Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (27): 4378-4382.doi: 10.12307/2024.508
Previous Articles Next Articles
Autophagy protects neurons against facial nerve injury in rats
Duan Kunling, Fei Jing, Li Leiji
- Department of Otorhinolaryngology, Head and Neck Surgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Received:2023-08-28Accepted:2023-10-14Online:2024-09-28Published:2024-01-29 -
Contact:Li Leiji, Master, Chief physician, Department of Otorhinolaryngology, Head and Neck Surgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Duan Kunling, Master candidate, Department of Otorhinolaryngology, Head and Neck Surgery, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China -
Supported by:Luzhou Municipal Science and Technology Program, No. 2021-SYF-30 (to LLJ)
CLC Number:
Cite this article
Duan Kunling, Fei Jing, Li Leiji. Autophagy protects neurons against facial nerve injury in rats[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4378-4382.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
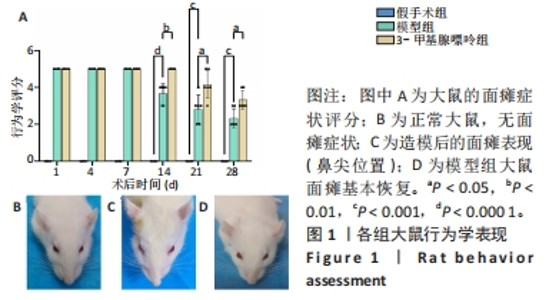
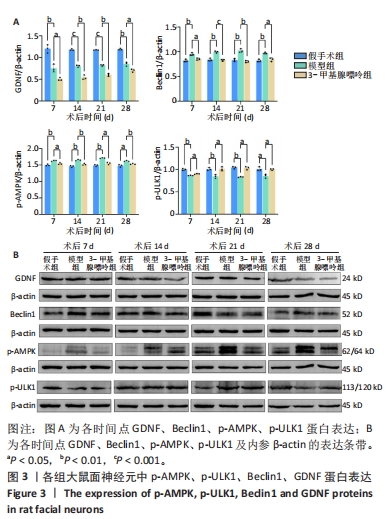
2.1 实验动物数量分析 共纳入72只SD大鼠,随机分为3组,全部进入结果分析,无脱落。 2.2 各组大鼠行为学比较 假手术组大鼠无周围性面瘫表现,评分为0分。术后1 d,模型组及3-甲基腺嘌呤组大鼠均表现为鼻尖明显偏向左侧、右侧眼睑无法闭合、胡须倒伏无活动,评分为5分,与假手术组比较,差异有显著性意义(P < 0.05),提示造模成功。术后4,7 d,模型组与3-甲基腺嘌呤组大鼠评分均为5分,上述面瘫症状无明显缓解,与假手术组比较,差异有显著性意义(P < 0.05)。术后14 d,模型组部分大鼠面瘫症状开始有一定的恢复,部分鼻尖稍向左侧倾斜、眨眼反射延迟、胡须运动较前明显,评分为3-5分;而3-甲基腺嘌呤组面瘫症状仍无明显缓解,评分仍为5分,与模型组比较,差异有显著性意义(P < 0.05)。术后28 d,模型组大鼠面瘫症状基本恢复,评分低于3分;3-甲基腺嘌呤组大鼠表现为鼻尖偏向左侧、右侧眼睑闭合稍差、胡须无自主活动,面瘫症状有一定程度恢复,但评分仍高于3分,与模型组比较,差异有显著性意义(P < 0.05),见图1。"
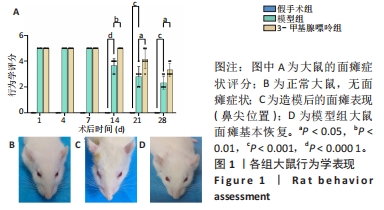

2.3 各组大鼠面神经元尼氏体变化 尼氏体是神经元的一种特征性结构。正常面神经元在低倍镜下大多呈角形细胞聚集,高倍镜下可见胞质淡红色,胞核呈淡蓝色或蓝色居中。尼氏染色显示:假手术组面神经元胞质染色均匀,尼氏体呈紫色“虎斑”样,胞核居中。术后7 d,模型组和3-甲基腺嘌呤组均出现神经元胞体皱缩,胞内染色不均,尼氏体减少,呈块状或颗粒状甚至粉末状,3-甲基腺嘌呤组更为严重。术后14 d,模型组尼氏体再现,呈颗粒状或块状,3-甲基腺嘌呤组大部分细胞内尼氏体缺失。术后28 d,模型组胞体大小及尼氏体形态基本恢复至术前,3-甲基腺嘌呤组逐渐恢复,可见部分细胞出现细颗粒状尼氏体。在术后各时间点,3组大鼠面神经核团平均吸光度值差异有显著性意义(P < 0.05),见图2。"
| [1] TOULGOAT F, SARRAZIN JL, BENOUDIBA F, et al. Facial nerve: from anatomy to pathology. Diagn Interv Imaging. 2013;94(10):1033-1042. [2] SPENCER CR, IRVING RM. Causes and management of facial nerve palsy. Br J Hosp Med (Lond). 2016;77(12):686-691. [3] FEI J, GAO L, LI HH, et al. Electroacupuncture promotes peripheral nerve regeneration after facial nerve crush injury and upregulates the expression of glial cell-derived neurotrophic factor. Neural Regen Res. 2019;14(4):673-682. [4] RIVERA A, RAYMOND M, GROBMAN A, et al. The effect of n-acetyl-cysteine on recovery of the facial nerve after crush injury. Laryngoscope Investig Otolaryngol. 2017;2(3):109-112. [5] 杨万章,吴芳,张敏.周围性面神经麻痹的中西医结合评定及疗效标准(草案)[J].中西医结合心脑血管病杂志,2005,3(9):786-787. [6] 唐杰,戚孟春,胡静.胶质细胞源性神经营养因子在自体静脉桥修复面神经缺损中促进神经再生的效应[J].华西口腔医学杂志,2011,29(1):87-91. [7] TAJDARAN K, GORDON T, WOOD MD, et al. A glial cell line-derived neurotrophic factor delivery system enhances nerve regeneration across acellular nerve allografts. Acta Biomater. 2016;29:62-70. [8] HENDERSON CE, PHILLIPS HS, POLLOCK RA, et al. GDNF: a potent survival factor for motoneurons present in peripheral nerve and muscle. Science. 1994;266(5187):1062-1064. [9] TRUPP M, RYDÉN M, JÖRNVALL H, et al. Peripheral expression and biological activities of GDNF, a new neurotrophic factor for avian and mammalian peripheral neurons. J Cell Biol. 1995;130(1):137-148. [10] LI L, WU W, LIN LF, et al. Rescue of adult mouse motoneurons from injury-induced cell death by glial cell line-derived neurotrophic factor. Proc Natl Acad Sci U S A. 1995;92(21):9771-9775. [11] EGGERS R, DE WINTER F, SMIT L, et al. Combining timed GDNF and ChABC gene therapy to promote long-distance regeneration following ventral root avulsion and repair. FASEB J. 2020;34(8):10605-10622. [12] IBÁÑEZ CF, ANDRESSOO JO. Biology of GDNF and its receptors - Relevance for disorders of the central nervous system. Neurobiol Dis. 2017;97(Pt B):80-89. [13] SHI Z, LI CY, ZHAO S, et al. A systems biology analysis of autophagy in cancer therapy. Cancer Lett. 2013;337(2):149-160. [14] CHANG JT, HANSEN M. Age-associated and tissue-specific decline in autophagic activity in the nematode C. elegans. Autophagy. 2018;14(7):1276-1277. [15] BHUKEL A, BEUSCHEL CB, MAGLIONE M, et al. Autophagy within the mushroom body protects from synapse aging in a non-cell autonomous manner. Nat Commun. 2019;10(1):1318. [16] DAMME M, SUNTIO T, SAFTIG P, et al. Autophagy in neuronal cells: general principles and physiological and pathological functions. Acta Neuropathol. 2015;129(3):337-362. [17] DIKIC I, ELAZAR Z. Mechanism and medical implications of mammalian autophagy. Nat Rev Mol Cell Biol. 2018;19(6):349-364. [18] THORBURN A. Apoptosis and autophagy: regulatory connections between two supposedly different processes. Apoptosis. 2008;13(1):1-9. [19] BUTLER DE, MARLEIN C, WALKER HF, et al. Inhibition of the PI3K/AKT/mTOR pathway activates autophagy and compensatory Ras/Raf/MEK/ERK signalling in prostate cancer. Oncotarget. 2017;8(34):56698-56713. [20] PELICCI G, TROGLIO F, BODINI A, et al. The neuron-specific Rai (ShcC) adaptor protein inhibits apoptosis by coupling Ret to the phosphatidylinositol 3-kinase/Akt signaling pathway. Mol Cell Biol. 2002;22(20):7351-7363. [21] ZHANG Y, MIAO JM. Ginkgolide K promotes astrocyte proliferation and migration after oxygen-glucose deprivation via inducing protective autophagy through the AMPK/mTOR/ULK1 signaling pathway. Eur J Pharmacol. 2018;832:96-103. [22] 郑红弟.面神经压榨损伤后面神经功能及形态学恢复的研究[D].泸州:西南医科大学,2022. [23] CHEN L, MO S, HUA Y. Compressive force-induced autophagy in periodontal ligament cells downregulates osteoclastogenesis during tooth movement. J Periodontol. 2019;90(10):1170-1181. [24] 杨敏,唐寅达,应婷婷,等.SD大鼠面神经干局部脱髓鞘模型制作[J].中国微侵袭神经外科杂志,2016,21(3):131-134. [25] DE FARIA SD, TESTA JR, BORIN A, et al. Standardization of techniques used in facial nerve section and facial movement evaluation in rats. Braz J Otorhinolaryngol. 2006;72(3):341-347. [26] LOPES B, SOUSA P, ALVITES R, et al. Peripheral Nerve Injury Treatments and Advances: One Health Perspective. Int J Mol Sci. 2022;23(2):918. [27] HÖKE A. Mechanisms of Disease: what factors limit the success of peripheral nerve regeneration in humans? Nat Clin Pract Neurol. 2006;2(8):448-454. [28] GORDON T, TYREMAN N, RAJI MA. The basis for diminished functional recovery after delayed peripheral nerve repair. J Neurosci. 2011;31(14):5325-5334. [29] HEINE W, CONANT K, GRIFFIN JW, et al. Transplanted neural stem cells promote axonal regeneration through chronically denervated peripheral nerves. Exp Neurol. 2004;189(2):231-240. [30] SULAIMAN OA, GORDON T. Effects of short- and long-term Schwann cell denervation on peripheral nerve regeneration, myelination, and size. Glia. 2000;32(3):234-246. [31] SHI R, WENG J, ZHAO L, et al. Excessive autophagy contributes to neuron death in cerebral ischemia. CNS Neurosci Ther. 2012;18(3):250-260. [32] ZHANG Y, ZHANG LH, CHEN X , et al. Piceatannol attenuates behavioral disorder and neurological deficits in aging mice via activating the Nrf2 pathway. Food Funct. 2018;9(1):371-378. [33] 费静,陶美惠,李雷激.电针干预面神经压榨模型大鼠促进面神经的再生[J].中国组织工程研究,2022,26(11):1728-1733. [34] 肖阳,龚立琼,费静,等.电针干预面神经损伤模型兔面神经核团中神经生长因子及其受体的表达[J].中国组织工程研究,2022,26(8):1253-1259. [35] 费静,郑红弟,余莉亚,等.胶质细胞源性神经营养因子/PI3K/AKT通路参与电针促进面神经压榨损伤模型兔的面神经再生[J].中国组织工程研究,2020,24(7):1094-1100. [36] MIZUSHIMA N, LEVINE B, CUERVO AM, et al. Autophagy fights disease through cellular self-digestion. Nature. 2008;451(7182):1069-1075. [37] JANG SY, SHIN YK, PARK SY, et al. Autophagy is involved in the reduction of myelinating Schwann cell cytoplasm during myelin maturation of the peripheral nerve. PLoS One. 2015; 10(1):e0116624. [38] SEGLEN PO, GORDON PB. 3-Methyladenine: specific inhibitor of autophagic/lysosomal protein degradation in isolated rat hepatocytes. Proc Natl Acad Sci U S A. 1982;79(6):1889-1892. [39] MARINELLI S, NAZIO F, TINARI A, et al. Schwann cell autophagy counteracts the onset and chronification of neuropathic pain. Pain. 2014;155(1):93-107. [40] CHEN H, HU Y, XIE K, et al. Effect of autophagy on allodynia, hyperalgesia and astrocyte activation in a rat model of neuropathic pain. Int J Mol Med. 2018;42(4):2009-2019. [41] ZHAO Y, FENG X, LI B, et al. Dexmedetomidine Protects Against Lipopolysaccharide-Induced Acute Kidney Injury by Enhancing Autophagy Through Inhibition of the PI3K/AKT/mTOR Pathway. Front Pharmacol. 2020;11:128. [42] ZHANG YL, YAO YT, FANG NX, et al. Restoration of autophagic flux in myocardial tissues is required for cardioprotection of sevoflurane postconditioning in rats. Acta Pharmacol Sin. 2014;35(6):758-769. [43] LIN LF, DOHERTY DH, LILE JD, et al. GDNF: a glial cell line-derived neurotrophic factor for midbrain dopaminergic neurons. Science. 1993;260(5111):1130-1132. [44] OMURA T, SANO M, OMURA K, et al. Different expressions of BDNF, NT3, and NT4 in muscle and nerve after various types of peripheral nerve injuries. J Peripher Nerv Syst. 2005;10(3):293-300. [45] CHEN P, PIAO X, BONALDO P. Role of macrophages in Wallerian degeneration and axonal regeneration after peripheral nerve injury. Acta Neuropathol. 2015;130(5):605-618. [46] MASAKI T, MATSUMURA K, SAITO F, et al. Expression of dystroglycan and laminin-2 in peripheral nerve under axonal degeneration and regeneration. Acta Neuropathol. 2000;99(3):289-295. [47] IWASE T, JUNG CG, BAE H, et al. Glial cell line-derived neurotrophic factor-induced signaling in Schwann cells. J Neurochem. 2005;94(6):1488-1499. [48] CAO Q, DU H, FU X, et al. Artemisinin Attenuated Atherosclerosis in High-Fat Diet-Fed ApoE-/- Mice by Promoting Macrophage Autophagy Through the AMPK/mTOR/ULK1 Pathway. J Cardiovasc Pharmacol. 2020;75(4):321-332. [49] CAI ZY, YANG B, SHI YX, et al. High glucose downregulates the effects of autophagy on osteoclastogenesis via the AMPK/mTOR/ULK1 pathway. Biochem Biophys Res Commun. 2018;503(2):428-435. [50] SHANG L, WANG X. AMPK and mTOR coordinate the regulation of Ulk1 and mammalian autophagy initiation. Autophagy. 2011;7(8):924-926. [51] KIM J, KUNDU M, VIOLLET B, et al. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat Cell Biol. 2011;13(2):132-141. [52] HA J, GUAN KL, KIM J. AMPK and autophagy in glucose/glycogen metabolism. Mol Aspects Med. 2015;46:46-62. [53] HWANG JY, GERTNER M, PONTARELLI F, et al. Global ischemia induces lysosomal-mediated degradation of mTOR and activation of autophagy in hippocampal neurons destined to die. Cell Death Differ. 2017;24(2):317-329. |
| [1] | Sheng Siqi, Xie Lin, Zhao Xiangyu, Jiang Yideng, Wu Kai, Xiong Jiantuan, Yang Anning, Hao Yinju, Jiao Yun. Involvement of miR-144-3p in Cbs+/- mouse hepatocyte autophagy induced by high-methionine diet [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1289-1294. |
| [2] | Wang Ji, Zhang Min, Li Wenbo, Yang Zhongya, Zhang Long. Effect of aerobic exercise on glycolipid metabolism, skeletal muscle inflammation and autophagy in type 2 diabetic rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1200-1205. |
| [3] | Zhou Bangyu, Li Jie, Ruan Yushang, Geng Funeng, Li Shaobo. Effects of Periplaneta americana powder on motor function and autophagic protein Beclin-1 in rats undergoing spinal cord hemisection [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1223-1228. |
| [4] | Pan Xiaolong, Fan Feiyan, Ying Chunmiao, Liu Feixiang, Zhang Yunke. Effect and mechanism of traditional Chinese medicine on inhibiting the aging of mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1091-1098. |
| [5] | Huang Yuxin, Liang Wenzi, Chen Xiuwen, Ni Na, Zhao Yinglin, Lin Changmin. Role of autophagy in hair regeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1112-1117. |
| [6] | Liu Qiwei, Zhang Junhui, Yang Yuan, Wang Jinjuan. Role and mechanism of umbilical cord mesenchymal stem cells on polycystic ovary syndrome [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1015-1020. |
| [7] | Xue Jingwen, Wang Fangfang, Zhang Xin, Pang Ruifeng, Wang Xiaoye, Ma Xiaoru. Effect of ganoderma spore on mitochondrial autophagy and apoptosis in testicular tissue of diabetic rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 562-568. |
| [8] | Yan Binghan, Li Zhichao, Su Hui, Xue Haipeng, Xu Zhanwang, Tan Guoqing. Mechanisms of traditional Chinese medicine monomers in the treatment of osteoarthritis by targeting autophagy [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 627-632. |
| [9] | Chen Guanting, Zhang Linqi, Wang Xixi, Chen Xu. Autophagy, ferroptosis-related targets and renal function progression in patients with chronic kidney disease: bioinformatics analysis and experimental verification [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5122-5129. |
| [10] | Xu Rui, Li Yanyan, Xu Hong. Effect and mechanism of short-chain fatty acids in aged rats with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5172-5176. |
| [11] | Zhai Sheng, Aikeremujiang • Aerken, Zhang Zheng, Rixiati • Paerhati, Hao Feihu. CircCDR1as/miR-7-5p/RAF1 axis promotes autophagy levels in steroid-induced necrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4455-4460. |
| [12] | Tian Yong, Zhou Ying, Gu Yongxiang, Yang Guohui. Metformin pretreatment induces cardiac autophagy to reduce myocardial injury in septic mice [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4469-4476. |
| [13] | Ma Yunfeng, Han Xiaofei. Eriodictyol accelerates glucocorticoid-induced apoptosis by promoting osteoblast autophagy [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4498-4504. |
| [14] | Guo Hui, Kong Jianda, Tian Chunlan. The role of mitochondrial autophagy-related receptor proteins and signaling pathways in the prevention and treatment of sarcopenia through exercise [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4397-4404. |
| [15] | Kong Jianda, Xie Yingao, Ma Wen, Liu Youhan, Wang Qinglu. Mitochondrial dysfunction in Parkinson’s disease and the potential ameliorative effects of exercise [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4413-4420. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||