[1] SCHMITZ JP, HOLLINGER JO. The critical size defect as an experimental model for craniomandibulofacial nonunions. Clin Orthop Relat Res. 1986;(205):299-308.
[2] HAUGEN HJ, LYNGSTADAAS SP, ROSSI F, et al. Bone grafts: which is the ideal biomaterial? J Clin Periodontol. 2019;46 Suppl 21:92-102.
[3] FERNANDEZ DE GRADO G, KELLER L, IDOUX-GILLET Y, et al. Bone substitutes: a review of their characteristics, clinical use, and perspectives for large bone defects management. J Tissue Eng. 2018; 9:2041731418776819.
[4] SZCZEŚ A, HOŁYSZ L, CHIBOWSKI E. Synthesis of hydroxyapatite for biomedical applications. Adv Colloid Interface Sci. 2017;249:321-330.
[5] 高飞,闫明,朱珊珊,等.羟基磷灰石在生物材料中的应用[J].现代口腔医学杂志,2019,33(5):310-313.
[6] KUNISADA T, HASEI J, FUJIWARA T, et al. Radiographic and clinical assessment of unidirectional porous hydroxyapatite to treat benign bone tumors. Sci Rep. 2020;10(1):21578.
[7] LINH NTB, ABUEVA CDG, JANG DW, et al. Collagen and bone morphogenetic protein-2 functionalized hydroxyapatite scaffolds induce osteogenic differentiation in human adipose-derived stem cells. J Biomed Mater Res B Appl Biomater. 2020;108(4):1363-1371.
[8] YANG L, ULLAH I, YU K, et al. Bioactive Sr2+/Fe3+co-substituted hydroxyapatite in cryogenically 3D printed porous scaffolds for bone tissue engineering. Biofabrication. 2021;13(3) doi: 10.1088/1758-5090/abcf8d.
[9] LI J, XU T, WANG Q, et al. Integrating surface topography of stripe pattern on pore surface of 3-dimensional hydroxyapatiye scaffolds. Mater Lett. 2016;169:148-152.
[10] LI J, ZH W, XU T, et al. Ectopic osteogenesis and angiogenesis regulated by porous architecture of hydroxyapatite scaffolds with similar interconnecting structure in vivo. Regen Biomater. 2016;3(5):285-297.
[11] REN X, TUO Q, TIAN K, et al. Enhancement of osteogenesis using a novel porous hydroxyapatite scaffold in vivo and vitro. Ceram Int. 2018; 44(17):21656-21665.
[12] LI C, YANG L, REN X, et al. Grooved hydroxyapatite scaffold modulates mitochondria homeostasis and thus promotes osteogenesis in bone mesenchymal stromal cells. Mol Med Rep. 2020;22(4):2801-2809.
[13] LI C, YANG L, REN X, et al. Groove structure of porous hydroxyapatite scaffolds (HAS) modulates immune environment via regulating macrophages and subsequently enhances osteogenesis. J Biol Inorg Chem. 2019;24(5):733-745.
[14] ATTIA MS, MOHAMMED HM, ATTIA MG, et al. Histological and histomorphometric evaluation of hydroxyapatite-based biomaterials in surgically created defects around implants in dogs. J Periodontol. 2019;90(3):281-287.
[15] MYEROFF C, ARCHDEACON M. Autogenous bone graft: donor sites and techniques. J Bone Joint Surg Am. 2011;93(23):2227-2236.
[16] TASDEMIR U, IYILIKÇI B, AKTÜRK MC, et al. The Effect of Autogenous Bone Graft Mixed With Recombinant Human Vascular Endothelial Growth Factor on Bone Regeneration. J Craniofac Surg. 2021;32(6):2233-2237.
[17] IIJIMA K, OTSUKA H. Cell Scaffolds for Bone Tissue Engineering. Bioengineering (Basel). 2020;7(4):119.
[18] KUBOKI Y, JIN Q, TAKITA H. Geometry of carriers controlling phenotypic expression in BMP-induced osteogenesis and chondrogenesis. J Bone Joint Surg Am. 2001;83-A Suppl 1(Pt 2):S105-S115.
[19] HAN X, SUN M, CHEN B, et al. Lotus seedpod-inspired internal vascularized 3D printed scaffold for bone tissue repair. Bioact Mater. 2020;6(6):1639-1652.
[20] JIN QM, TAKITA H, KOHGO T, et al. Effects of geometry of hydroxyapatite as a cell substratum in BMP-induced ectopic bone formation. J Biomed Mater Res. 2000;51(3):491-499.
[21] MAREW T, BIRHANU G. Three dimensional printed nanostructure biomaterials for bone tissue engineering. Regen Ther. 2021;18:102-111.
[22] MURPHY CM, HAUGH MG. The effect of mean pore size on cell attachment, proliferation and migration in collagen-glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials. 2010;31(3):461-466.
[23] 魏莉,马保金,邵金龙,等.羟基磷灰石复合材料在骨组织工程中应用的研究进展[J].四川大学学报(医学版),2021,52(3):357-363.
[24] 李杜晨晖,田艾,唐正龙.骨生物支架材料诱导的血管生成[J].中国组织工程研究,2022,26(22):3602-3608.
[25] HE J, CHEN G, LIU M, et al. Scaffold strategies for modulating immune microenvironment during bone regeneration. Mater Sci Eng C Mater Biol Appl. 2020;108:110411.
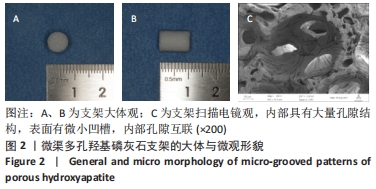
[26] 吕欣荣,温永梅,伍佳,等.微渠表面多孔羟基磷灰石支架体内异位成骨性的研究[J].实用医院临床杂志,2017,14(3):28-31.
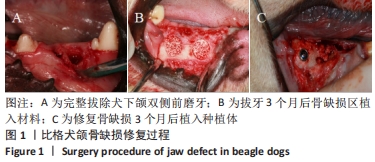
[27] 陈胡贵,覃建国,李理,等.大动物节段性骨缺损模型的研究进展[J].北京生物医学工程,2021,40(2):203-208.
[28] DRAENERT M, DRAENERT A, DRAENERT K. Osseointegration of hydroxyapatite and remodeling-resorption of tricalciumphosphate ceramics. Microsc Res Tech. 2013;76(4):370-380.
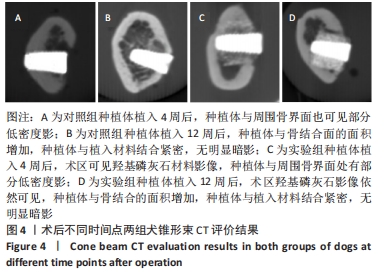
[29] TSAI MT, HE RT, HUANG HL, et al. Effect of Scanning Resolution on the Prediction of Trabecular Bone Microarchitectures Using Dental Cone Beam Computed Tomography. Diagnostics (Basel). 2020;10(6):368.
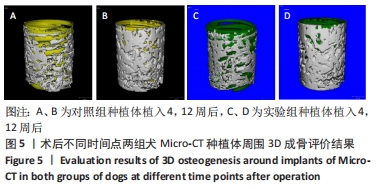
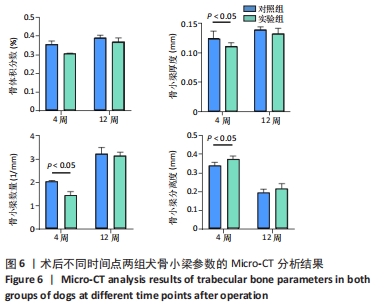
[30] HUANG Y, LI Z, VAN DESSEL J, et al. Effect of platelet-rich plasma on peri-implant trabecular bone volume and architecture: A preclinical micro-CT study in beagle dogs. Clin Oral Implants Res. 2019;30(12):1190-1199.
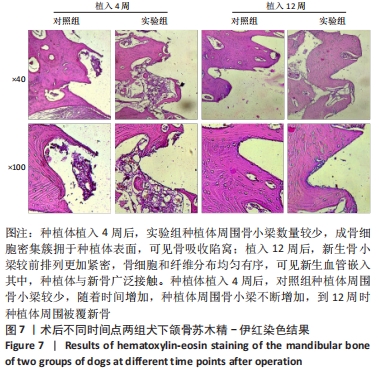
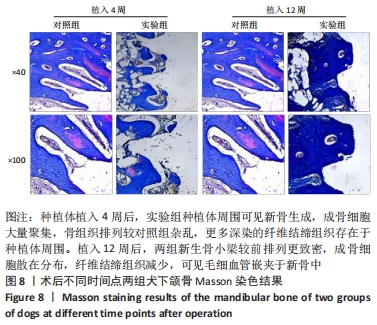
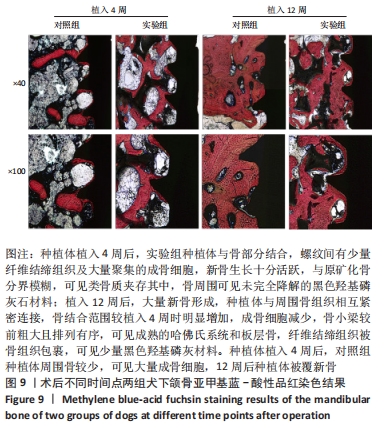
[31] 朱福余,袁暾,张杰,等.含植入物不脱钙骨组织病理切片技术在骨组织形态学研究中的应用[J].医疗装备,2020,33(19):30-34.
[32] INSUA A, MONJE A, WANG HL, et al. Basis of bone metabolism around dental implants during osseointegration and peri-implant bone loss. J Biomed Mater Res A. 2017;105(7):2075-2089.
[33] CHÁVARRI-PRADO D, BRIZUELA-VELASCO A, DIÉGUEZ-PEREIRA M, et al. Influence of cortical bone and implant design in the primary stability of dental implants measured by two different devices of resonance frequency analysis: An in vitro study. J Clin Exp Dent. 2020; 12(3):e242-e248.
[34] HÉRIVEAUX Y, VAYRON R, FRAULOB M, et al. Assessment of dental implant stability using resonance frequency analysis and quantitative ultrasound methods. J Prosthodont Res. 2021;65(3):421-427.
[35] SIM CP, LANG NP. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: I. Instrument positioning, bone structure, implant length. Clin Oral Implants Res. 2010;21(6):598-604.
[36] DAVIES JE. Mechanisms of endosseous integration. Int J Prosthodont. 1998;11(5):391-401.
|