Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (27): 4319-4324.doi: 10.12307/2024.579
Previous Articles Next Articles
Association between obesity and osteoporosis: a two-sample Mendelian randomization analysis
Zhan Qunzhang1, Zhang Yuling1, Han Yuxin1, Lyu Jiazhen1, Zheng Xiaoxia1, Qu Chongzheng2
- 1Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China; 2Department of Acupuncture and Massage, Third Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510378, Guangdong Province, China
-
Received:2023-10-19Accepted:2023-12-18Online:2024-09-28Published:2024-01-27 -
Contact:Qu Chongzheng, MD, Chief physician, Department of Acupuncture and Massage, Third Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510378, Guangdong Province, China -
About author:Zhan Qunzhang, Master, Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
Supported by:the “Thirteenth Five-Year Plan” Key Specialized Construction Project of Traditional Chinese Medicine in Guangdong Province, China, No. [2019]472 (to QCZ); Guangdong Provincial Science and Technology Plan Project in 2017, No. 2017ZC0136 (to QCZ)
CLC Number:
Cite this article
Zhan Qunzhang, Zhang Yuling, Han Yuxin, Lyu Jiazhen, Zheng Xiaoxia, Qu Chongzheng. Association between obesity and osteoporosis: a two-sample Mendelian randomization analysis[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4319-4324.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

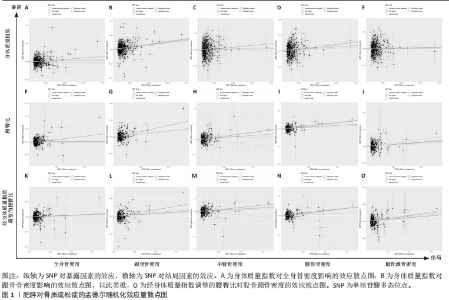
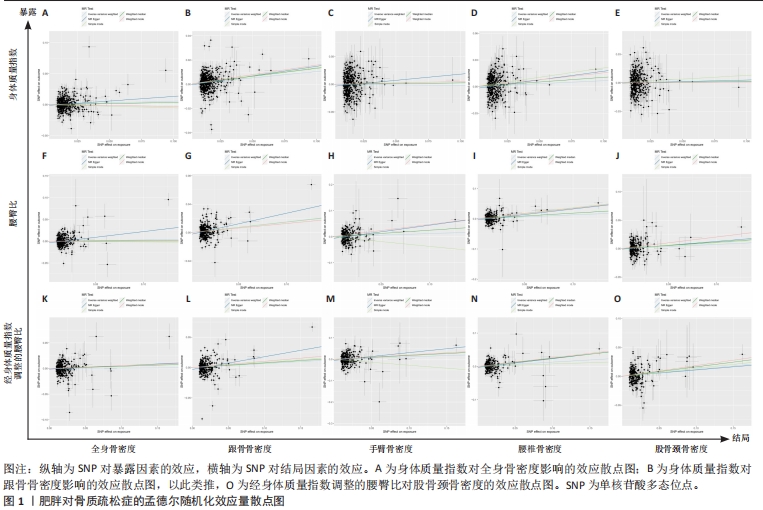
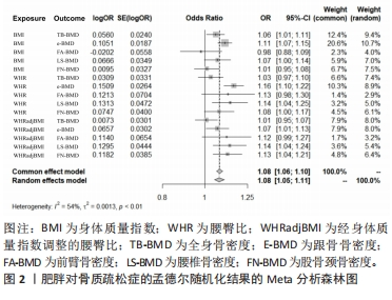
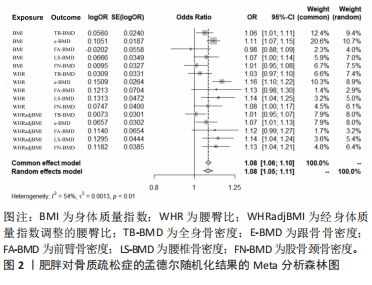
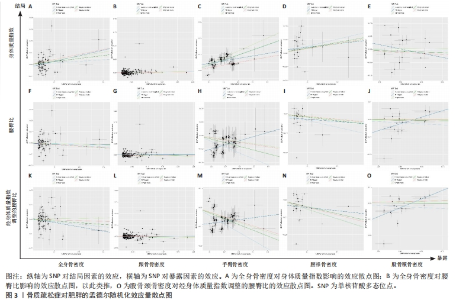
2.1 肥胖对骨质疏松症的影响 2.1.1 工具变量 在探索肥胖作为暴露因素对骨质疏松症患病率的因果影响时,在考虑遗传变异作为工具变量的独立性和连锁不平衡后,研究从身体质量指数、腰臀比及经身体质量指数调整的腰臀比的GWAS数据集中分别筛选出了531个SNPs、346个SNPs及322个SNPs,其P值均小于5×10-8,说明这些SNPs与暴露因素高度相关,满足关联性假设。通过Phenoscanner数据库搜索,无剔除SNPs,所有SNPs均符合独立性假设和排他性假设,计算F值均大于10。 2.1.2 孟德尔随机化分析结果 逆方差加权法法分析表明,跟骨骨密度作为结局数据集,与身体质量指数(OR=1.111,95%CI:1.071-1.152,P=0.000)、腰臀比(OR=1.163,95%CI:1.104-1.225,P=0.000)、经身体质量指数调整的腰臀比(OR=1.068,95%CI:1.007-1.133,P=0.029)之间呈现正向因果效应,且差异有显著性意义与身体质量指数(OR=1.111, 95%CI:1.071-1.152,P=0.000)、腰臀比(OR=1.163,95%CI:1.104-1.225, P < 0.001)、经身体质量指数调整的腰臀比(OR=1.068,95%CI:1.007-1.133,P=0.029)之间呈现正向因果效应,且差异有显著性意义,与身体质量指数之间无因果关系(P > 0.05)。股骨颈密度作为结局数据集,与身体质量指数、腰臀比之间无因果关系(P > 0.05),与经身体质量指数调整的腰臀比(OR=1.125,95%CI:1.044-1.214,P=0.002)呈现正向因果效应,差异有显著性意义。与身体质量指数之间无因果关系(P > 0.05)。股骨颈密度作为结局数据集,与身体质量指数、腰臀比之间无因果关系(P > 0.05),与经身体质量指数调整的腰臀比(OR=1.125,95%CI:1.044-1.214,P=0.002)呈现正向因果效应,差异有显著性意义。具体信息见表2。此外,孟德尔随机化-PRESSO方法在异常值校正前后的因果估计是一致的,散点图同样显示了遗传预测的回归线基本一致,见图1。以上结果表明孟德尔随机化分析的结果是可靠的。"
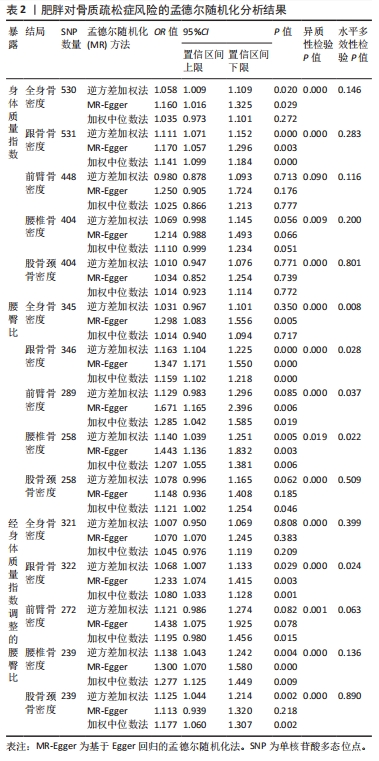
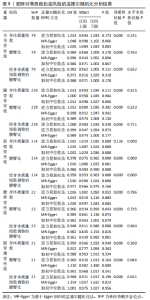
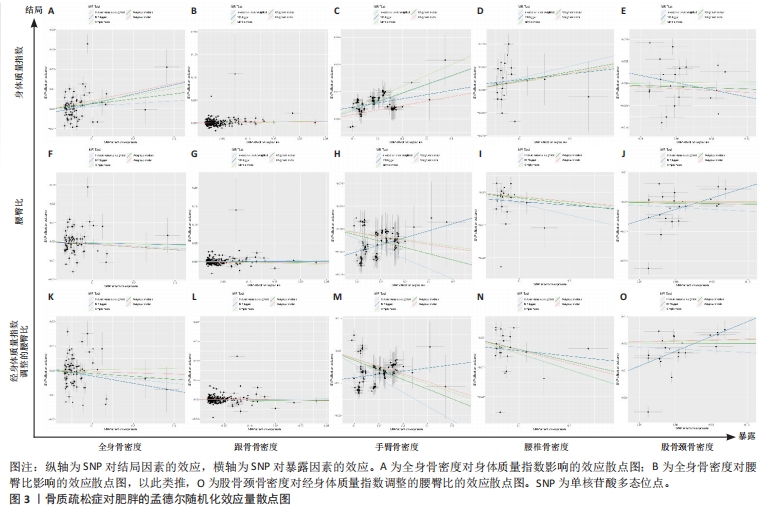
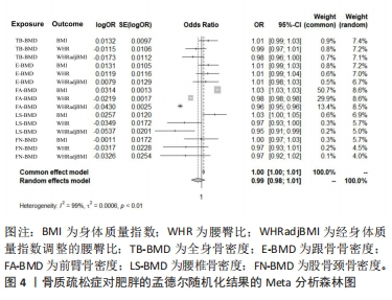
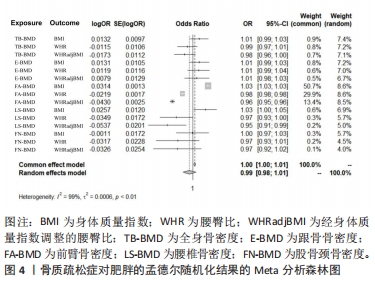
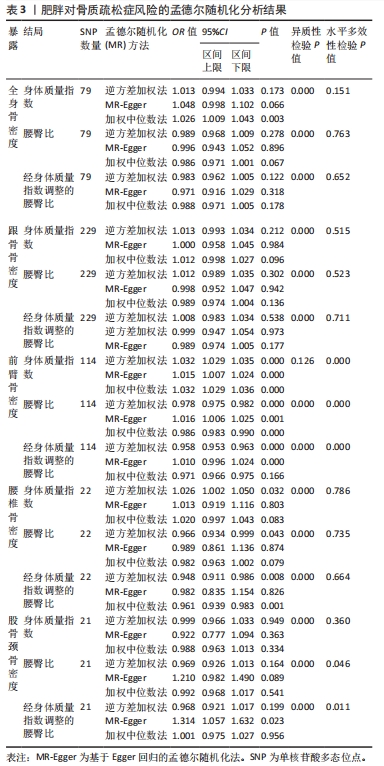
2.1.3 敏感性分析结果 Cochran’s Q检验结果表明,文章中存在显著的异质性(P < 0.05),见表2,采用随机效应模型进行分析。利用MR-Egger截距检验水平多效性,结果显示其截距的P值> 0.05,证明水平多效性并不显著,结果较稳健,见表2。留一法检验分析显示没有个别单核苷酸多态性对整体因果估计产生影响。为了进一步检验上述结果的稳定性,绘制的漏斗图中显示的因果效应分布基本对称,不受潜在因素影响而发生偏倚。 2.2 骨质疏松症对肥胖的影响 2.2.1 工具变量 在探索骨质疏松症作为暴露因素对肥胖的因果影响时,在考虑遗传变异作为工具变量的独立性和连锁不平衡后,文章从全身骨密度及跟骨骨密度的GWAS数据集中分别筛选出了79个SNPs及229个SNPs,其P值均小于5×10-8,说明这些SNPs与暴露因素高度相关,满足关联性假设。通过Phenoscanner数据库搜索,无剔除SNPs,所有SNPs均符合独立性假设和排他性假设,计算F值均大于10。 2.2.2 孟德尔随机化分析结果 逆方差加权法法分析表明,全身骨密度、跟骨骨密度、股骨颈骨密度与肥胖之间不呈现因果效应:全身骨密度与身体质量指数(OR=1.031,95%CI:0.994-1.033,P=0.173)、腰臀比(OR=0.989,95%CI:0.968-1.009,P=0.278)、经身体质量指数调整的腰臀比(OR=0.983,95%CI:0.962-1.005,P=0.122);跟骨骨密度与肥胖与身体质量指数(OR=1.013,95%CI:0.993-1.034,P=0.212)、腰臀比(OR=1.012,95%CI:0.989-1.035,P=0.302)、经身体质量指数调整的腰臀比(OR=1.008,95%CI:0.983-1.034,P=0.538);股骨颈骨密度与身体质量指数(OR=0.999,95%CI:0.966-1.033,P=0.949)、腰臀比(OR=0.969,95%CI:0.926-1.013,P=0.164)、经身体质量指数调整的腰臀比(OR=0.968,95%CI:0.921-1.017,P=0.199)。前臂骨密度、腰椎骨密度作为暴露因素对肥胖有因果关系,但因果效应方向性不一致,与身体质量指数呈正向因果关系,与腰臀比、经身体质量指数调整的腰臀比呈负向因果关系。具体结果见表3。此外,散点图同样显示了遗传预测的回归线方向的不一致进一步验证结果是可靠的,见图3。"
| [1] WU D, CLINE-SMITH A, SHASHKOVA E, et al. T-cell mediated inflammation in postmenopausal osteoporosis. Front Immunol. 2021;12:687551. [2] XIAO PL, CUI AY, HSU CJ, et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: a systematic review and meta-analysis. Osteoporos Int. 2022;33(10):2137-2153. [3] SIRIS ES, ADLER R, BILEZIKIAN J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25(5):1439-1443. [4] BOUDIN E, VAN HUL W. Mechanisms in endocrinology: genetics of human bone formation. Eur J Endocrinol. 2017;177(2):R69-R83. [5] MARSHALL D, JOHNELL O, WEDEL H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996; 312(7041):1254-1259. [6] EBELING PR, NGUYEN HH, ALEKSOVA J, et al. Secondary osteoporosis. Endocr Rev. 2022;43(2):240-313. [7] BLüHER M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288-298. [8] NIMPTSCH K, KONIGORSKI S, PISCHON T. Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism. 2019;92:61-70. [9] FELSON DT, ZHANG Y, HANNAN MT, et al. Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res. 1993;8(5):567-573. [10] JOHANSSON H, NAUREEN G, IQBAL R, et al. FRAX-based intervention thresholds for Pakistan. Osteoporos Int. 2022;33(1):105-112. [11] FINTINI D, CIANFARANI S, COFINI M, et al. The bones of children with obesity. Front Endocrinol (Lausanne). 2020;11:200. [12] EVANS AL, PAGGIOSI MA, EASTELL R, et al. Bone density, microstructure and strength in obese and normal weight men and women in younger and older adulthood. J Bone Miner Res. 2015;30(5):920-928. [13] PIñAR-GUTIERREZ A, GARCíA-FONTANA C, GARCíA-FONTANA B, et al. Obesity and bone health: a complex relationship. Int J Mol Sci. 2022;23(15):8303. [14] RINONAPOLI G, PACE V, RUGGIERO C, et al. Obesity and bone: a complex relationship. Int J Mol Sci. 2021;22(24):13662. [15] GKASTARIS K, GOULIS DG, POTOUPNIS M, et al. Obesity, osteoporosis and bone metabolism. J Musculoskelet Neuronal Interact. 2020;20(3):372-381. [16] BIRNEY E. Mendelian randomization. Cold Spring Harb Perspect Med. 2022;12(4): a041302. [17] WANG L, YU W, YIN X, et al. Prevalence of osteoporosis and fracture in china: the china osteoporosis prevalence study. JAMA Netw Open. 2021;4(8):e2121106. [18] NUTTALL FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50(3):117-128. [19] MUDIE K, LAWLOR DA, PEARCE N, et al. How does the association of general and central adiposity with glycaemia and blood pressure differ by gender and area of residence in a Malawian population: a cross-sectional study. Int J Epidemiol. 2018;47(3):887-898. [20] JAYEDI A, SOLTANI S, ZARGAR MS, et al. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ. 2020;370:m3324. [21] HASANI-RANJBAR S, JAFARI-ADLI S, PAYAB M, et al. Association of osteoporosis with anthropometric measures in a representative sample of iranian adults: the iranian multicenter osteoporosis study. Int J Prev Med. 2019;10:157. [22] JIA L, CHENG M. Correlation analysis between risk factors, BMD and serum osteocalcin, CatheK, PINP, β-crosslaps, TRAP, lipid metabolism and BMI in 128 patients with postmenopausal osteoporotic fractures. Eur Rev Med Pharmacol Sci. 2022;26(21):7955-7959. [23] SANTOS VRD, CHRISTOFARO DGD, GOMES IC, et al. Relationship between obesity, sarcopenia, sarcopenic obesity, and bone mineral density in elderly subjects aged 80 years and over. Rev Bras Ortop. 2018;53(3):300-305. [24] TIAN H, PAN J, QIAO D, et al. Adiposity reduces the risk of osteoporosis in Chinese rural population: the henan rural cohort study. BMC Public Health. 2020; 20(1):285. [25] GAO X, SHEN S, NIU Q, et al. Differential bone metabolism and protein expression in mice fed a high-fat diet versus Daurian ground squirrels following natural pre-hibernation fattening. J Zhejiang Univ Sci B. 2022;23(12):1042-1056. [26] KRISHNAMOORTHY D, FRECHETTE DM, ADLER BJ, et al. Marrow adipogenesis and bone loss that parallels estrogen deficiency is slowed by low-intensity mechanical signals. Osteoporos Int. 2016;27(2):747-756. [27] SUNDH D, RUDäNG R, ZOULAKIS M, et al. A high amount of local adipose tissue is associated with high cortical porosity and low bone material strength in older women. J Bone Miner Res. 2016;31(4):749-757. [28] DENG G, YIN L, LI K, et al. Relationships between anthropometric adiposity indexes and bone mineral density in a cross-sectional Chinese study. Spine J. 2021;21(2):332-342. [29] SONG W, SHENG Q, BAI Y, et al. Obesity, but not high-fat diet, is associated with bone loss that is reversed via CD4(+)CD25(+)Foxp3(+) Tregs-mediated gut microbiome of non-obese mice. NPJ Sci Food. 2023;7(1):14. [30] DA SILVA SV, RENOVATO-MARTINS M, RIBEIRO-PEREIRA C, et al. Obesity modifies bone marrow microenvironment and directs bone marrow mesenchymal cells to adipogenesis. Obesity (Silver Spring). 2016;24(12):2522-2532. [31] ROY B, CURTIS ME, FEARS LS, et al. Molecular mechanisms of obesity-induced osteoporosis and muscle atrophy. Front Physiol. 2016;7:439. [32] COHEN A, SHEN W, DEMPSTER DW, et al. Marrow adiposity assessed on transiliac crest biopsy samples correlates with noninvasive measurement of marrow adiposity by proton magnetic resonance spectroscopy ((1)H-MRS) at the spine but not the femur. Osteoporos Int. 2015;26(10):2471-2478. [33] CORDES C, BAUM T, DIECKMEYER M, et al. MR-based assessment of bone marrow fat in osteoporosis, diabetes, and obesity. Front Endocrinol (Lausanne). 2016;7:74. |
| [1] | Guo Sutong, Feng Dehong, Guo Yu, Wang Ling, Ding Yujian, Liu Yi, Qian Zhengying, Li Mingyang. Construction and finite element analysis of normal and osteoporotic hip models [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1342-1346. |
| [2] | Yang Cekai, Cai Zhuoyan, Chen Ming, Liu Hao, Weng Rui, Cui Jianchao, Zhang Shuncong, Yao Zhensong. Relationship between degeneration of paraspinal muscle and refractures in postmenopausal women treated by percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1414-1419. |
| [3] | Zhong Jun, Wang Wen. Network meta-analysis of different anatomical repair strategies to improve chronic lateral ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1470-1476. |
| [4] | Zhang Xiaoyun, Liu Hua, Chai Yuan, Chen Feng, Zeng Hao, Gao Zhengang, Huang Yourong. Effect of Yishen Gushu Formula on bone metabolic markers and clinical efficacyn in patients with osteoporosis of kidney deficiency and blood stasis type [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1155-1160. |
| [5] | Dai Yuexing, Zheng Liqin, Wu Minhui, Li Zhihong, Li Shaobin, Zheng Desheng, Lin Ziling. Effect of vessel number on computational fluid dynamics in vascular networks [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1206-1210. |
| [6] | Xiaheida·Yilaerjiang, Nijiati·Tuerxun, Reyila·Kuerban, Baibujiafu·Yelisi, Chen Xin. Three-dimensional finite element analysis of the distribution pattern of stress in bone tissues with different characteristics [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1277-1282. |
| [7] | Wang Weiqing, Zhou Yue. Chronic inflammation regulates adipose tissue fibrosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1307-1312. |
| [8] | Ma Shuwei, He Sheng, Han Bing, Zhang Liaoyun. Exosomes derived from mesenchymal stem cells in treatment of animals with acute liver failure: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1137-1142. |
| [9] | Zhang Min, Peng Jing, Zhang Qiang, Chen Dewang. Mechanical properties of L3/4 laminar decompression and intervertebral fusion in elderly osteoporosis patients analyzed by finite element method [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 847-851. |
| [10] | Xue Xiaofeng, Wei Yongkang, Qiao Xiaohong, Du Yuyong, Niu Jianjun, Ren Lixin, Yang Huifeng, Zhang Zhimin, Guo Yuan, Chen Weiyi. Finite element analysis of osteoporosis in proximal femur after cannulated screw fixation for femoral neck fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 862-867. |
| [11] | Kaiyisaier•Abudukelimu, Maimaitimin•Abulimiti, Li Lei, Yang Xiaokai, Zhang Yukun, Liu Shuai. Effect of lumbar CT values in the diagnosis of osteoporosis in women patients with lumbar degenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 945-949. |
| [12] | Wang Liping, Lian Tianxing, Hu Yongrong, Yang Hongsheng, Zeng Zhimou, Liu Hao, Qu Bo. HU value of chest CT vertebral body in the opportunistic screening of type 2 diabetes mellitus osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 950-954. |
| [13] | Zhang Zeyi, Yang Yimin, Li Wenyan, Zhang Meizhen. Effect of foot progression angle on lower extremity kinetics of knee osteoarthritis patients of different ages: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 968-975. |
| [14] | Hu Zhixing, Li Qun, Yang Chao, Wang Xiaoxiao, Fang Luochangting, Hou Wuqiong, Lin Na, Chen Weiheng, Liu Chunfang, Lin Ya. Network meta-analysis of the modeling effects of different factors on rabbit models of steroid-induced osteonecrosis of femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 976-984. |
| [15] | Yu Zhaoyu, Tan Lixin, Sun Kai, Lu Yao, Li Yong. Meta-analysis of cement-augmented pedicle screw for thoracolumbar degenerative diseases with osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 813-820. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||