Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (4): 504-509.doi: 10.12307/2022.083
Previous Articles Next Articles
Correlation between preoperative magnetic resonance imaging findings and bone cement leakage after percutaneous vertebral augmentation
Hou Wanxing, Li Hongwei, Zheng Xin, Zhu Xianren
- Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221006, Jiangsu Province, China
-
Received:2020-08-31Revised:2020-09-04Accepted:2020-10-09Online:2022-02-08Published:2021-11-03 -
Contact:Li Hongwei, Chief physician, Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221006, Jiangsu Province, China -
About author:Hou Wanxing, Master candidate, Physician, Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221006, Jiangsu Province, China
CLC Number:
Cite this article
Hou Wanxing, Li Hongwei, Zheng Xin, Zhu Xianren. Correlation between preoperative magnetic resonance imaging findings and bone cement leakage after percutaneous vertebral augmentation[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 504-509.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

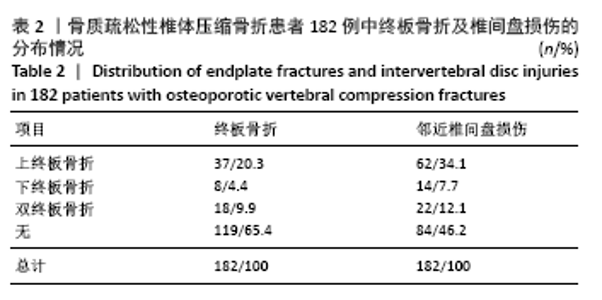
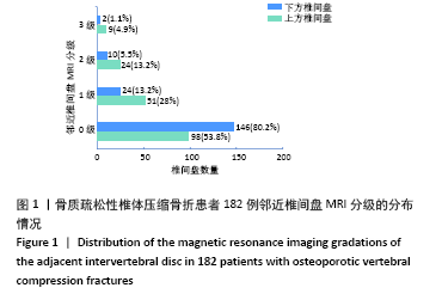
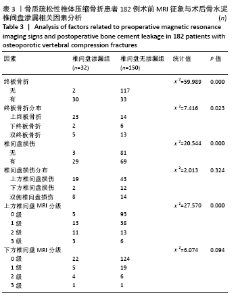
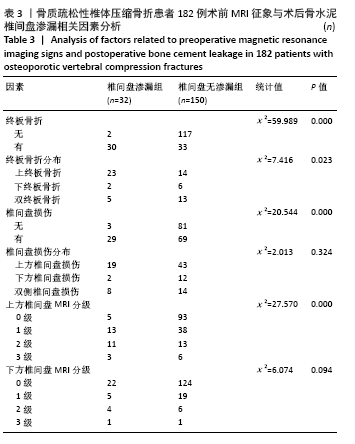
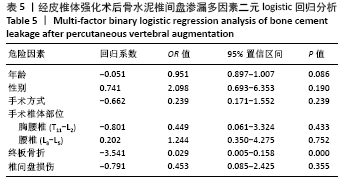
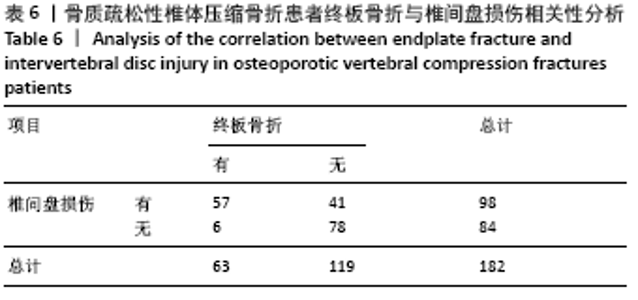
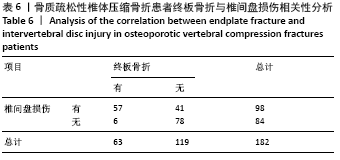
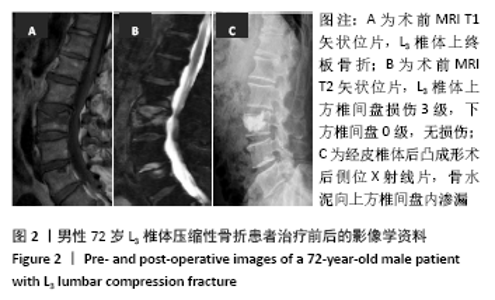
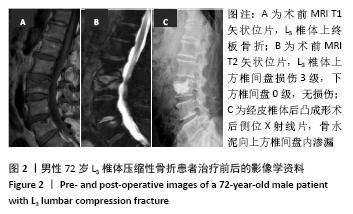
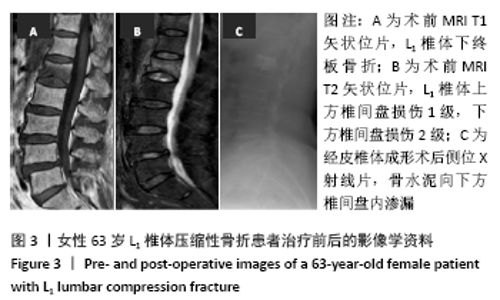
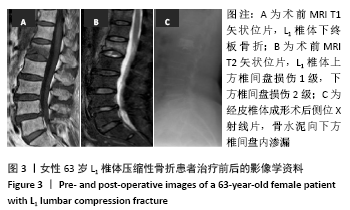
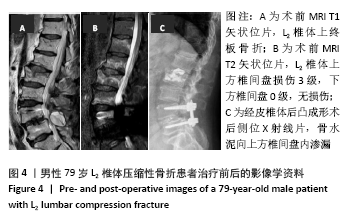
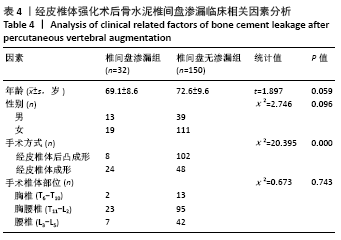
存在终板骨折组的骨水泥椎间盘渗漏发生率(30/63,47.6%)高于无终板骨折组(2/119,1.7%,χ2=59.989,P=0.000);在63例有终板骨折患者的中,终板骨折分布位于上方、下方、双侧在骨水泥椎间盘渗漏发生率比较差异有显著性意义(χ2=7.416,P=0.023),上方终板骨折组的骨水泥椎间盘渗漏率(23/63,37.0%)高于下方终板骨折组(2/63,8.0%)及双侧终板骨折组(5/63,18.0%)。 存在椎间盘损伤组的骨水泥椎间盘渗漏发生率(29/98,29.6%)高于无椎间盘损伤组(3/84,3.6%,χ2=20.544,P=0.000);上方椎间盘MRI各分级中骨水泥渗漏率比较差异有显著性意义(χ2=27.570,P=0.000),损伤程度2级组的骨水泥渗漏率(45.8%)明显高于损伤程度1级组(25.4%)及损伤程度3级组(33.3%);下方椎间盘MRI各分级中骨水泥渗漏率比较差异无显著性意义(χ2=6.074,P=0.094)。 2.4 临床相关因素与骨水泥椎间盘渗漏 骨水泥椎间盘渗漏与年龄、性别、手术椎体部位和手术方式等一般临床资料的单因素分析,见表4。"
| [1] 中华医学会骨科学分会骨质疏松学组.骨质疏松性骨折诊疗指南[J].中华骨科杂志,2017,37(1):1-10. [2] CHEN WJ, KAO YH, YANG SC, et al. Impact of cement leakage into disks on the development of adjacent vertebral compression fractures. J Spinal Disord Tech. 2010;23(1):35-39. [3] 蔡金辉,刘庆余,阮耀钦,等.经皮椎体强化术后骨水泥椎间盘渗漏与邻近椎体骨折的相关性分析[J]. 中国脊柱脊髓杂志,2018,28(8):713-719. [4] 刘军,张陆,刘志昂,等.经皮椎体增强术后邻近椎体再骨折的相关因素[J].中国矫形外科杂志,2020,28(4):319-322. [5] NIEUWENHUIJSE MJ, PUTTER H, VAN ERKEL AR, et al. New vertebral fractures after percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures: a clustered analysis and the relevance of intradiskal cement leakage. Radiology. 2013;266(3):862-870. [6] JAMJOOM B, PATEL S, BOMMIREDDY R, et al. Impact of the quantity of intradiscal cement leak on the progression of intervertebral disc degeneration. Ann R Coll Surg Engl. 2017;99(7):529-533. [7] HONG SJ, LEE S, YOON JS, et al. Analysis of intradiscal cement leakage during percutaneous vertebroplasty: multivariate study of risk factors emphasizing preoperative MR findings. J Neuroradiol. 2014;41(3):195-201. [8] MIROVSKY Y, ANEKSTEIN Y, SHALMON E, et al. Intradiscal cement leak following percutaneous vertebroplasty. Spine (Phila Pa 1976). 2006;31(10): 1120-1124. [9] ZHONG BY, HE SC, ZHU HD, et al. Nomogram for Predicting Intradiscal Cement Leakage Following Percutaneous Vertebroplasty in Patients with Osteoporotic Related Vertebral Compression Fractures. Pain Physician. 2017;20(4):E513-e520. [10] 蔡金辉,刘庆余,曾玉蓉,等. MRI预测经皮椎体强化术骨水泥椎间盘渗漏的价值[J].中国医学影像技术,2017,33(7):1061-1065. [11] ORTIZ AO, BORDIA R. Injury to the vertebral endplate-disk complex associated with osteoporotic vertebral compression fractures. AJNR Am J Neuroradiol. 2011;32(1):115-120. [12] FUJIWARA T, AKEDA K, YAMADA J, et al. Endplate and intervertebral disc injuries in acute and single level osteoporotic vertebral fractures: is there any association with the process of bone healing? BMC Musculoskelet Disord. 2019;20(1):336. [13] GALIBERT P, DERAMOND H, ROSAT P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33(2):166-168. [14] COTTEN A, DEWATRE F, CORTET B, et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996;200(2):525-530. [15] PHAM CT, CLARENçON F, GANEM G, et al. Spinal cervical metastasis from a glioblastoma multiform treated by percutaneous vertebroplasty: a case report. J Neuroradiol. 2011;38(5):323-325. [16] COHEN M, ZEITOUN D, BLANPAIN S, et al. Percutaneous vertebroplasty of the C2 body and dens using the anterior oblique ascending transdiscal approach. J Neuroradiol. 2013;40(3):211-215. [17] CHUROJANA A, SONGSAENG D, KHUMTONG R, et al. Is intervertebral cement leakage a risk factor for new adjacent vertebral collapse? Interv Neuroradiol. 2014;20(5):637-645. [18] LEE KA, HONG SJ, LEE S, et al. Analysis of adjacent fracture after percutaneous vertebroplasty: does intradiscal cement leakage really increase the risk of adjacent vertebral fracture? Skeletal Radiol. 2011; 40(12):1537-1542. [19] SEMAAN H, OBRI T, BAZERBASHI M, et al. Clinical outcome and subsequent sequelae of cement extravasation after percutaneous kyphoplasty and vertebroplasty: a comparative review. Acta Radiol. 2018;59(7):861-868. [20] PITTON MB, HERBER S, BLETZ C, et al. CT-guided vertebroplasty in osteoprotic vertebral fractures: incidence of secondary fractures and impact of intradiscal cement leakages during follow-up. Eur radiol. 2008;18(1): 43-50. [21] SHEN M, NIU J, ZHOU H, et al. Adjacent disc height reduction and clinical outcome after intradiscal cement leakage. Int J Spine Surg. 2016;10(2016): 34. [22] 倪才方,赵辉,陈珑,等.两种骨水泥渗漏对椎间盘影响的实验研究[J].中华骨科杂志,2007,27(4):263-267. [23] HIWATASHI A, OHGIYA Y, KAKIMOTO N, et al. Cement leakage during vertebroplasty can be predicted on preoperative MRI. AJR Am J Roentgenol. 2007;188(4):1089-1093. [24] KOH YH, HAN D, CHA JH, et al. Vertebroplasty: magnetic resonance findings related to cement leakage risk. Acta Radiol. 2007;48(3):315-320. [25] 王立,钟润泉,郭东明,等.应用MRI预判经皮椎体增强术中骨水泥的邻近椎间盘渗漏[J].实用医学杂志,2010,26(13):2358-2361. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [3] | Yu Chengxiang, Liu Lehong, Li Wenbo, Chen Jinshi, Ran Chunlei, Wang Zhongping. Correlation between spine-pelvic sagittal parameters and prognosis of vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1412-1417. |
| [4] | Xue Yadong, Zhou Xinshe, Pei Lijia, Meng Fanyu, Li Jian, Wang Jinzi . Reconstruction of Paprosky III type acetabular defect by autogenous iliac bone block combined with titanium plate: providing a strong initial fixation for the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1424-1428. |
| [5] | Li Wei, Zhu Hanmin, Wang Xin, Gao Xue, Cui Jing, Liu Yuxin, Huang Shuming. Effect of Zuogui Wan on bone morphogenetic protein 2 signaling pathway in ovariectomized osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1173-1179. |
| [6] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [7] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [8] | Wu Bingshuang, Wang Zhi, Tang Yi, Tang Xiaoyu, Li Qi. Anterior cruciate ligament reconstruction: from enthesis to tendon-to-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1293-1298. |
| [9] | Tian Chuan, Zhu Xiangqing, Yang Zailing, Yan Donghai, Li Ye, Wang Yanying, Yang Yukun, He Jie, Lü Guanke, Cai Xuemin, Shu Liping, He Zhixu, Pan Xinghua. Bone marrow mesenchymal stem cells regulate ovarian aging in macaques [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 985-991. |
| [10] | Hu Wei, Xie Xingqi, Tu Guanjun. Exosomes derived from bone marrow mesenchymal stem cells improve the integrity of the blood-spinal cord barrier after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 992-998. |
| [11] | Gao Yujin, Peng Shuanglin, Ma Zhichao, Lu Shi, Cao Huayue, Wang Lang, Xiao Jingang. Osteogenic ability of adipose stem cells in diabetic osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 999-1004. |
| [12] | Hou Jingying, Guo Tianzhu, Yu Menglei, Long Huibao, Wu Hao. Hypoxia preconditioning targets and downregulates miR-195 and promotes bone marrow mesenchymal stem cell survival and pro-angiogenic potential by activating MALAT1 [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1005-1011. |
| [13] | Liang Xuezhen, Yang Xi, Li Jiacheng, Luo Di, Xu Bo, Li Gang. Bushen Huoxue capsule regulates osteogenic and adipogenic differentiation of rat bone marrow mesenchymal stem cells via Hedgehog signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1020-1026. |
| [14] | Cui Xing, Sun Xiaoqi, Zheng Wei, Ma Dexin. Huangqin Decoction regulates autophagy to intervene with intestinal acute graft-versus-host disease in mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1057-1062. |
| [15] | Fang Xiaolei, Leng Jun, Zhang Chen, Liu Huimin, Guo Wen. Systematic evaluation of different therapeutic effects of mesenchymal stem cell transplantation in the treatment of ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1085-1092. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||