[1] SRIVASTAVA RK, SAPRA L, MISHRA PK. Osteometabolism: Metabolic Alterations in Bone Pathologies. Cells. 2022;11(23):3943.
[2] ZHOU M, AN YZ, GUO Q, et al. Energy homeostasis in the bone. Trends Endocrinol Metab. 2024;35(5):439-451.
[3] FU L, ZHANG P, WANG Y, et al. Microbiota-bone axis in ageing-related bone diseases. Front Endocrinol (Lausanne). 2024;15: 1414350.
[4] INCHINGOLO AM, GARGIULO ISACCO C, INCHINGOLO AD, et al. The human microbiota key role in the bone metabolism activity. Eur Rev Med Pharmacol Sci. 2023; 27(6):2659-2670.
[5] BEHERA J, ISON J, TYAGI SC, et al. The role of gut microbiota in bone homeostasis. Bone. 2020;135:115317.
[6] LI C, PI G, LI F. The Role of Intestinal Flora in the Regulation of Bone Homeostasis. Front Cell Infect Microbiol. 2021;11:579323.
[7] NINKOV A, FRANK JR, MAGGIO LA. Bibliometrics: Methods for studying academic publishing. Perspect Med Educ. 2022;11(3):173-176.
[8] HASSAN W, DUARTE AE. Bibliometric analysis: A few suggestions. Curr Probl Cardiol. 2024;49(8):102640.
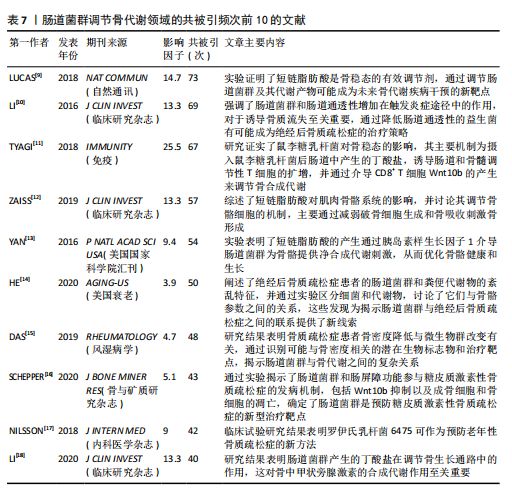
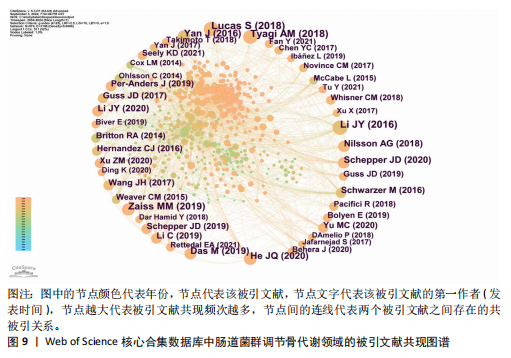
[9] LUCAS S, OMATA Y, HOFMANN J, et al. Short-chain fatty acids regulate systemic bone mass and protect from pathological bone loss. Nat Commun. 2018;9(1):55.
[10] LI JY, CHASSAING B, TYAGI AM, et al. Sex steroid deficiency-associated bone loss is microbiota dependent and prevented by probiotics. J Clin Invest. 2016;126(6):2049-2063.
[11] TYAGI AM, YU M, DARBY TM, et al. The Microbial Metabolite Butyrate Stimulates Bone Formation via T Regulatory Cell-Mediated Regulation of WNT10B Expression. Immunity. 2018;49(6):1116-1131.e7.
[12] ZAISS MM, JONES RM, SCHETT G, et al. The gut-bone axis: how bacterial metabolites bridge the distance. J Clin Invest. 2019; 129(8):3018-3028.
[13] YAN J, HERZOG JW, TSANG K, et al. Gut microbiota induce IGF-1 and promote bone formation and growth. Proc Natl Acad Sci U S A. 2016;113(47):E7554-E7563.
[14] HE J, XU S, ZHANG B, et al. Gut microbiota and metabolite alterations associated with reduced bone mineral density or bone metabolic indexes in postmenopausal osteoporosis. Aging (Albany NY). 2020; 12(9):8583-8604.
[15] DAS M, CRONIN O, KEOHANE DM, et al. Gut microbiota alterations associated with reduced bone mineral density in older adults. Rheumatology (Oxford). 2019; 58(12):2295-2304.
[16] SCHEPPER JD, COLLINS F, RIOS-ARCE ND, et al. Involvement of the Gut Microbiota and Barrier Function in Glucocorticoid-Induced Osteoporosis. J Bone Miner Res. 2020;35(4):801-820.
[17] NILSSON AG, SUNDH D, BÄCKHED F, et al. Lactobacillus reuteri reduces bone loss in older women with low bone mineral density: a randomized, placebo-controlled, double-blind, clinical trial. J Intern Med. 2018;284(3):307-317.
[18] LI JY, YU M, PAL S, et al. Parathyroid hormone-dependent bone formation requires butyrate production by intestinal microbiota. J Clin Invest. 2020;130(4):1767-1781.
[19] D’AMELIO P, SASSI F. Gut Microbiota, Immune System, and Bone. Calcif Tissue Int. 2018;102(4):415-425.
[20] GUO M, LIU H, YU Y, et al. Lactobacillus rhamnosus GG ameliorates osteoporosis in ovariectomized rats by regulating the Th17/Treg balance and gut microbiota structure. Gut Microbes. 2023;15(1):2190304.
[21] ZHOU B, YUAN Y, ZHANG S, et al. Intestinal Flora and Disease Mutually Shape the Regional Immune System in the Intestinal Tract. Front Immunol. 2020;11:575.
[22] ZHANG YW, SONG PR, WANG SC, et al. Diets intervene osteoporosis via gut-bone axis. Gut Microbes. 2024;16(1):2295432.
[23] ADAK A, KHAN MR. An insight into gut microbiota and its functionalities. Cell Mol Life Sci. 2019;76(3):473-493.
[24] WEI H, ZHAO Y, XIANG L. Bone health in inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2023;17(9):921-935.
[25] CUSHING K, HIGGINS PDR. Management of Crohn Disease: A Review. JAMA. 2021; 325(1):69-80.
[26] KE K, ARRA M, ABU-AMER Y. Mechanisms Underlying Bone Loss Associated with Gut Inflammation. Int J Mol Sci. 2019;20(24): 6323.
[27] AL-DAGHRI NM, AZIZ I, YAKOUT S, et al. Inflammation as a contributing factor among postmenopausal Saudi women with osteoporosis. Medicine (Baltimore). 2017;96(4):e5780.
[28] MONTALVANY-ANTONUCCI CC, DUFFLES LF, DE ARRUDA JAA, et al. Short-chain fatty acids and FFAR2 as suppressors of bone resorption. Bone. 2019;125:112-121.
[29] WALLIMANN A, MAGRATH W, THOMPSON K, et al. Gut microbial-derived short-chain fatty acids and bone: a potential role in fracture healing. Eur Cell Mater. 2021;41:454-470.
[30] BAO M, ZHANG K, WEI Y, et al. Therapeutic potentials and modulatory mechanisms of fatty acids in bone. Cell Prolif. 2020;53(2): e12735.
[31] LIU X, ZHANG H, SHI G, et al. The impact of gut microbial signals on hematopoietic stem cells and the bone marrow microenvironment. Front Immunol. 2024; 15:1338178.
[32] LORENZO J. From the gut to bone: connecting the gut microbiota with Th17 T lymphocytes and postmenopausal osteoporosis. J Clin Invest. 2021;131(5): e146619.
[33] XU Q, LI D, CHEN J, et al. Crosstalk between the gut microbiota and postmenopausal osteoporosis: Mechanisms and applications. Int Immunopharmacol. 2022;110:108998.
[34] GUAN Z, XUANQI Z, ZHU J, et al. Estrogen deficiency induces bone loss through the gut microbiota. Pharmacol Res. 2023;196: 106930.
[35] FENG R, WANG Q, YU T, et al. Quercetin ameliorates bone loss in OVX rats by modulating the intestinal flora-SCFAs-inflammatory signaling axis. Int Immunopharmacol. 2024;136:112341.
[36] ZHANG YW, CAO MM, LI YJ, et al. Fecal microbiota transplantation ameliorates bone loss in mice with ovariectomy-induced osteoporosis via modulating gut microbiota and metabolic function. J Orthop Translat. 2022;37:46-60.
[37] ZHAO T, WEI Y, ZHU Y, et al. Gut microbiota and rheumatoid arthritis: From pathogenesis to novel therapeutic opportunities. Front Immunol. 2022;13: 1007165.
[38] LIN L, ZHANG K, XIONG Q, et al. Gut microbiota in pre-clinical rheumatoid arthritis: From pathogenesis to preventing progression. J Autoimmun. 2023;141:103001.
[39] CAMPBELL C, KANDALGAONKAR MR, GOLONKA RM, et al. Crosstalk between Gut Microbiota and Host Immunity: Impact on Inflammation and Immunotherapy. Biomedicines. 2023;11(2):294.
[40] LI J, JIA N, CUI M, et al. The intestinal mucosal barrier - A key player in rheumatoid arthritis? Clin Anat. 2023;36(7):977-985.
[41] KIMBALL JS, JOHNSON JP, CARLSON DA. Oxidative Stress and Osteoporosis. J Bone Joint Surg Am. 2021;103(15):1451-1461.
[42] RIEGGER J, SCHOPPA A, RUTHS L, et al. Oxidative stress as a key modulator of cell fate decision in osteoarthritis and osteoporosis: a narrative review. Cell Mol Biol Lett. 2023;28(1):76.
[43] SHANDILYA S, KUMAR S, KUMAR JHA N, et al. Interplay of gut microbiota and oxidative stress: Perspective on neurodegeneration and neuroprotection. J Adv Res. 2021;38: 223-244.
[44] ZONG Y, LI H, LIAO P, et al. Mitochondrial dysfunction: mechanisms and advances in therapy. Signal Transduct Target Ther. 2024;9(1):124.
[45] KOWALCZYK P, SULEJCZAK D, KLECZKOWSKA P, et al. Mitochondrial Oxidative Stress-A Causative Factor and Therapeutic Target in Many Diseases. Int J Mol Sci. 2021; 22(24):13384.
[46] SUN K, JING X, GUO J, et al. Mitophagy in degenerative joint diseases. Autophagy. 2021;17(9):2082-2092.
[47] AILIOAIE LM, AILIOAIE C, LITSCHER G. Gut Microbiota and Mitochondria: Health and Pathophysiological Aspects of Long COVID. Int J Mol Sci. 2023;24(24):17198. |