Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (6): 898-903.doi: 10.12307/2022.173
Previous Articles Next Articles
Effect of tourniquet combined with exsanguination band use on short-term lower extremity venous thrombosis after knee arthroscopy
Yang Yang1, Li Naxi1, Zhang Jian2, Wang Mian2, Gong Taifang3, Gu Liuwei4
- 1Postgraduate Training Basement of Jinzhou Medical University, Taihe Hospital (Affiliated Hospital of Hubei Medical College); 2Hubei Medical College; 3Department of Orthopedics, Joint and Sports Medicine, Taihe Hospital Affiliated to Hubei Medical College; 4Postgraduate Training Basement of Jinzhou Medical University, Shiyan People’s Hospital (Affiliated Hospital of Hubei Medical College)
-
Received:2021-05-19Revised:2021-05-20Accepted:2021-06-30Online:2022-02-28Published:2021-12-07 -
Contact:Gong Taifang, Professor, Master’s supervisor, Department of Orthopedics, Joint and Sports Medicine, Taihe Hospital Affiliated to Hubei Medical College, Shiyan 442000, Hubei Province, China -
About author:Yang Yang, Master candidate, Postgraduate Training Basement of Jinzhou Medical University, Taihe Hospital (Affiliated Hospital of Hubei Medical College), Shiyan 442000, Hubei Province, China
CLC Number:
Cite this article
Yang Yang, Li Naxi, Zhang Jian, Wang Mian, Gong Taifang, Gu Liuwei. Effect of tourniquet combined with exsanguination band use on short-term lower extremity venous thrombosis after knee arthroscopy[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 898-903.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
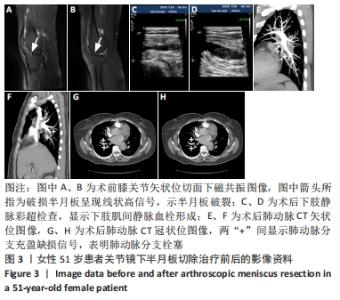
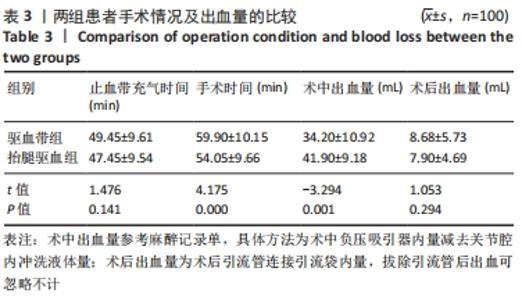
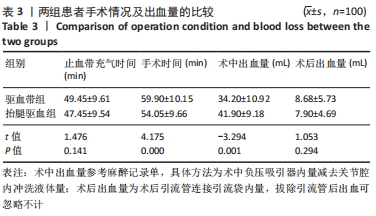
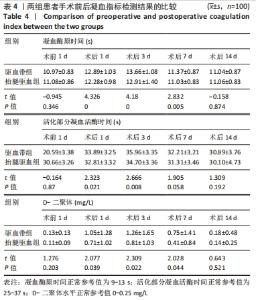
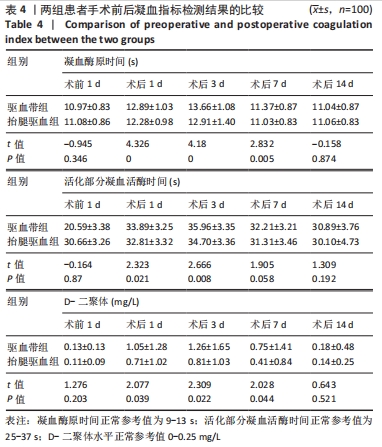
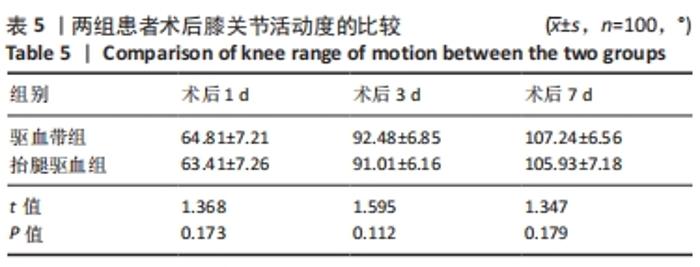
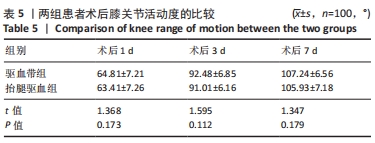
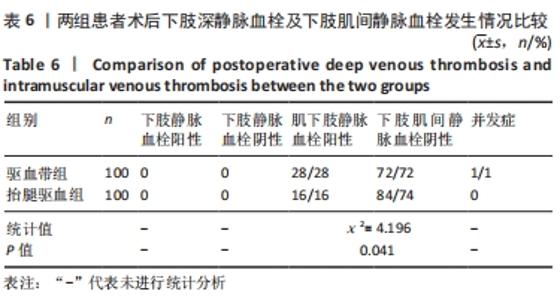
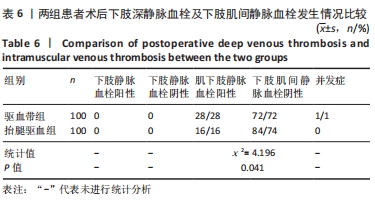
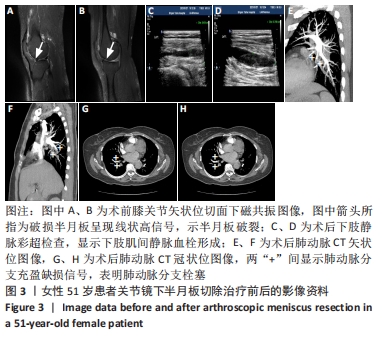
术后2 d常规行下肢静脉彩色多普勒超声检查,结果提示两组患者中均有下肢静脉血栓发生,且都为肌间静脉血栓,均未发现有严重的下肢深静脉血栓。驱血带组发生肌间静脉血栓患者有28例 ,发生率为28%;抬腿驱血组发生肌间静脉血栓患者有16例,发生率为16%,两组间肌间静脉血栓发生率比较差异有显著性意义(P < 0.05)。 两组患者均未出现下肢肿胀、肿痛、肤色变化等血栓栓塞相关典型临床表现。术后给予患者抬高患肢、禁止挤压、按摩、热敷患肢及抗凝等处理,其中驱血带组有1例患者在查出下肢肌间静脉血栓发生后因不遵医嘱私自下床活动而导致栓子脱落,继而发生肺动脉分支栓塞,出现胸闷、气促症状。 2.7 典型病例 51岁女性患者,无明显诱因出现左膝关节疼痛3个月,加重1周。入院后,左膝关节磁共振示左膝关节退变、左膝半月板损伤,见图3A、B。完善相关检查后,在腰硬联合麻醉下行关节镜下半月板切除治疗,术中使用驱血带进行驱血。术后2 d复查下肢静脉彩超,显示下肢肌间静脉血栓形成,见图3C、D。嘱患者暂卧床休息,患者于术后第3天夜间私自下床活动后忽感心慌、胸闷、气促,急查肺动脉造影CT检查,显示肺动脉分支栓塞,见图3E-H。"
| [1] 陈成帷,潘哲尔,周也立,等.常规止血带下膝关节镜手术后早期深静脉血栓的发生率及危险因素分析[J].中国骨伤,2018,31(9): 829-834. [2] SHIRVANIAN S, TAPSON VF. Venous thromboembolism: identifying patients at risk and establishing prophylaxis. Curr Med Res Opin. 2015; 31(12):2297-2311. [3] MINAKAWA M, FUKUDA I, MIYATA H, et al. Outcomes of Pulmonary Embolectomy for Acute Pulmonary Embolism. Circ J. 2018;82(8):2184-2190. [4] DAVISON S P, HAYES KD. Commentary on: Analysis of the American Society of Anesthesiologists Physical Status Classification System and Caprini Risk Assessment Model in Predicting Venous Thromboembolic Outcomes in Plastic Surgery Patients. Aesthet Surg J. 2016;36(4):506-507. [5] KRYCH AJ, SOUSA PL, MORGAN JA, et al. Incidence and Risk Factor Analysis of Symptomatic Venous Thromboembolism After Knee Arthroscopy. Arthroscopy. 2015;31(11):2112-2118. [6] SUN Y, CHEN D, XU Z, et al. Incidence of Symptomatic and Asymptomatic Venous Thromboembolism After Elective Knee Arthroscopic Surgery: A Retrospective Study With Routinely Applied Venography. Arthroscopy. 2014;30(7):818-822. [7] SARFANI S, CANTWELL S, SHIN A, et al. Challenging the Dogma of Tourniquet Pressure Requirements for Upper Extremity Surgery. J Wrist Surg. 2016;5(2):120-123. [8] SCHNETTLER T, PAPILLON N, REES H. Use of a Tourniquet in Total Knee Arthroplasty Causes a Paradoxical Increase in Total Blood Loss. J Bone Joint Surg. 2017;99(16):1331-1336. [9] RODRIGUEZ-COLLAZO ER, URSO ML. Combined use of the Ilizarov method, concentrated bone marrow aspirate (cBMA), and platelet-rich plasma (PRP) to expedite healing of bimalleolar fractures. Str Trauma Limb Rec. 2015;10(3):161-166. [10] MAEDA MPH, IWASE PH, KANDA MPA, et al. A study of the blood flow restriction pressure of a tourniquet system to facilitate development of a system that can prevent musculoskeletal complications. Am J Disaster Med. 2017;12(3):139-145. [11] 李嫚,李东红,徐宗慧.3种驱血方法在骨科上肢手术应用的对比研究[J].护理研究,2014,28(1):67-68. [12] 彭丽贞.不同驱血方法在骨科下肢手术中的应用研究[J].临床医学工程,2016,23(8):1123-1124. [13] ZHANG M, LIU G, ZHAO Z, et al. Comparison of lower limb lifting and squeeze exsanguination before tourniquet inflation during total knee arthroplasty. BMC Musculoskelet Disord. 2019;20(1):35. [14] SKOWRON M, KOCIUGA J, DOMZALSKI M. Electrostimulation has a positive effect on the knee function after knee arthroscopic surgery: A randomized trial. J Back Musculoskelet Reh. 2020;33(5):777. [15] BOGUNOVIC L, HAAS AK, BROPHY RH, et al. The Perioperative Continuation of Aspirin in Patients Undergoing Arthroscopic Surgery of the Knee. Am J Sports Med. 2019;47(9):2138-2142. [16] JUNG KH, YOUM YS, CHO SD, et al. Iatrogenic Medial Collateral Ligament Injury by Valgus Stress During Arthroscopic Surgery of the Knee. Arthroscopy. 2019;35(5):1520-1524. [17] MANNION AF, BIANCHI G, MARIAUX F, et al. Can the Charlson Comorbidity Index be used to predict the ASA grade in patients undergoing spine surgery? Eur Spine J. 2020;29(12):2941-2952. [18] SING DC, LUAN TF, FEELEY BT, et al. Is Obesity a Risk Factor for Adverse Events After Knee Arthroscopy? Arthroscopy. 2016;32(7):1346-1353. [19] LIU PL, LI DQ, ZHANG YK, et al. Effects of Unilateral Tourniquet Used in Patients Undergoing Simultaneous Bilateral Total Knee Arthroplasty. Orthop Surg. 2017;9(2):180-185. [20] HUANG G, TANG Y, WANG H, et al. Lower limb vein thrombosis-induced pulmonary embolism and paradoxical multiple arterial embolisms: A case report with a 10-year follow-up. Medicine (Baltimore). 2019; 98(30):e16522. [21] JOHNSON AP, KOGANTI D, WALLACE A, et al. Asymptomatic Trauma Patients Screened for Venous Thromboembolism Have a Higher Risk Profile with Lower Rate of Pulmonary Embolism: A Five-Year Single-Institution Experience. Am Surg. 2020;86(2):104-109. [22] CHOPARD R, ALBERTSEN IE, PIAZZA G. Diagnosis and Treatment of Lower Extremity Venous Thromboembolism: A Review. JAMA. 2020; 324(17):1765-1776. [23] ZHAO Z, MA J, MA X. Comparative efficacy and safety of different hemostatic methods in total hip arthroplasty: a network meta-analysis. J Orthop Surg Res. 2019;14(1):1-10. [24] LALONE EA, GREWAL R, KING GJW, et al. A Structured Review Addressing the Use of Radiographic Measures of Alignment and the Definition of Acceptability in Patients with Distal Radius Fractures. Hand (N Y). 2015;10(4):621-638. [25] COLLEONI JL, RIBEIRO FN, MOS P, et al. Venous thromboembolism prophylaxis after total knee arthroplasty (TKA): aspirin vs. rivaroxaban. Rev Bras Ortop. 2018;53(1):22-27. [26] ZHAO X, ALI SJ, SANG X. Clinical Study on the Screening of Lower Extremity Deep Venous Thrombosis by D-Dimer Combined with RAPT Score Among Orthopedic Trauma Patients. Indian J Orthop. 2020; 54(S2):316-321. [27] CHENG J, FU Z, ZHU J, et al. The predictive value of plasminogen activator inhibitor-1, fibrinogen, and D-dimer for deep venous thrombosis following surgery for traumatic lower limb fracture. Ann Palliat Med. 2020;9(5):3385-3392. [28] ABDULKARIM A, KRAUSE KE, SHEEHAN E. Pain and functional outcomes with tourniquet use in total knee arthroplasty. Irish J Med Sci. 2015; 184:S201. [29] 曹青刚,包倪荣,赵建宁.止血带导致全膝关节置换术后肢体肿痛机制的研究进展[J].医学研究生学报,2019,32(4):428-431. [30] GOCER H, YAZICI AK, POLAT AV. Should venous doppler ultrasonography be routinely applied before lower extremity major orthopedic surgery? Niger Med J. 2017;58(1):32-36. [31] ZAN P, MOL MO, YAO JJ, et al. Release of the tourniquet immediately after the implantation of the components reduces the incidence of deep vein thrombosis after primary total knee arthroplasty. Bone Joint Res. 2017;6(9):535-541. [32] MORI N, KIMURA S, ONODERA T, et al. Use of a pneumatic tourniquet in total knee arthroplasty increases the risk of distal deep vein thrombosis: A prospective, randomized study. knee. 2016;23(5):887-889. [33] ISHII Y, NOGUCHI H, SATO J, et al. Impact of anesthesia modality and mechanical venous thromboembolism prophylaxis on the incidence of symptomatic deep venous thrombosis after TKA. J Clin Orthop Trauma. 2018;9(2):142-145. [34] 尹健东,王鑫灵,左彪,等.全膝关节置换过程中挤压驱血和抬腿驱血与置换后并发症的关系[J].中国组织工程研究,2020,24(9):1331-1336. [35] WRIGHT AA, TAYLOR JB, FORD KR, et al. Risk factors associated with lower extremity stress fractures in runners: a systematic review with meta-analysis. Br J Sports Med. 2015;49(23):1517-1523. [36] ARSOY D, GIORI NJ, WOOLSON ST. Mobile Compression Reduces Bleeding-related Readmissions and Wound Complications After THA and TKA. Clin Orthop Relat Res. 2018;476(2):381-387. [37] ISSA K, PIERCE T P, HARWIN SF, et al. No Decrease in Knee Survivorship or Outcomes Scores for Patients With HIV Infection Who Undergo TKA. Clin Orthop Relat Res. 2017;475(2):465-471. [38] LIU Y, SI H, ZENG Y, et al. More pain and slower functional recovery when a tourniquet is used during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1842-1860. [39] ALONSO-ALGARABEL M, ESTEBAN-SEBASTIÀ X, SANTILLÁN-GARCÍA A, et al. Tourniquet use in out-of-hospital emergency care: a systematic review. Emergencias. 2019;31(1):47-54. |
| [1] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [2] | Hu Shouye, Yang Zhi, Hao Yangquan, Lu Chao, Zhang Qiong, Zhang Weisong, Zhu Yujie, Peng Kan. Tourniquet use in the first half-course of total knee arthroplasty does not affect postoperative functional outcomes or pain: a prospective, randomized controlled trial [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4327-4332. |
| [3] | Deng Bo, Hong Hainan, Fan Yongyong, Cai Guoping, Feng Xingbing, Hong Zhenghua. Efficacy and safety of tourniquet application in total knee arthroplasty and only at the time of cementing: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2908-2914. |
| [4] | Song Min, Lu Chao, Chen Jin, Wu Gaoyi, Li Congcong, Li Anan, Ye Guozhu, Lin Wenzheng, Cai Yuning, Liu Wengang, Xu Weipeng. Application of tourniquet affects thickness of bone cement penetration in total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1917-1923. |
| [5] | Sun Kai, Chen Lei, Mai Yao, Hu Hua, Chen Liang, Zhong Jun, Hu Yong, Qiu Bo. Clinical application of enhanced recovery after surgery in the perioperative period of anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(11): 1647-1651. |
| [6] |
Yin Jiandong, Wang Xinling, Zuo Biao, Li Nongyi.
Relationship of extrusion and elevation of blood-expelling methods during
total knee arthroplasty with postoperative complications |
| [7] | Zhang Hui, Li Hong, Li Yetian, Lu Ming, Yin Li, Gao Weilu, Liu Jingjun, Liu Biquan, Yin Zongsheng. Comparison of early joint amnesia degree after posterior cruciate-retaining and posterior stabilized total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(30): 4802-4806. |
| [8] | Wang Hairuo, Liu Xi, Li Mingjin, Chen Xiaohua, Liang Ting, Ding Yongqing, Tang Xiaoli, Wang Ji, Ma Huixu. Effects of intravenous tranexamic acid infusion combined with articular cavity injection on pain and early rehabilitation after knee arthroscopy [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(36): 5766-5771. |
| [9] | Peng Chenjian, Du Bin, Sun Guangquan, Liu Xin, He Bing. Usage strategy of optimized tourniquet in enhanced recovery after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(28): 4451-4455. |
| [10] | Wang Xinling, Tan Biao, Yin Jiandong, Zuo Biao. Restrictive use and non-use tourniquets during total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(28): 4456-4460. |
| [11] |
Yang Shuo, Feng Shuo, Xu Chongjun, Tang Jinlong, Pei Fang, Zha Guochun, Chen Xiangyang.
Relationship of lower limb alignment and component alignment with outcomes and implant loosening rate after total knee arthroplasty
[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(24): 3780-3785.
|
| [12] | Zhao Juntao, Zheng Chengsheng, Wang Bo. Optimized use of tourniquet in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(20): 3124-3129. |
| [13] | Zhou Jianguo, Hu Weiquan, Bi Shengrong, Hu Bijuan, Liu Shiwei, Xiong Long, Qian Rui. Clinical application of individualized tourniquet pressure in primary total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(20): 3136-3142. |
| [14] | Zhou Hongxing, Yi Weiguo, Yuan Xiangsheng. Correlation of different treatment methods of synovial membrane in total knee arthroplasty with the joint function recovery [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(16): 2461-2466. |
| [15] | Lu Yao-jia, Xiong Chuan-zhi, Li Xiao-lei, Hu Han-sheng, Chen Gang, Wang Qiang, Lu Zhi-hua. Comparison of two methods for reducing blood loss during total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2017, 21(7): 1004-1008. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||