Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (36): 5831-5836.doi: 10.12307/2022.790
Previous Articles Next Articles
Absence of a tourniquet during total knee arthroplasty: a prospective randomized controlled trial
Ma Qiaoqiao, Wu Zerui, Guo Zhuotao, Zhang Kai, Zha Guochun, Guo Kaijin
- Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
-
Received:2021-11-21Accepted:2021-12-31Online:2022-12-28Published:2022-04-27 -
Contact:Zha Guochun, MD, Associate chief physician, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
About author:Ma Qiaoqiao, Master candidate, Physician, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
Supported by:Young Medical Talent Project of Jiangsu Province, No. QNRC2016800 (to ZGC); General Project of Jiangsu Provincial Health and Family Planning Commission, No. H2017081 (to ZGC)
CLC Number:
Cite this article
Ma Qiaoqiao, Wu Zerui, Guo Zhuotao, Zhang Kai, Zha Guochun, Guo Kaijin. Absence of a tourniquet during total knee arthroplasty: a prospective randomized controlled trial[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5831-5836.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
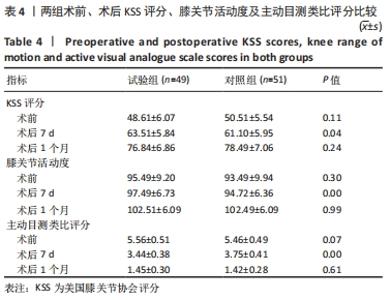
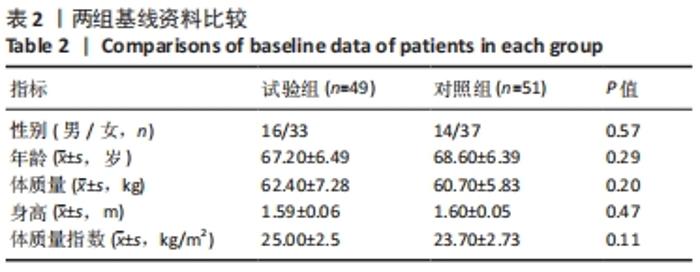
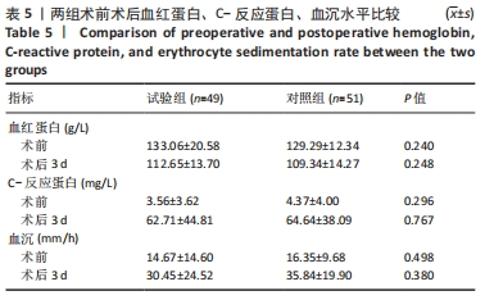
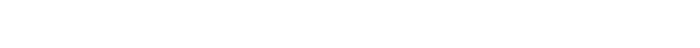
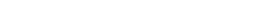
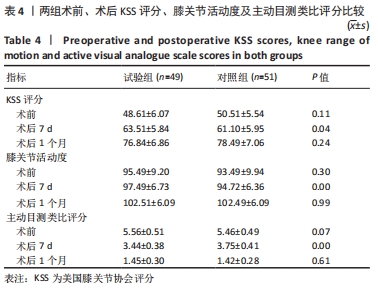
2.4 KSS评分、目测类比评分及膝关节活动度比较 随访1个月中,两组术前目测类比评分无差异,两组术后目测类比评分均有所改善,术后1周试验组目测类比评分明显优于对照组(P < 0.05),术后1个月两组差异无显著性意义(P > 0.05)。下肢肿胀率在术后1周内均逐渐变小,试验组明显优于对照组(P < 0.05),术后1个月随访,两组差异无显著性意义。由下肢肿胀率的变化可以得出结论,不使用止血带可以降低术后近期的肿胀率,对远期下肢肿胀率无明显差异。两组在术后不同阶段,膝关节KSS评分均有改善;术后1周内,试验组KSS评分优于对照组(P < 0.05);术后1个月时,两组KSS评分无明显差异,见表4。"
| [1] ROYECA JM, CUNNINGHAM CM, PANDIT H, et al. Complex regional pain syndrome as a result of total knee arthroplasty: A case report and review of literature. Case Rep Womens Health. 2019;23:e00136. [2] LU C, SONG M, CHEN J, et al. Does tourniquet use affect the periprosthetic bone cement penetration in total knee arthroplasty? A meta-analysis. J Orthop Surg Res. 2020;15(1):602. [3] CAWLEY DT, KELLY N, MCGARRY JP, et al. Cementing techniques for the tibial component in primary total knee replacement. Bone Joint J. 2013;95-b(3):295-300. [4] HOFMANN AA, GOLDBERG TD, TANNER AM, et al. Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty. 2006;21(3):353-357. [5] ARTHUR JR, SPANGEHL MJ. Tourniquet Use in Total Knee Arthroplasty. J Knee Surg. 2019;32(8):719-729. [6] AHMED I, CHAWLA A, UNDERWOOD M, et al. Time to reconsider the routine use of tourniquets in total knee arthroplasty surgery. Bone Joint J. 2021;103-B(5):830-839. [7] MAISTRELLI GL, ANTONELLI L, FORNASIER V, et al. Cement penetration with pulsed lavage versus syringe irrigation in total knee arthroplasty. Clin Orthop Relat Res. 1995;312:261-265. [8] ARGENSON JN, PARRATTE S, ASHOUR A, et al. The outcome of rotating-platform total knee arthroplasty with cement at a minimum often years of follow-up. J Bone Joint Surg Am. 2012;94:638-644. [9] FENG B, WENG X, LIN J, et al. Long-term follow-up of cemented fixed-bearing total knee arthroplasty in a Chinese population: a survival analysis of more than 10 years. J Arthroplasty. 2013;28:1701-1706. [10] PETERS CL, CRAIG MA, MOHR RA, et al. Tibial component fixation with cement: full- versus surface-cementation techniques. Clin Orthop Relat Res. 2003;409:158-168. [11] EWALD FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9-12. [12] GOMES LS, BECHTOLD JE, GUSTILO RB. Patellar prosthesis positioning in total knee arthroplasty. A roentgenographic study. Clin Orthop Relat Res. 1988;(236):72-81. [13] DENNIS DA, KITTELSON AJ, YANG CC, et al. Does Tourniquet Use in TKA Affect Recovery of Lower Extremity Strength and Function? A Randomized Trial. Clin Orthop Relat Res. 2016;474(1):69-77. [14] PARVIZI J, DIAZ-LEDEZMA C. Total knee replacement with the use ofa tourniquet: more pros than cons. Bone Joint J. 2013;95:133-134. [15] CHEN S, LI J, PENG H, et al. The influence of a half-course tourniquet strategy on peri-operative blood loss and early functional recovery in primary total knee arthroplasty. Int Orthop. 2014;38:355-359. [16] FENG L, ZHANG XG, YANG QG, et al. Effects of tourniquet on cardiac function in total knee arthroplasty with trans-esophageal echocardiography. Zhonghua Yi Xue Za Zhi.2013;93:3755-3757. [17] ZHANG W, LI N, CHEN S, et al. The effects of a tourniquet used in total knee arthroplasty: a metaanalysis. J Orthop Surg Res. 2014;9:13. [18] LEDIN H, ASPENBERG P, GOOD L. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. 2012;83:499-503. [19] TAI TW, CHANG CW, LAI KA, et al. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: A randomized controlled trial. J Bone Joint Surg Am. 2012; 94(24):2209-2215. [20] LI B, WEN Y, WU H, et al. The effectof tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33(5):1263-1268. [21] HARRIS LW, REID D, POWERS SK, et al. Tourniquet-induced skeletal muscle oxidative injury during lower limb orthopaedic trauma surgery. Bone Jt J. 2011;93:557. [22] PFITZNER T, VON ROTH P, VOERKELIUS N, et al. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:96-101. [23] BANWART JC, MCQUEEN DA, FRIIS EA, et al. Negative pressure intrusion cementing technique for total knee arthroplasty. J Arthroplasty. 2000; 15:360-367. [24] JAWHAR A, STETZELBERGER V, KOLLOWA K, et al. Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019; 27(7):2071-2081. [25] MITTAL R, KO V, ADIE S, et al. Tourniquet application only during cement fxation in total knee arthroplasty: a double-blind, randomized controlled trial. ANZ J Surg. 2012;82:428-433. [26] HASANAIN MS, APOSTU D, ALREFAEE A, et al. Comparing the effect of tourniquet vs tourniquet-less in simultaneousbilateral total knee arthroplasties. J Arthroplasty. 2018;33:2119-2124. [27] KUMAR N, YADAV C, SINGH S, et al. Evaluation of pain in bilateral total knee replacement withand without tourniquet; a prospective randomized control trial. J Clin Orthop Trauma. 2015;6:85-88. [28] EJAZ A, LAURSEN AC, KAPPEL A, et al. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014;85:422-426. [29] ALEXANDERSSON M, WANG EY, ERIKSSON S. A small difference in recovery between total knee arthroplasty with and without tourniquet use the frst 3 months after surgery: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2019;27:1035-1042. [30] HELLER S, CHEN A, RESTREPO C, et al. Tourniquet release prior to dressing application reduces blistering following total knee arthroplasty. J Arthroplasty.2015;30(7):1207-1210. [31] KOMATSU T, ISHIBASHI Y, OTSUKA H, et al. The effect of surgicall approache sand tourniquet tapplication on patella femoral tracking in total knee arthroplasty. J Arthroplasty. 2003;18(3):308-312. [32] VAISHYA R, AGARWAL AK, VIJAY V, et al. Short term outcomes of long duration versus short duration tourniquet in primary total knee arthroplasty: A randomized controlled trial. J Clin Orthop Trauma. 2018;9(1):46-50. |
| [1] | Zhang Jichao, Dong Yuefu, Mou Zhifang, Zhang Zhen, Li Bingyan, Xu Xiangjun, Li Jiayi, Ren Meng, Dong Wanpeng. Finite element analysis of biomechanical changes in the osteoarthritis knee joint in different gait flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1357-1361. |
| [2] | Jin Tao, Liu Lin, Zhu Xiaoyan, Shi Yucong, Niu Jianxiong, Zhang Tongtong, Wu Shujin, Yang Qingshan. Osteoarthritis and mitochondrial abnormalities [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1452-1458. |
| [3] | Wang Baojuan, Zheng Shuguang, Zhang Qi, Li Tianyang. Miao medicine fumigation can delay extracellular matrix destruction in a rabbit model of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1180-1186. |
| [4] | Liu Dongcheng, Zhao Jijun, Zhou Zihong, Wu Zhaofeng, Yu Yinghao, Chen Yuhao, Feng Dehong. Comparison of different reference methods for force line correction in open wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 827-831. |
| [5] | Huang Hao, Hong Song, Wa Qingde. Finite element analysis of the effect of femoral component rotation on patellofemoral joint contact pressure in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 848-852. |
| [6] | Yuan Jing, Sun Xiaohu, Chen Hui, Qiao Yongjie, Wang Lixin. Digital measurement and analysis of the distal femur in adults with secondary knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 881-885. |
| [7] | Zhou Jianguo, Liu Shiwei, Yuan Changhong, Bi Shengrong, Yang Guoping, Hu Weiquan, Liu Hui, Qian Rui. Total knee arthroplasty with posterior cruciate ligament retaining prosthesis in the treatment of knee osteoarthritis with knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 892-897. |
| [8] | Yang Yang, Li Naxi, Zhang Jian, Wang Mian, Gong Taifang, Gu Liuwei. Effect of tourniquet combined with exsanguination band use on short-term lower extremity venous thrombosis after knee arthroscopy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 898-903. |
| [9] | He Junjun, Huang Zeling, Hong Zhenqiang. Interventional effect of Yanghe Decoction on synovial inflammation in a rabbit model of early knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 694-699. |
| [10] | Lin Xuchen, Zhu Hainian, Wang Zengshun, Qi Tengmin, Liu Limin, Suonan Angxiu. Effect of xanthohumol on inflammatory factors and articular cartilage in a mouse mode of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 676-681. |
| [11] | Xu Lei, Han Xiaoqiang, Zhang Jintao, Sun Haibiao. Hyaluronic acid around articular chondrocytes: production, transformation and function characteristics [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 768-773. |
| [12] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [13] | Pan Jianke, Zhao Di, Jin Xiao, Yang Weiyi, Luo Minghui, Liu Jun, Han Yanhong, Cao Houran. Implant-related errors and complications in medial open-wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5849-5856. |
| [14] | Lin Zhiyu, Han Jie, Ren Guowu, Chai Yuan, Wen Shuaibo, Wu Yukun, Xie Xiaozhong, Jin Wanqing. Active components of flemingia in regulating the signaling pathways related to knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5889-5896. |
| [15] | Xin Daqi, Wang Guoqiang, Han Di, Xing Wenhua, Fu Yu, Zhu Yong, Zhou Yang, Bai Xianming, He Chenyang, Zhao Yan. Finite element simulation surgical modeling of Lenke 3 adult idiopathic scoliosis: modeling evaluation twice in 5 years [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5755-5763. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||