaohong1
- 1Hubei University of Chinese Medicine, Wuhan 430061, Hubei Province, China; 2Affiliated Hospital of Jiangsu University, Zhenjiang 212000, Jiangsu Province, China
-
Received:2023-10-07Accepted:2023-11-10Online:2024-09-28Published:2024-01-27 -
Contact:Xiong Yong, MD, Associate professor, Associate chief physician, Master’s supervisor, Hubei University of Chinese Medicine, Wuhan 430061, Hubei Province, China Chen Honggu, Master, Affiliated Hospital of Jiangsu University, Zhenjiang 212000, Jiangsu Province, China -
About author:Ma Weiwei, Master candidate, Hubei University of Chinese Medicine, Wuhan 430061, Hubei Province, China -
Supported by:Young and Middle-aged Talent Project of Hubei Provincial Department of Education, No. Q20212004 (to ZXH); Scientific Research Program Guiding Project of Hubei Provincial Department of Education, No. B2022107 (to XY)
CLC Number:
Cite this article
Ma Weiwei, Xiong Yong, Chen Honggu, Huang Wenzhuo, Huang Xin, Zhou Xiaohong. Relationship between statin drugs and bone density: a drug target-mediated Mendelian randomization study[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4340-4345.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
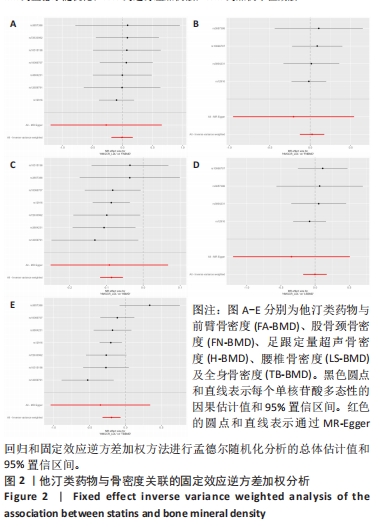
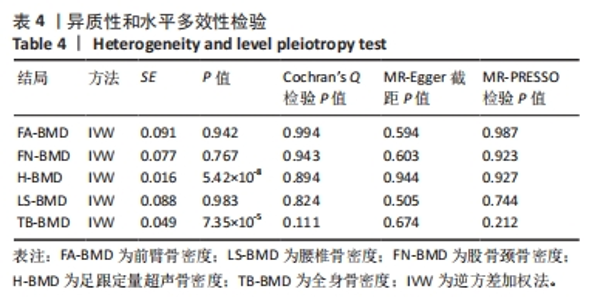
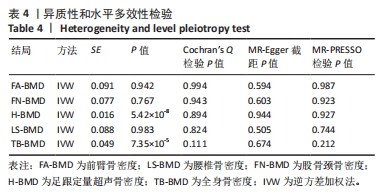
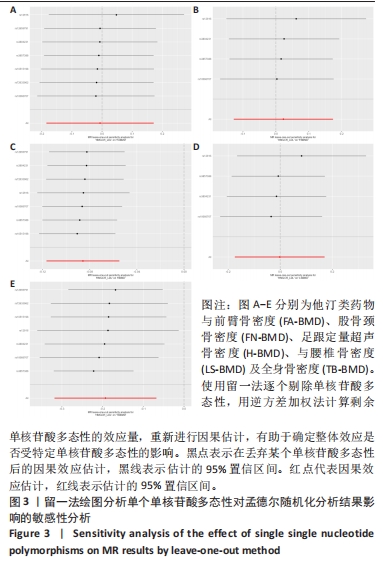
| [1] LI J, CHEN X, LU L, et al. The relationship between bone marrow adipose tissue and bone metabolism in postmenopausal osteoporosis. Cytokine Growth Factor Rev. 2020;52:88-98. [2] XU Q, LI D, CHEN J, et al. Crosstalk between the gut microbiota and postmenopausal osteoporosis: Mechanisms and applications. Int Immunopharmacol. 2022;110:108998. [3] MARTÍN-GONZÁLEZ C, GONZÁLEZ-REIMERS E, QUINTERO-PLATT G, et al. Lipid profile and bone mineral density in heavy alcoholics. Clin Nutr. 2018; 37(6 Pt A):2137-2143. [4] LI S, GUO H, LIU Y, et al. Relationships of serum lipid profiles and bone mineral density in postmenopausal Chinese women. Clin Endocrinol (Oxf). 2015;82(1): 53-58. [5] ALLA VM, AGRAWAL V, DENAZARETH A, et al. A reappraisal of the risks and benefits of treating to target with cholesterol lowering drugs. Drugs. 2013;73(10): 1025-1054. [6] UZZAN B, COHEN R, NICOLAS P, et al. Effects of statins on bone mineral density: a meta-analysis of clinical studies. Bone. 2007;40(6):1581-1587. [7] LIN TK, CHOU P, LIN CH, et al. Long-term effect of statins on the risk of new-onset osteoporosis: A nationwide population-based cohort study. PLoS One. 2018; 13(5):e0196713. [8] VAN DER BAAN FH, KLUNGEL OH, EGBERTS AC, et al. Pharmacogenetics in randomized controlled trials: considerations for trial design. Pharmacogenomics. 2011;12(10):1485-1492. [9] GRECO M FD, MINELLI C, SHEEHAN NA, et al. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat Med. 2015;34(21):2926-2940. [10] BOWDEN J, HOLMES MV. Meta-analysis and Mendelian randomization: A review. Res Synth Methods. 2019;10(4):486-496. [11] SEKULA P, DEL GRECO MF, PATTARO C, et al. Mendelian Randomization as an Approach to Assess Causality Using Observational Data. J Am Soc Nephrol. 2016;27(11):3253-3265. [12] LIU L, ZENG P, XUE F, et al. Multi-trait transcriptome-wide association studies with probabilistic Mendelian randomization. Am J Hum Genet. 2021;108(2):240-256. [13] FERENCE BA. Interpreting the Clinical Implications of Drug-Target Mendelian Randomization Studies. J Am Coll Cardiol. 2022;80(7):663-665. [14] WISHART DS, FEUNANG YD, GUO AC, et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res. 2018;46(D1): D1074-D1082. [15] SKRIVANKOVA VW, RICHMOND RC, WOOLF BAR, et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The STROBE-MR Statement. JAMA. 2021;326(16):1614-1621. [16] WILLER CJ, SCHMIDT EM, SENGUPTA S, et al. Discovery and refinement of loci associated with lipid levels. Nat Genet. 2013;45(11):1274-1283. [17] CAMACHO PM, PETAK SM, BINKLEY N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis-2020 Update. Endocr Pract. 2020;26(Suppl 1):1-46. [18] ZHENG HF, FORGETTA V, HSU YH, et al. Whole-genome sequencing identifies EN1 as a determinant of bone density and fracture. Nature. 2015;526(7571):112-117. [19] MORRIS JA, KEMP JP, YOULTEN SE, et al. An atlas of genetic influences on osteoporosis in humans and mice [published correction appears in Nat Genet. 2019;51(5):920]. Nat Genet. 2019;51(2):258-266. [20] MEDINA-GOMEZ C, KEMP JP, TRAJANOSKA K, et al. Life-Course Genome-wide Association Study Meta-analysis of Total Body BMD and Assessment of Age-Specific Effects. Am J Hum Genet. 2018;102(1):88-102. [21] ZHANG X, GENG T, LI N, et al. Associations of Lipids and Lipid-Lowering Drugs with Risk of Vascular Dementia: A Mendelian Randomization Study. Nutrients. 2022;15(1):69. [22] HUANG W, XIAO J, JI J, et al. Association of lipid-lowering drugs with COVID-19 outcomes from a Mendelian randomization study. Elife. 2021;10: e73873. [23] HEMANI G, TILLING K, DAVEY SMITH G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data [published correction appears in PLoS Genet. 2017;13(12 ):e1007149]. PLoS Genet. 2017; 13(11):e1007081. [24] YUAN S, XIONG Y, LARSSON SC. An atlas on risk factors for multiple sclerosis: a Mendelian randomization study. J Neurol. 2021;268(1):114-124. [25] MASSON W, CORRAL P, BARBAGELATA L, et al. Reduction of cardiovascular events with the use of lipid-lowering medication in patients with familial hypercholesterolemia or severe primary hypercholesterolemia: A systematic review. J Clin Lipidol. 2022;16(5):562-573. [26] BOWDEN J, DAVEY SMITH G, HAYCOCK PC, et al. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. 2016;40(4):304-314. [27] BURGESS S, THOMPSON SG. Interpreting findings from Mendelian randomization using the MR-Egger method [published correction appears in Eur J Epidemiol. 2017;32(5):391-392]. Eur J Epidemiol. 2017;32(5):377-389. [28] JIA N, DONG L, LU Q, et al. The causal effect of schizophrenia on fractures and bone mineral density: a comprehensive two-sample Mendelian randomization study of European ancestry. BMC Psychiatry. 2023;23(1):692. [29] LAWLOR DA, HARBORD RM, STERNE JA, et al. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27(8):1133-1163. [30] BOWDEN J, DAVEY SMITH G, BURGESS S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512-525. [31] WU X, ZHANG W, ZHAO X, et al. Investigating the relationship between depression and breast cancer: observational and genetic analyses. BMC Med. 2023;21(1):170. [32] BOWDEN J, DEL GRECO MF, MINELLI C, et al. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat Med. 2017;36(11):1783-1802. [33] VERBANCK M, CHEN CY, NEALE B, et al. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases [published correction appears in Nat Genet. 2018;50(8):1196]. Nat Genet. 2018;50(5):693-698. [34] MA W, ZHOU X, HUANG X, et al. Causal relationship between body mass index, type 2 diabetes and bone mineral density: Mendelian randomization. PLoS One. 2023;18(10):e0290530. [35] WANG JS, TOKAVANICH N, WEIN MN. SP7: from Bone Development to Skeletal Disease. Curr Osteoporos Rep. 2023;21(2):241-252. [36] XU J, CAO B, LI C, et al. The recent progress of endocrine therapy-induced osteoporosis in estrogen-positive breast cancer therapy. Front Oncol. 2023;13: 1218206. [37] LIU Q, TOOKI T, DI D, et al. Role of lifestyle factors in mediating the effect of educational attainment on bone mineral density: a Mendelian randomization study. Arch Osteoporos. 2023;18(1):120. [38] HE X, HU W, ZHANG Y, et al. Cellular senescence in skeletal disease: mechanisms and treatment. Cell Mol Biol Lett. 2023;28(1):88. [39] LI Y, SI Y, MA Y, et al. Application and prospect of metabolomics in the early diagnosis of osteoporosis: a narrative review. Bioanalysis. 2023;15(22): 1369-1379. [40] AN T, HAO J, SUN S, et al. Efficacy of statins for osteoporosis: a systematic review and meta-analysis. Osteoporos Int. 2017;28(1):47-57. [41] LIU J, ZHU LP, YANG XL, et al. HMG-CoA reductase inhibitors (statins) and bone mineral density: a meta-analysis. Bone. 2013;54(1):151-156. [42] WANG Z, LI Y, ZHOU F, et al. Effects of Statins on Bone Mineral Density and Fracture Risk: A PRISMA-compliant Systematic Review and Meta-Analysis. Medicine (Baltimore). 2016;95(22):e3042. [43] REJNMARK L, OLSEN ML, JOHNSEN SP, et al. Hip fracture risk in statin users--a population-based Danish case-control study. Osteoporos Int. 2004; 15(6):452-458. [44] XIONG M, XUE Y, ZHU W, et al. Comparative efficacy and safety of statins for osteoporosis: a study protocol for a systematic review and network meta-analysis. BMJ Open. 2022;12(5):e054158. [45] REID IR, HAGUE W, EMBERSON J, et al. Effect of pravastatin on frequency of fracture in the LIPID study: secondary analysis of a randomised controlled trial. Long-term Intervention with Pravastatin in Ischaemic Disease. Lancet. 2001;357(9255):509-512. [46] PEÑA JM, ASPBERG S, MACFADYEN J, et al. Statin therapy and risk of fracture: results from the JUPITER randomized clinical trial. JAMA Intern Med. 2015;175(2): 171-177. [47] PEDERSEN TR, WILHELMSEN L, FAERGEMAN O, et al. Follow-up study of patients randomized in the Scandinavian simvastatin survival study (4S) of cholesterol lowering. Am J Cardiol. 2000;86(3):257-262. [48] WARREN T, MCALLISTER R, MORGAN A, et al. The Interdependency and Co-Regulation of the Vitamin D and Cholesterol Metabolism. Cells. 2021; 10(8):2007. [49] PRABHU AV, LUU W, LI D, et al. DHCR7: A vital enzyme switch between cholesterol and vitamin D production. Prog Lipid Res. 2016;64:138-151. [50] GÓMEZ-CORONADO D, LASUNCIÓN MA, MARTÍNEZ-BOTAS J, et al. Role of cholesterol metabolism in the anticancer pharmacology of selective estrogen receptor modulators. Semin Cancer Biol. 2021;73:101-115. [51] YU D, LIAO JK. Emerging views of statin pleiotropy and cholesterol lowering. Cardiovasc Res. 2022;118(2):413-423. [52] ABDUL-RAHMAN T, BUKHARI SMA, HERRERA EC, et al. Lipid Lowering Therapy: An Era Beyond Statins. Curr Probl Cardiol. 2022;47(12):101342. [53] RAY KK. Changing the paradigm for post-MI cholesterol lowering from intensive statin monotherapy towards intensive lipid-lowering regimens and individualized care. Eur Heart J. 2021;42(3):253-256. [54] OXLUND H, DALSTRA M, ANDREASSEN TT. Statin given perorally to adult rats increases cancellous bone mass and compressive strength. Calcif Tissue Int. 2001;69(5):299-304. [55] TIAN L, YU X. Lipid metabolism disorders and bone dysfunction--interrelated and mutually regulated (review). Mol Med Rep. 2015;12(1):783-794. [56] NIU J, DING G, ZHANG L. Effects of simvastatin on the osteogenic differentiation and immunomodulation of bone marrow mesenchymal stem cells. Mol Med Rep. 2015;12(6):8237-8240. [57] XU R, SHI G, XU L, et al. Simvastatin improves oral implant osseointegration via enhanced autophagy and osteogenesis of BMSCs and inhibited osteoclast activity. J Tissue Eng Regen Med. 2018;12(5):1209-1219. [58] CHAMANI S, LIBERALE L, MOBASHERI L, et al. The role of statins in the differentiation and function of bone cells. Eur J Clin Invest. 2021;51(7): e13534. |
| [1] | Yang Cekai, Cai Zhuoyan, Chen Ming, Liu Hao, Weng Rui, Cui Jianchao, Zhang Shuncong, Yao Zhensong. Relationship between degeneration of paraspinal muscle and refractures in postmenopausal women treated by percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1414-1419. |
| [2] | Xiaheida·Yilaerjiang, Nijiati·Tuerxun, Reyila·Kuerban, Baibujiafu·Yelisi, Chen Xin. Three-dimensional finite element analysis of the distribution pattern of stress in bone tissues with different characteristics [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1277-1282. |
| [3] | Kaiyisaier•Abudukelimu, Maimaitimin•Abulimiti, Li Lei, Yang Xiaokai, Zhang Yukun, Liu Shuai. Effect of lumbar CT values in the diagnosis of osteoporosis in women patients with lumbar degenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 945-949. |
| [4] | Wang Liping, Lian Tianxing, Hu Yongrong, Yang Hongsheng, Zeng Zhimou, Liu Hao, Qu Bo. HU value of chest CT vertebral body in the opportunistic screening of type 2 diabetes mellitus osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 950-954. |
| [5] | Abuduwupuer·Haibier, Alimujiang·Yusufu, Maihemuti·Yakufu, Maimaitimin·Abulimiti, Tuerhongjiang·Abudurexiti. Meta-analysis of efficacy and safety of terlipatide and bisphosphate in the treatment of postmenopausal osteoporosis fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 639-645. |
| [6] | Chen Jixin, Yu Weijie, Guo Tianci, Zhou Qinxin, Niu Puyu, Ye Yuntian, Liu Aifeng. Sleep characteristics and risk of osteoarthritis: a two-sample and multivariate Mendelian randomization study [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5203-5209. |
| [7] | Chen Tianxin, Dong Tingting, Li Yan, Zhang Sheng, Zhang Lei. Causal relationship between blood metabolites and sarcopenia-related traits: a Mendelian randomization study [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4288-4292. |
| [8] | Fan Yidong, Qin Gang, He Kaiyi, Gong Yufang, Li Weicai, Wu Guangtao. Expression of immune-related genes in rheumatoid arthritis and a two-sample Mendelian randomization study of immune cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4312-4318. |
| [9] | Zhan Qunzhang, Zhang Yuling, Han Yuxin, Lyu Jiazhen, Zheng Xiaoxia, Qu Chongzheng. Association between obesity and osteoporosis: a two-sample Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4319-4324. |
| [10] | Chai Jinlian, Li Shudong, Li Wei, Du Haitao, Dong Limin, Liang Xuezhen, Wang Ping. Gut microbiota and drug-associated osteonecrosis: a two‑sample Mendelian randomization study [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4325-4331. |
| [11] | Wu Ruiqi, Zhang Xuan, Zhou Yi, Meng Lin, Li Hongyu. Two-sample Mendelian randomization analysis of the relationship between statins and the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(26): 4106-4112. |
| [12] | Peng Zhihua, Pan Junxi, Feng Qinghui, Tian Tianzhao, Zhang Sheng, Li An, Cai Yingfeng. The causal relationship between blood lipids and muscle atrophy based on Mendelian randomization analysis of two samples [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3699-3703. |
| [13] | Wu Ruiqi, Zhou Yi, Xia Tian, Zhang Chi, Yang Qipei, Zhang Xuan, Zhang Yazhong, Cui Wei. Mendelian randomization study on the association between rheumatoid arthritis and osteoporosis and bone mineral density [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3715-3721. |
| [14] | Zhang Wensheng, Song Zhenjie, Wu Chunfei, Li Wenchao, Liu Hongjiang, Yang Xiaoguang, Yuan Chao. Prediction of osteoporotic vertebral compression fracture based on comprehensive index of lumbar vertebral bone strength [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2871-2875. |
| [15] | Wu Tianliang, Tao Xiuxia, Xu Hongguang. Influence of different bone mineral densities on cage subsidence after stand-alone oblique lateral interbody fusion: three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1352-1358. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||