Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (36): 5837-5843.doi: 10.12307/2022.799
Previous Articles Next Articles
Distribution, drug resistance, and clinical characteristics of pathogenic bacteria in 102 cases of periprosthetic joint infection
Jiang Xu, Cao Fuyang, Xiong Ao, Yang Meng, Tan Jun, Yu Yang, Zhang Shaokun, Xu Jianzhong
- Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China
-
Received:2021-12-04Accepted:2022-01-13Online:2022-12-28Published:2022-04-27 -
Contact:Xu Jianzhong, MD, Chief physician, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China -
About author:Jiang Xu, Master candidate, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province, China
CLC Number:
Cite this article
Jiang Xu, Cao Fuyang, Xiong Ao, Yang Meng, Tan Jun, Yu Yang, Zhang Shaokun, Xu Jianzhong. Distribution, drug resistance, and clinical characteristics of pathogenic bacteria in 102 cases of periprosthetic joint infection[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5837-5843.
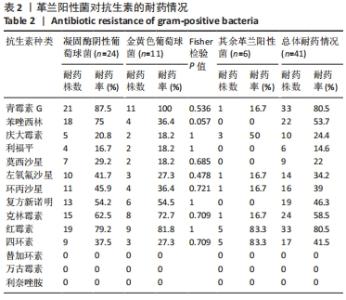
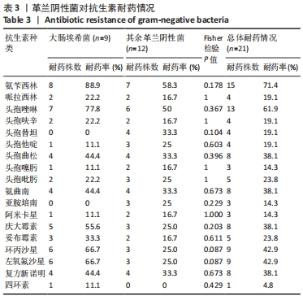
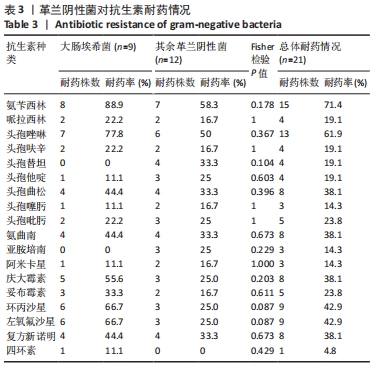
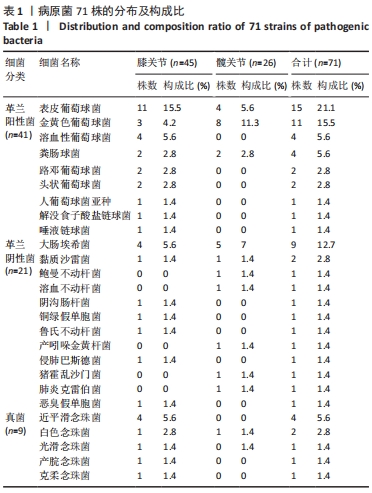
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

2.1 假体周围感染患者基本资料 纳入102例明确诊断为假体周围感染的病例资料,66例患者病原菌培养阳性,36例患者病原菌培养阴性,培养阳性率为64.7%,每例患者2次培养结果均一致。患者平均年龄为(66.3±10.6)岁;男性45例(44.1%),女性57例(55.9%);患有高血压45例(44.1%)、糖尿病25例(24.5%)。感染部位:膝关节71例(69.6%),髋关节31例(30.4%)。存在与感染关节相通窦道者21例(20.6%)。感染分期:早期感染者46例(45.1%),迟发感染者20例(19.6%),晚期感染者36例(35.3%)。治疗方式有:保留假体清创术17例(16.7%),一期翻修例26例(25.5%),二期翻修例59例(57.8%)。术后至少12个月的随访,102例患者中11例(10.8%)术后1年内出现感染症状复发。 2.2 假体周围感染患者病原菌种类及分布 66例培养阳性病例,共计检出71株病原菌,其中5例患者为混合感染,分别为阴沟肠杆菌+铜绿假单胞菌、大肠埃希菌+金黄色葡萄球菌、人葡萄球菌亚种+表皮葡萄球菌、大肠埃希菌+猪霍乱沙门菌、表皮葡萄球菌+粪肠球菌。 全部病原菌中,革兰阳性菌41株,占比57.8%,其中表皮葡萄球菌(21.1%)和金黄色葡萄球菌(15.5%)最常见;革兰阴性菌21株,占比29.6%,其中大肠埃希菌(12.7%)最常见;真菌9株,占比12.7%,其中近平滑念珠菌(5.6%)最常见。 在膝关节中,革兰阳性菌占比60%(27/45),革兰阴性菌占比22.2%(10/45),真菌占比17.8%(8/45);在髋关节中,革兰阳性菌占比53.8%(14/26),革兰阴性菌占比42.3%(11/26),真菌占比3.8%(1/26)。膝、髋病原菌分布比较差异无显著性意义(P=0.087),见表1。 "

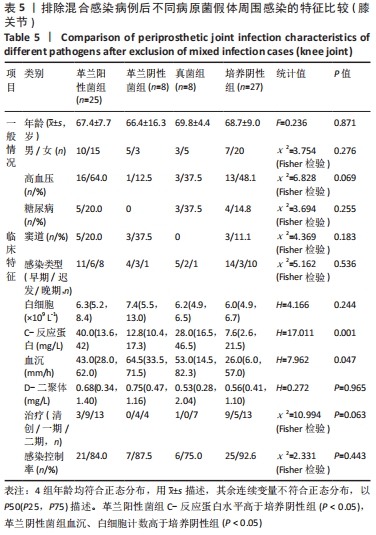
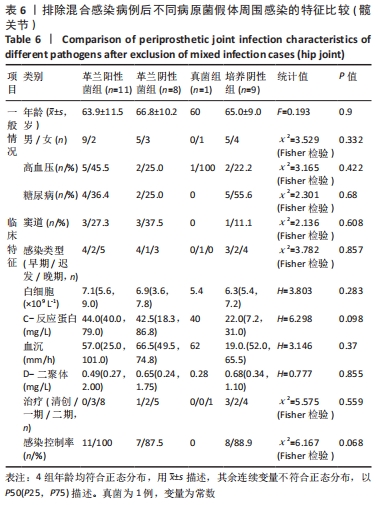
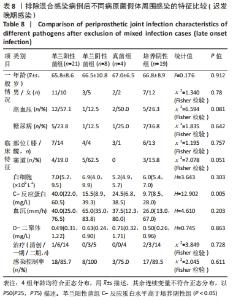
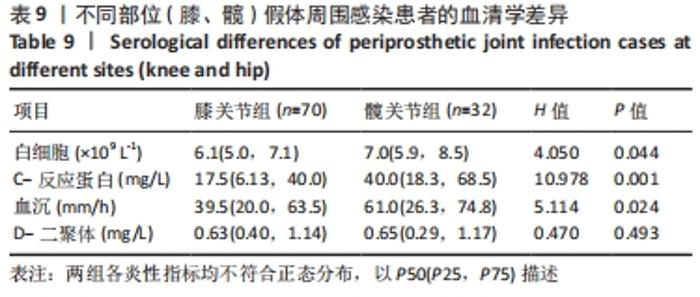
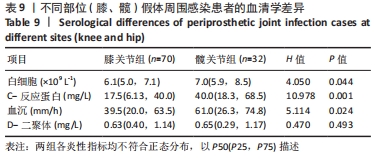
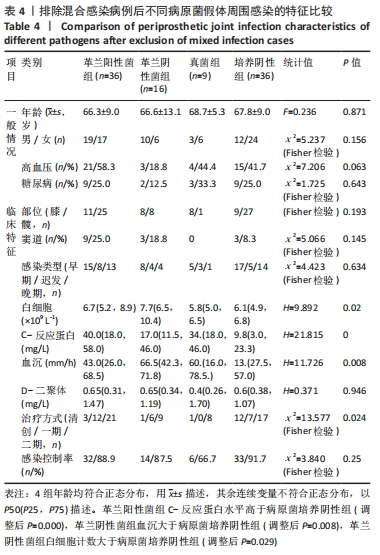
2.3.3 真菌耐药情况 药敏试验未发现耐药菌株。 2.4 假体周围感染患者不同病原菌培养结果间的特征差异 排除5例混合感染病例后,其余97例以病原菌培养结果分为革兰阳性菌36例、革兰阴性菌16例、真菌9例及培养阴性36例共4组,4组在年龄、部位、高血压、糖尿病、窦道、D-二聚体、感染时间、感染控制情况等方面比较差异无显著性意义(P > 0.05)。此外Fisher精确检验结果显示,4组在治疗方式(清创/一期/二期)选择上存在统计学差异(P < 0.05),但采用Bonferroni调整后分析显示,4组在治疗方式(清创/一期/二期)选择上组间成对比较差异无显著性意义(P > 0.05)。4组在炎症指标(白细胞、血沉、C-反应蛋白)方面比较差异有显著性意义(P < 0.05),进一步分析(组间成对比较,用Bonferroni法校正显著性水平)结果:①C-反应蛋白:革兰阳性菌组C-反应蛋白水平高于病原菌培养阴性组(调整后P=0.000),其余组间比较差异无显著性意义(P > 0.05);②血沉:革兰阴性菌组血沉大于病原菌培养阴性组(调整后P=0.008),其余组间比较差异比较无显著性意义(P > 0.05);③白细胞计数:革兰阴性菌组白细胞计数大于病原菌培养阴性组(调整后P=0.029),其余组间比较差异无显著性意义(P > 0.05),见表4。"
| [1] 边焱焱,程开源,常晓,等.2011至2019年中国人工髋膝关节置换手术量的初步统计与分析[J].中华骨科杂志,2020,40(21):1453-1460. [2] KURTZ SM, ONG KL, LAU E, et al. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat R. 2010;468(1):52-56. [3] DALE H, HALLAN G, HALLAN G, et al. Increasing risk of revision due to deep infection after hip arthroplasty. Acta Orthop. 2009;80(6):639-645. [4] BAEK SH. Identification and preoperative optimization of risk factors to prevent periprosthetic joint infection. World J Orthop. 2014;5(3):362-367. [5] BEAM E, OSMON D. Prosthetic Joint Infection Update. Infect Dis Clin N Am. 2018; 32(4):843-859. [6] LI ZL, HOU YF, ZHANG BQ, et al. Identifying Common Pathogens in Periprosthetic Joint Infection and Testing Drug-resistance Rate for Different Antibiotics: A Prospective, Single Center Study in Beijing. Orthop Surg. 2018;10(3): 235-240. [7] 周一逸,刘仪,袁鹏,等.骨关节置换术后假体周围感染的病原菌特征及影响因素分析[J].中华医院感染学杂志,2019,29(14):2189-2193. [8] CHOI HR, KWON YM, FREIBERG AA, et al. Periprosthetic joint infection with negative culture results: clinical characteristics and treatment outcome. J Arthroplasty. 2013;28(6):899-903. [9] PARVIZI J, GEHRKE T, CHEN AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013;95-B(11):1450-1452. [10] KAPADIA BH, BERG RA, DALEY JA, et al. Periprosthetic joint infection. Lancet (London, England). 2016;387(10016):386-394. [11] MORAN E, MASTERS S, BERENDT AR, et al. Guiding empirical antibiotic therapy in orthopaedics: The microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J Infect. 2007;55(1):1-7. [12] KALBIAN I, PARK JW, GOSWAMI K, et al. Culture-negative periprosthetic joint infection: prevalence, aetiology, evaluation, recommendations, and treatment. Int Orthop. 2020;44(7):1255-1261. [13] LIU H, ZHANG Y, LI L, et al. The application of sonication in diagnosis of periprosthetic joint infection. Eur J Clin Microbiol Infect Dis. 2017;36(1):1-9. [14] 于洋,张少坤,陆世涛,等.宏基因组二代测序技术在假体周围感染病原诊断中的应用[J].中华骨科杂志,2021,41(5):280-288. [15] 崔苛苛,杨伟毅,刘军,等.全膝关节置换后假体周围感染病原菌分布特点及治疗策略[J].中国组织工程研究,2017,21(35):5721-5726. [16] 程翔,梁玉龙,邵宏翊,等.假体周围感染病原菌及耐药性分析[J].中国矫形外科杂志,2020,28(11):870-875. [17] TSAI Y, CHANG CH, LIN YC, et al. Different microbiological profiles between hip and knee prosthetic joint infections. J Orthop Surg (Hong Kong). 2019;27(2): 2309499019847768. [18] BROWN TS, PETIS SM, OSMON DR, et al. Periprosthetic Joint Infection With Fungal Pathogens. J Arthroplasty. 2018;33(8):2605-2612. [19] ESCOLÀ-VERGÉ L, RODRÍGUEZ-PARDO D, LORA-TAMAYO J, et al. Candida periprosthetic joint infection: A rare and difficult-to-treat infection. J Infect. 2018; 77(2):151-157. [20] TÓTH R, NOSEK J, MORA-MONTES HM, et al. Candida parapsilosis: from Genes to the Bedside. Clin Microbiol Rev. 2019;32(2):e00111-00118. [21] 王加利,张燕,蔺伟,等.人工关节置换术后假体感染的病原学分析[J].中华医院感染学杂志,2014, 24(9):2251-2253. [22] 赵欣宇,陈廖斌,谭杨,等.利福平在人工关节假体周围感染治疗中的应用[J].中华骨科杂志,2016,36(19):1263-1267. [23] NISCHAL PM. First global report on antimicrobial resistance released by the WHO. Natl Med J India. 2014;27(4):241. [24] WIJESEKARA PNK, KUMBUKGOLLA WW, JAYAWEERA JAAS, et al. Review on Usage of Vancomycin in Livestock and Humans: Maintaining Its Efficacy, Prevention of Resistance and Alternative Therapy. Vet Sci. 2017;4(1):6. [25] KHEIR MM, TAN TL, SHOHAT N, et al. Routine Diagnostic Tests for Periprosthetic Joint Infection Demonstrate a High False-Negative Rate and Are Influenced by the Infecting Organism. J Bone Joint Surg Am. 2018;100(23):2057-2065. [26] PARVIZI J, DELLA VALLE CJ. AAOS Clinical Practice Guideline: diagnosis and treatment of periprosthetic joint infections of the hip and knee. J Am Acad Orthop Surg. 2010;18(12):771-772. [27] HARTMAN MB, FEHRING TK, JORDAN L, et al. Periprosthetic knee sepsis. The role of irrigation and debridement. Clin Orthop Relat Res. 1991;(273):113-118. [28] BEROZ F, YAN J, SABASS B, et al. Verticalization of bacterial biofilms. Nat Phys. 2018;14(9):954-960. [29] BERBARI EF, MARCULESCU C, SIA I, et al. Culture-negative prosthetic joint infection. Clin Infect Dis. 2007;45(9):1113-1119. [30] NACE J, SIDDIQI A, TALMO CT, et al. Diagnosis and Management of Fungal Periprosthetic Joint Infections. J Am Acad Orthop Surg. 2019;27(18):e804-e818. [31] MCARTHUR BA, ABDEL MP, TAUNTON MJ, et al. Seronegative infections in hip and knee arthroplasty: periprosthetic infections with normal erythrocyte sedimentation rate and C-reactive protein level. Bone Joint J. 2015;97-B(7):939-944. [32] 何金,袁雪凌,陈歌.细菌培养结果对髋假体周围感染翻修结果的影响[J].中国矫形外科杂志,2020,28(23):2127-2130. [33] LEE YS, LEE YK, HAN SB, et al. Natural progress of D-dimer following total joint arthroplasty: a baseline for the diagnosis of the early postoperative infection. J Orthop Surg Res. 2018;13(1):36. [34] HU Q, FU Y, TANG L. Serum D-dimer as a diagnostic index of PJI and retrospective analysis of etiology in patients with PJI. Clin Chim Acta. 2020;506:67-71. |
| [1] | Li Jiajun, Xia Tian, Liu Jiamin, Chen Feng, Chen Haote, Zhuo Yinghong, Wu Weifeng. Molecular mechanism by which icariin regulates osteogenic signaling pathways in the treatment of steroid-induced avascular necrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 780-785. |
| [2] | Liang Haoran, Zhou Xin, Yang Yanfei, Niu Wenjie, Song Wenjie, Ren Zhiyuan, Wang Xueding, Liu Yang, Duan Wangping. Pathogenesis of femoral head necrosis after internal fixation of femoral neck fractures in young adults [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 456-460. |
| [3] | Zhang Zihan, Wang Wenli, Li Jinnuo, Li Yourui. Carvacrol: antibacterial activity, bone repair, and prevention and treatment in oral diseases [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(26): 4252-4257. |
| [4] | Li Shuyuan, Chen Leilei, Huang Linfeng, Zhao Heran, Wu Suwen, Jiang Yuankang. Periprosthetic joint infection of hip and knee [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5859-5866. |
| [5] | Wang Chuan, Peng Wuxun. Participation and regulation of long-chain non-coding RNA on pathogenesis of avascular necrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(33): 5381-5387. |
| [6] | Fan Chongshan, Sun Mingshuai, Han Wenchao. Proinflammatory factors and matrix metalloproteinases: status and roles in the pathogenesis of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(32): 5162-5170. |
| [7] | Gao Tianhao, Qian Huifang, Yang Shangliang, Xin Chaofei, Lu Shitao, Xu Jianzhong. Calcium sulfate antibiotic carrier in the treatment of periprosthetic infection after arthroplasty and its effect on serum calcium [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4823-4827. |
| [8] | Ma Rui, Wang Jialin, Wu Mengjun, Ge Ying, Wang Wei, Wang Kunzheng. Relationship of pathogenic bacteria distribution with drug resistance and treatment cycle for periprosthetic joint infection after total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 380-385. |
| [9] | Cheng Chongjie, Yan Yan, Zhang Qidong, Guo Wanshou. Diagnostic value and accuracy of D-dimer in periprosthetic joint infection: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3921-3928. |
| [10] | Xu Qi, Zhang Chao, Ha Chengzhi, Wang Dawei. Susceptibility genes related to non-traumatic femoral head necrosis: improving detection accuracy and developing new treatment strategy [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(5): 747-752. |
| [11] | Guo Juan, Zheng Shan, Xie Hui, Hu Yahui. An analysis of pathogenic bacteria infection in 422 kidney transplant recipients [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(32): 5198-5202. |
| [12] | Cao Houran, Deng Peng, Ye Pengcheng, Jie Ke, Zeng Jianchun, Feng Wenjun, Chen Jinlun, Qi Xinyu, Li Jie, Tan Xueqiu, Zhang Haitao, Zeng Yirong. Platelet count as a novel potential predictor of periprosthetic joint infection [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(30): 4795-4801. |
| [13] |
Wang Zhen, Li Xiaolan, Liu Jianguo.
Insights into immunoregulatory properties of dental-derived mesenchymal stem cells in oral diseases [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(25): 4060-4067. |
| [14] | Liang Chenliang, Zhao Zhenqun, Liu Wanlin. The role of OPG/RANKL/RANK signaling pathway in the pathogenesis of giant-cell tumor of bone [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(23): 3723-3729. |
| [15] | Li Shibin, Zhang Xiaoyun, Zhang Xuan. Mechanism of autophagy in osteosarcoma [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(21): 3409-3415. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||