Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (10): 1555-1560.doi: 10.12307/2022.203
Previous Articles Next Articles
Dermal extracellular matrix hydrogel in promoting acute skin wound healing in rats
Dong Hongfei1, 2, Huang Qilin2, Yang Xiong2, Li Shuai2, Gu Rui2, Sun Hongyu2, Tang Lijun1, 2
- 1Department of School of Clinical Medicine, Southwest Medical University, Luzhou 646000, Sichuan Province, China; 2Department of General Surgery & Pancreatic Injury and Repair Key Laboratory of Sichuan Province, General Hospital of Western Theater Command, Chengdu 610083, Sichuan Province, China
-
Received:2020-10-10Revised:2020-10-13Accepted:2020-11-21Online:2022-04-08Published:2021-10-25 -
Contact:Tang Lijun, MD, Chief physician, Department of School of Clinical Medicine, Southwest Medical University, Luzhou 646000, Sichuan Province, China; Department of General Surgery & Pancreatic Injury and Repair Key Laboratory of Sichuan Province, General Hospital of Western Theater Command, Chengdu 610083, Sichuan Province, China -
About author:Dong Hongfei, Master, Department of School of Clinical Medicine, Southwest Medical University, Luzhou 646000, Sichuan Province, China; Department of General Surgery & Pancreatic Injury and Repair Key Laboratory of Sichuan Province, General Hospital of Western Theater Command, Chengdu 610083, Sichuan Province, China -
Supported by:the Military Construction Project for National Clinical Key Speciality, No. 41732113 (to TLJ); the Series Study on Graded Treatment of Abdominal Trauma and Organ Function Repair, No. 2019LH04 (to SHY)
CLC Number:
Cite this article
Dong Hongfei, Huang Qilin, Yang Xiong, Li Shuai, Gu Rui, Sun Hongyu, Tang Lijun. Dermal extracellular matrix hydrogel in promoting acute skin wound healing in rats[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1555-1560.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

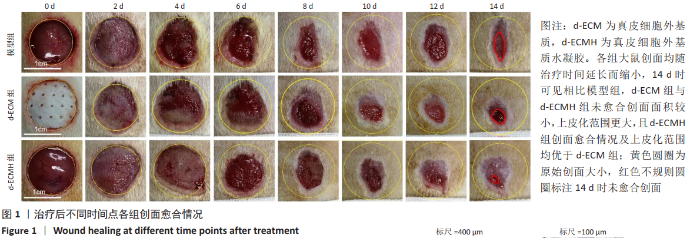
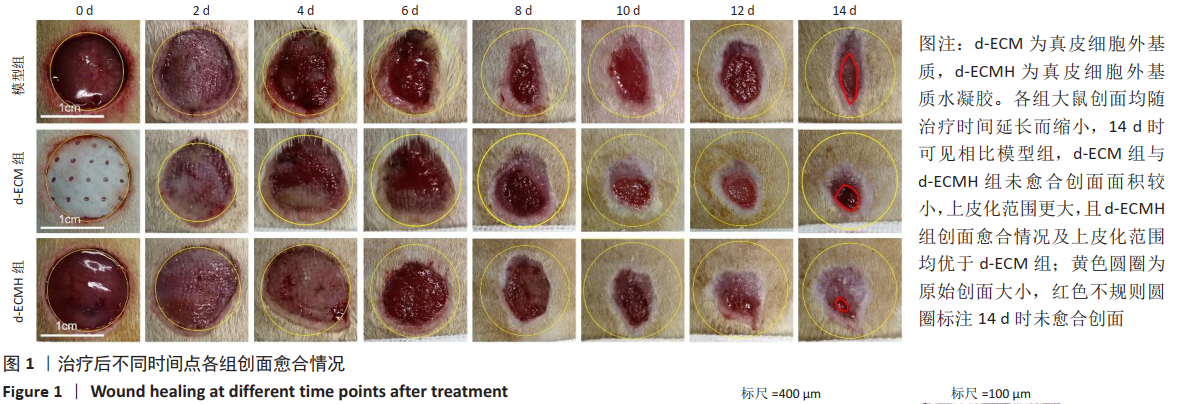
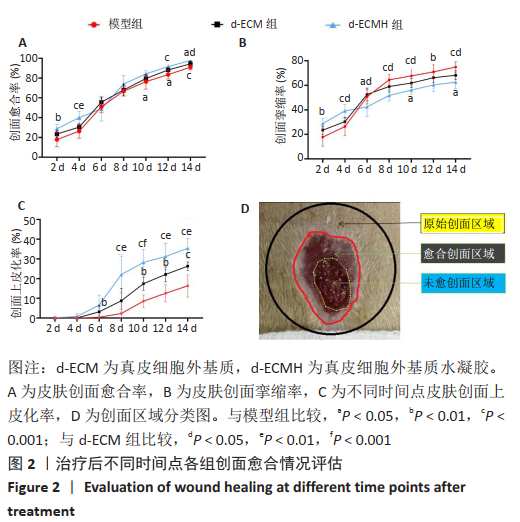
d-ECMH组与d-ECM组治疗14 d后的创面愈合率均高于模型组[模型组(91.00±2.75)%,d-ECM组(94.41±2.76)%, d-ECMH组(97.84±1.39)%,P < 0.05],且d-ECMH组高于d-ECM组(P < 0.05),见图2A。d-ECMH组与d-ECM组治疗14 d后的创面挛缩比率均低于模型组[模型组(74.87±4.18)%,d-ECM组(68.2±3.54)%,d-ECMH组(62.56±5.06)%,P < 0.05],且 d-ECMH组低于d-ECM组(P < 0.05),见图2B。此外发现,d-ECMH组与d-ECM组治疗14 d后的创面上皮化率显著高于模型组[模型组(16.31±5.66)%,d-ECM组(26.31±2.11)%,d-ECMH组(35.39± 5.15)%,P < 0.001],且d-ECMH组高于d-ECM组 (P < 0.01),见图2C。创面区域分类图见图2D。"
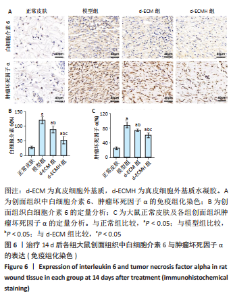
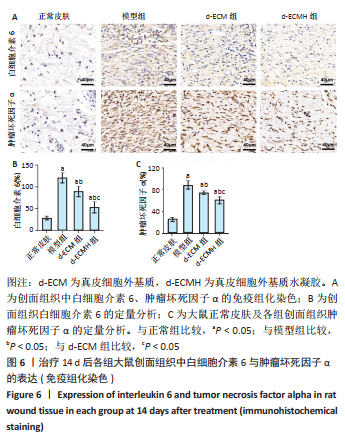
2.6 各组大鼠皮肤组织中白细胞介素6与肿瘤坏死因子α的表达 皮肤免疫组化染色结果显示,相比正常皮肤,模型组、d-ECM组及d-ECMH组皮肤组织中白细胞介素6与肿瘤坏死因子α均处于升高水平[白细胞介素6表达情况:正常皮肤(28.75±4.30) %,模型组(120.75±12.04)%,d-ECM组(89.50±11.39)%,d-ECMH组(53.04±13.14)%;肿瘤坏死因子α表达情况:正常皮肤(25.00±4.55)%,模型组(88.50±8.23)%,d-ECM组(74.25±3.59)%,d-ECMH组(60.51±6.61)%,P 均< 0.05]。相比模型组,d-ECM组与d-ECMH组皮肤创面内白细胞介素6与肿瘤坏死因子α表达降低(P < 0.05)。此外,相比d-ECM组,d-ECMH组肤创面内白细胞介素6与肿瘤坏死因子α表达更低(P < 0.05),见图6。"

2.7 各组大鼠皮肤组织中巨噬细胞极化表型分析 正常皮肤组织中M1型巨噬细胞与M2型巨噬细胞均处于较低水平[M1型巨噬细胞(11.25±1.50)个/视野,M2型巨噬细胞(13.25±1.50)个/视野]。模型组、d-ECM组及d-ECMH组创面组织内M1型巨噬细胞均高于正常皮肤[模型组(45.00±8.08)个/视野,d-ECM组(36.50±3.87)个/视野,d-ECMH组(24.25±6.13)个/视野,P < 0.05]。模型组与d-ECM组创面组织中M1型巨噬细胞数比较差异无显著性意义(P > 0.05),d-ECMH创面组织内M1型巨噬细胞数目少于模型组、d-ECM组(P < 0.05)。模型组、d-ECM组及d-ECMH组创面组织内M2型巨噬细胞均高于正常皮肤[模型组(26.75±6.34)个/视野,d-ECM组(43.25±5.79)个/视野,d-ECMH组(66.50± 8.89)个/视野,P < 0.05]。与模型组比较,d-ECM组及d-ECMH创面组织内M2型巨噬细胞数增多(P < 0.05),且d-ECMH组创面组织内M2型巨噬细胞较d-ECM组多(P < 0.05),见图7。 2.8 材料生物相容性 由创面愈合与组织形态观察可知,d-ECM与d-ECMH具有良好的组织相容性。"

| [1] WANG RM, CHRISTMAN KL. Decellularized myocardial matrix hydrogels: In basic research and preclinical studies. Adv Drug Deliv Rev. 2016;96:77-82. [2] WASSENAAR JW, GAETANI R, GARCIA JJ, et al. Evidence for Mechanisms Underlying theFunctional Benefits of a Myocardial Matrix Hydrogel for Post-MI Treatment. J Am Coll Cardiol. 2016;67(9):1074-1086. [3] JIANG J, ZHANG C, ZHANG T, et al. Research progress of decellularized extracellular matrix hydrogel in regenerative medicine. J Biomed Eng. 2020;37(1):179-184. [4] VENTURA RD, PADALHIN AR, PARK CM, Et al. Enhanced decellularization technique of porcine dermal ECM for tissue engineering applications. Mater Sci Eng C Mater Biol Appl. 2019;104:109841. [5] WON JY, LEE MH, KIM MJ, et al. A potential dermal substitute using decellularized dermis extracellular matrix derived bio-ink. Artif Cells Nanomed Biotechnol. 2019; 47(1):644-649. [6] ZHANG Z, LV L, MAMAT M, et al. Xenogenic (porcine) acellular dermal matrix promotes growth of granulation tissues in the wound healing of Fournier gangrene. Am Surg. 2015;81(1):92-95. [7] REING JE, BROWN BN, DALY KA, et al. The effects of processing methods upon mechanical and biologic properties of porcine dermal extracellular matrix scaffolds. Biomaterials. 2010;31(33):8626-8633. [8] ZHANG Y, HE Y, BHARADWAJ S, et al. Tissue-specific extracellular matrix coatings for the promotion of cell proliferation and maintenance of cell phenotype. Biomaterials. 2009;30(23-24):4021-4028. [9] LIN CY, LIU TY, CHEN MH, et al. An injectable extracellular matrix for the reconstruction of epidural fat and the prevention of epidural fibrosis. Biomed Mater. 2016;11(3):035010. [10] HAO D, LIU R, GAO K, et al. Developing an Injectable Nanofibrous Extracellular Matrix Hydrogel With an Integrin αvβ3 Ligand to Improve Endothelial Cell Survival, Engraftment and Vascularization. Front Bioeng Biotechnol. 2020;8:890. [11] NARANJO JD, SALDIN LT, SOBIESKI E, et al. Esophageal extracellular matrix hydrogel mitigates metaplastic change in a dog model of Barrett’s esophagus. Sci Adv. 2020;6(27):eaba4526. [12] WOLF MT, DALY KA, BRENNAN-PIERCE EP, et al. A hydrogel derived from decellularized dermal extracellular matrix. Biomaterials. 2012;33( 29):7028-7038. [13] 吴鹏飞,施光清,范贤明,等.肺细胞外基质水凝胶治疗大鼠放射性肺损伤的实验研究[J].中国现代医学杂志,2019,29(12):1-6. [14] 赵京禹,付小兵,雷永红,等.大鼠小面积全层皮肤缺损创面模型的制备[J].感染·炎症·修复,2008,9(1):64-64. [15] GURTNER GC, WERNER S, BARRANDON Y, et al. Wound Repair and Regeneration. Nature. 2008;453(7193):314-321. [16] CHEN X, SHI Y, SHU B, et al. The effect of porcine ADM to improve the burn wound healing. Int J Clin Exp Pathol. 2013;6(11):2280-2291. [17] 井刚,潘云川,王君.异种脱细胞真皮结合封闭负压引流技术临时重建巨大Ⅲ型腹壁缺损[J].组织工程与重建外科杂志,2020,16(1):43-45. [18] BORDBAR S, BAKHSHAIESH NL, KHANMOHAMMADI M, et al. Production and evaluation of decellularized extracellular matrix hydrogel for cartilage regeneration derived from knee cartilage. J Biomed Mater Res A. 2020;108(4):938-946. [19] TRAVERSE JH, HENRY TD, DIB N, et al. First-in-Man Study of a Cardiac Extracellular Matrix Hydrogel in Early and Late Myocardial Infarction Patients. JACC Basic Transl Sci. 2019;4(6):659-669. [20] CHEN G, YU Y, WU X, et al. Bioinspired Multifunctional Hybrid Hydrogel Promotes Wound Healing. Adv Funct Mater. 2018;28(33):1801386. [21] BONDIOLI E, PURPURA V, ORLANDI C, et al. The use of an acellular matrix derived from human dermis for the treatment of full-thickness skin wounds. Cell Tissue Bank. 2019;20(2):183-192. [22] 杨维,崔占峰.组织工程皮肤发展现状[J].中国科学:生命科学,2015,45(5): 460-470. [23] 杜烨,冯自波,李恭驰,等.猪脱细胞真皮基质对小鼠创面毛囊再生中基质细胞衍生因子-1及Wnt3a/β-catenin信号通路表达的影响[J].中华损伤与修复杂志(电子版),2019,14(1):26-33. [24] 施恩,刘英芹.组织工程皮肤及其附属器再生修复机制与生物学行为的研究进展[J].中国保健营养,2017,13(27):93-95. [25] HONG JY, SEO Y, DAVAA G, et al. Decellularized Brain Matrix Enhances Macrophage Polarization and Functional Improvements in Rat Spinal Cord Injury. Acta Biomater. 2020;101:357-371. [26] HE C, YANG Z, JIN Y, et al. ADM Scaffolds Generate a Pro-regenerative Microenvironment During Full-Thickness Cutaneous Wound Healing Through M2 Macrophage Polarization via Lamtor1. Front Physiol. 2018;9:657. [27] JIANG K, CHAIMOV D, PATEL SN, et al.3-D physiomimetic extracellular matrix hydrogels provide a supportive microenvironment for rodent and human islet culture. Biomaterials. 2019;198:37-48. [28] ZHAO Y, FAN J, BAI S. Biocompatibility of injectable hydrogel from decellularized human adipose tissue in vitro and in vivo. J Biomed Mater Res B Appl Biomater. 2019;107(5):1684-1694. [29] LEE JS, SHIN J, PARK HM, et al. Liver extracellular matrix providing dual functions of two-dimensional substrate coating and three-dimensional injectable hydrogel platform for liver tissue engineering. Biomacromolecules. 2014;15(1):206. |
| [1] | Liu Huan, Li Han, Ma Yunhao, Zhong Weijian, Ma Guowu. Osteogenic capacity of partially demineralized dentin particles in the maxillary sinus lift [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 354-359. |
| [2] | Li Yue, Lyu Yan, Feng Wanying, Song Yang, Yan Yu, Guan Yongge. Preparation of hyperoside nanoparticles to repair endometrial injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 360-366. |
| [3] | Wu Lihao, Shao Anliang, Xu Lin, Ren Kang, Wang Hongjian, Chen Liang, Xu Ling. Evaluation of immunotoxicity of the absorbable macroporous polysaccharides composite hemostatic material [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 329-334. |
| [4] | Bi Jintong, Hu Xin, Liu Jinshu. Wear properties of dental ceramics [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 406-412. |
| [5] | Jiang Haifang, Liu Rong, Hu Peng, Chen Wei, Wei Zairong, Yang Chenglan, Nie Kaiyu. Application of 3D printing technology in the precise and personalized treatment of cleft lip and palate [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 413-419. |
| [6] | Dai Xianglin, Zhang Wenfeng, Yao Xijun, Shang Jiaqi, Huang Qiujin, Ren Yifan, Deng Jiupeng. Barium titanate/polylactic acid piezoelectric composite film affects adhesion, proliferation, and osteogenic differentiation of MC3T3-E1 cells [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 367-373. |
| [7] | Zhang Haobo, Zhao Yunan, Yang Xuejun. Role and therapeutic implications of pyroptosis in intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1445-1451. |
| [8] | Hou Jingying, Guo Tianzhu, Yu Menglei, Long Huibao, Wu Hao. Hypoxia preconditioning targets and downregulates miR-195 and promotes bone marrow mesenchymal stem cell survival and pro-angiogenic potential by activating MALAT1 [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1005-1011. |
| [9] | Zhou Ying, Zhang Huan, Liao Song, Hu Fanqi, Yi Jing, Liu Yubin, Jin Jide. Immunomodulatory effects of deferoxamine and interferon gamma on human dental pulp stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1012-1019. |
| [10] | Shen Song, Xu Bin. Diffuse distribution of bone cement in percutaneous vertebroplasty reduces the incidence of refracture of adjacent vertebral bodies [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 499-503. |
| [11] | Hou Wanxing, Li Hongwei, Zheng Xin, Zhu Xianren. Correlation between preoperative magnetic resonance imaging findings and bone cement leakage after percutaneous vertebral augmentation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 504-509. |
| [12] | Huang Chuanjun, Zou Yu, Zhou Xiaoting, Zhu Yangqing, Qian Wei, Zhang Wei, Liu Xing. Transplantation of umbilical cord mesenchymal stem cells encapsulated in RADA16-BDNF hydrogel promotes neurological recovery in an intracerebral hemorrhage rat model [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 510-515. |
| [13] | Yang Sidi, Wang Qian, Xu Nuo, Wang Ronghan, Jin Chuanqi, Lu Ying, Dong Ming. Biodentine enhances the proliferation and differentiation of osteoblasts through upregulating bone morphogenetic protein-2 [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 516-520. |
| [14] | Le Guoping, Zhang Ming, Xi Licheng, Luo Hanwen. Preparation and in vitro evaluation of vancomycin hydrochloride@polylactic acid-glycolic acid copolymer-chitosan-hyaluronic acid composite sustained-release microspheres [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 528-534. |
| [15] | Liu Tongbin, Lin Peng, Zhang Xiaoming, Dong Xiling, Cao Fei, Wang Le, Guo Xinxing. Optimization of preparation method of atorvastatin calcium sustained-release microspheres [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 535-539. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||