1] LEE S, ZHENG H, PARK SM, et al. A Randomized Controlled Trial of Vertebral Body Decompression Procedure Versus Conservative Treatment for Painful Vertebral Compression Fracture. Medicina (Kaunas). 2023;59(10):1848.
[2] JANG HD, KIM EH, LEE JC, et al. Management of Osteoporotic Vertebral Fracture: Review Update 2022. Asian Spine J. 2022;16(6):934-946.
[3] SONG T, SUN F, LIU S, et al. Percutaneous lordoplasty for the treatment of severe osteoporotic vertebral compression fractures with kyphosis. Front Neurol. 2023;14:1132919.
[4] OKUWAKI S, FUNAYAMA T, IKUMI A, et al. Risk factors affecting vertebral collapse and kyphotic progression in postmenopausal osteoporotic vertebral fractures. J Bone Miner Metab. 2022;40(2):301-307.
[5] WANG X, ZHU YH, ZHU QS. Efficacy and safety of robot-assisted versus fluoroscopy-assisted PKP or PVP for osteoporotic vertebral compression fractures: a systematic review and meta-analysis. J Robot Surg. 2023; 17(6):2597-2610.
[6] PATEL N, JACOBS D, JOHN J, et al. Balloon Kyphoplasty vs Vertebroplasty: A Systematic Review of Height Restoration in Osteoporotic Vertebral Compression Fractures. J Pain Res. 2022;15:1233-1245.
[7] OSTERHOFF G, RAPPERT D, SCHEYERER MJ, et al. [Value of routine transpedicular biopsies in kyphoplasty and vertebroplasty for vertebral compression fractures : A survey among 250 spine surgeons]. Unfallchirurgie (Heidelb). Unfallchirurgie (Heidelb). 2023;126(11): 873-879.
[8] 张志伟,李利,黄兹谕,等.单、双侧椎弓根入路及单侧椎弓根外入路椎体成形治疗胸腰段椎体压缩性骨折:骨水泥灌注量与渗漏率[J].中国组织工程研究,2020,24(9):1353-1358.
[9] 顾晨希,虞宵,黄安全,等.单侧椎体后外上方入路与双侧椎弓根入路行椎体成型术治疗骨质疏松性椎体压缩骨折的生物力学对比研究[J].生物骨科材料与临床研究,2022,19(5):16-20+26.
[10] ZHU D, HU JN, WANG L, et al. A Modified Unilateral Extrapedicular Approach Applied to Percutaneous Kyphoplasty to Treat Lumbar Osteoporotic Vertebral Compression Fracture: A Retrospective Analysis. Pain Physician. 2023;26(3):E191-E201.
[11] ZHANG T, DENG Y. A design of a targeted puncture trajectory applied to unilateral extrapedicular percutaneous vertebroplasty. BMC Musculoskelet Disord. 2023;24(1):268.
[12] HONG H, LI J, DING H, et al. Unilaterally extrapedicular versus transpedicular kyphoplasty in treating osteoporotic lumbar fractures: a randomized controlled study. J Orthop Surg Res. 2023;18(1):801.
[13] 中国康复医学会骨质疏松预防与康复专业委员会.骨质疏松性椎体压缩骨折诊治专家共识(2021版)[J]. 中华医学杂志,2021,101(41): 3371-3379.
[14] 中华医学会骨质疏松和骨矿盐疾病分会.骨代谢生化标志物临床应用指南[J].中华骨质疏松和骨矿盐疾病杂志,2015,8(4):283-293.
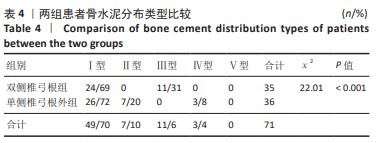
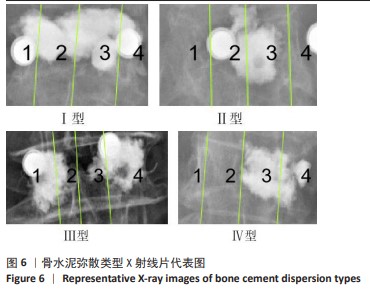
[15] 张大鹏,毛克亚,强晓军,等.椎体增强术后骨水泥分布形态分型及其临床意义[J].中华创伤杂志,2018,34(2):130-137.
[16] GU Y, HAO K, BAI J, et al. Effect of vertebroplasty with bone cement on osteoporotic compression fractures in elderly patients. Am J Transl Res. 2023;15(9):5921-5929.
[17] SUN Y, ZHANG Y, MA H, et al. Therapeutic Efficacy and Safety of Percutaneous Curved Vertebroplasty in Osteoporotic Vertebral Compression Fractures: A Systematic Review and Meta-Analysis. Orthop Surg. 2023;15(10):2492-2504.
[18] SUNG HS, KIM SI, PARK HY, et al. Predictive factors for conversion from conservatively to surgically treatment osteoporotic thoracolumbar compression fractures based on sagittal parameters and magnetic resonance imaging features. Eur Spine J. 2023;32(11):3933-3940.
[19] DAI C, LIANG G, ZHANG Y, et al. Risk factors of vertebral re-fracture after PVP or PKP for osteoporotic vertebral compression fractures, especially in Eastern Asia: a systematic review and meta-analysis. J Orthop Surg Res. 2022;17(1):161.
[20] SUN X, DENG M, XU W, et al. CT features and risk factors of pulmonary cement embolism after vertebroplasty or kyphoplasty in patients with vertebral compression fracture: a retrospective cohort study. Quant Imaging Med Surg. 2023;13(4):2397-2407.
[21] WANG R, XU Y, MA X. Risk factors and strategies for recovery quality, postoperative pain, and recurrent fractures between percutaneous kyphoplasty and percutaneous vertebroplasty in elderly patients with thoracolumbar compression fractures: a retrospective comparative cohort study. Ann Transl Med. 2023;11(2):122.
[22] WANG H, SRIBASTAV SS, YE F, et al. Comparison of Percutaneous Vertebroplasty and Balloon Kyphoplasty for the Treatment of Single Level Vertebral Compression Fractures: A Meta-analysis of the Literature. Pain Physician. 2015;18(3):209-222.
[23] WEI H, DONG C, ZHU Y, et al. Analysis of two minimally invasive procedures for osteoporotic vertebral compression fractures with intravertebral cleft: a systematic review and meta-analysis. J Orthop Surg Res. 2020;15(1):401.
[24] HOH BL, RABINOV JD, PRYOR JC, et al. Balloon kyphoplasty for vertebral compression fracture using a unilateral balloon tamp via a uni-pedicular approach: technical note. Pain Physician. 2004;7(1):111-114.
[25] LI T, PANG S, ENGLAND R, et al. Clinical Outcomes and Safety Comparison of Vertebroplasty, Balloon Kyphoplasty, and Vertebral Implant for Treatment of Vertebral Compression Fractures. AJNR Am J Neuroradiol. 2023;44(11):1345-1351.
[26] PATEL A, PETRONE B, CARTER KR. Percutaneous Vertebroplasty and Kyphoplasty. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2023.
[27] 谢杨,李长军,肖勇.多节段脊柱骨折的手术策略[J].中国医学工程,2015,23(5):118-119.
[28] 杨勇.经皮椎体成形术治疗跳跃性多节段脊柱骨折的手术效果评价[J].中国现代药物应用,2021,15(4):55-57.
[29] LIS E, LAUFER I, BARZILAI O, et al. Change in the cross-sectional area of the thecal sac following balloon kyphoplasty for pathological vertebral compression fractures prior to spine stereotactic radiosurgery. J Neurosurg Spine. 2018;30(1):111-118.
[30] ALPANTAKI K, DOHM M, KOROVESSIS P, et al. Surgical options for osteoporotic vertebral compression fractures complicated with spinal deformity and neurologic deficit. Injury. 2018;49(2):261-271.
[31] ZHU J, ZHANG K, LUO K, et al. Mineralized Collagen Modified Polymethyl Methacrylate Bone Cement for Osteoporotic Compression Vertebral Fracture at 1-Year Follow-up. Spine (Phila Pa 1976). 2019; 44(12):827-838.
[32] BEALL DP, PARSONS B, BURNER S. Technical Strategies and Anatomic Considerations for an Extrapedicular Modified Inferior Endplate Access to Thoracic and Lumbar Vertebral Bodies. Pain Physician. 2016; 19(8):593-601.
[33] 李玉伟,王海蛟,崔巍,等.极外侧穿刺法行经皮椎体成形术治疗骨质疏松性椎体压缩骨折[J].中国修复重建外科杂志,2019,33(5): 612-617.
[34] ZHUO Y, LIU L, WANG H, et al. A Modified Transverse Process-Pedicle Approach Applied to Unilateral Extrapedicular Percutaneous Vertebroplasty. Pain Res Manag. 2021;2021:6493712.
[35] CHEVALIER Y, PAHR D, CHARLEBOIS M, et al. Cement distribution, volume, and compliance in vertebroplasty: some answers from an anatomy-based nonlinear finite element study. Spine (Phila Pa 1976). 2008;33(16):1722-1730.
[36] HE X, HU W, ZHANG Y, et al. Cellular senescence in skeletal disease: mechanisms and treatment. Cell Mol Biol Lett. 2023;28(1):88.
[37] MA S, QIN J, HAO Y, et al. Association of gut microbiota composition and function with an aged rat model of senile osteoporosis using 16S rRNA and metagenomic sequencing analysis. Aging (Albany NY). 2020;12(11):10795-10808. |