[1] 中华医学会运动医疗分会下肢运动创伤学组,中国医师协会运动医学医师分会.前十字韧带全内重建技术中国专家共识(2023年版)[J].中华骨科杂志,2023, 43(24):1631-1640.
[2] CAI Z, LIU D, YANG Y, et al. Outcomes from different aspects indicate the all-inside technique may serve as an ideal option for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2024; 32(11):2746-2754.
[3] AN BJ, WANG YT, ZHAO Z, et al. Comparative study of the clinical efficacy of all-inside and traditional techniques in anterior cruciate ligament reconstruction. World J Clin Cases. 2023;11(14):3195-3203.
[4] TANG H, XIAO YF, WU YM, et al. Physeal-Sparing, All-Inside Anterior Cruciate Ligament Reconstruction Using Quadrupled Semitendinosus Autograft and Suture Tape Augmentation for Skeletally Immature Patients. Arthrosc Tech. 2024;13(3):102889.
[5] LI X, CAO W, ZHOU H, et al. The healing effect of the all inside technique is superior to the traditional technique in the reconstruction of the anterior cruciate ligament. Eur J Transl Myol. 2024;34(1): 11970.
[6] XU J, JIA Y, ZHANG B, et al. Comparison of the Clinical Outcomes between All-inside and Standard Technique in Anterior Cruciate Ligament Reconstruction with 6-strand Hamstring Tendon Autograft. Orthop Surg. 2024;16(5):1034-1041.
[7] LIN R, ZHONG Q, WU X, et al. Randomized controlled trial of all-inside and standard single-bundle anterior cruciate ligament reconstruction with functional, MRI-based graft maturity and patient-reported outcome measures. BMC Musculoskelet Disord. 2022;23(1):289.
[8] 冯建豪,徐一宏,徐卫东.全内技术与全胫骨隧道技术重建前十字韧带的临床疗效meta分析[J].中华骨科杂志,2023, 43(16):1104-1114.
[9] VARGHESE P, PATRA SK, DAS G, et al. Comparison of the Functional Outcomes of Arthroscopic Anterior Cruciate Ligament Reconstruction through the All-inside and Outside-in Techniques: A Double-Blinded Randomized Controlled Trial. Rev Bras Ortop (Sao Paulo). 2024;59(3):e385-e392.
[10] MO IF, HARLEM T, FALEIDE AGH, et al. ACL Reconstruction Using Quadrupled Semitendinosus Versus Double-Stranded Semitendinosus and Gracilis Autograft: 2-Year Results From a Prospective Randomized Controlled Study. Am J Sports Med. 2024;52(8):1927-1936.
[11] 徐一宏,冯建豪,宋廷轩,等.腓骨长肌全内重建前交叉韧带与腘绳肌重建的对比[J].中华关节外科杂志(电子版),2024, 18(2):175-185.
[12] EICHINGER M, PLONER M, DEGENHART G, et al. Tunnel widening after ACL reconstruction with different fixation techniques: aperture fixation with biodegradable interference screws versus all-inside technique with suspensory cortical buttons. 5-year data from a prospective randomized trial. Arch Orthop Trauma Surg. 2023;143(11):6707-6718.
[13] RAI P, PURI S, GUPTA LM, et al. Comparative study of functional outcomes of arthroscopic anterior cruciate ligament reconstruction using anteromedial portal and translateral all-inside technique. Med J Armed Forces India. 2023;79(Suppl 1): S181-S188.
[14] KULSHRESTHA V, SOOD M, KUMAR S, et al. Original study: early patient-reported functional outcome of all-inside ACL reconstruction as compared to anteromedial portal technique. Eur J Orthop Surg Traumatol. 2021;31(7):1477-1483.
[15] SMITH PA, COOK CS, BLEY JA. All-Inside Quadrupled Semitendinosus Autograft Shows Stability Equivalent to Patellar Tendon Autograft Anterior Cruciate Ligament Reconstruction: Randomized Controlled Trial in Athletes 24 Years or Younger. Arthroscopy. 2020;36(6): 1629-1646.
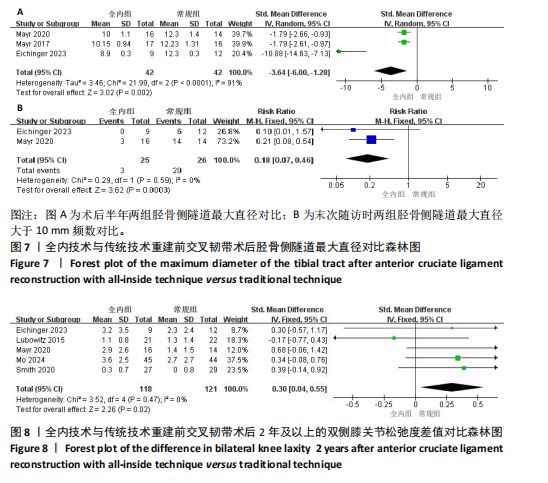
[16] MAYR R, SMEKAL V, KOIDL C, et al. ACL reconstruction with adjustable-length loop cortical button fixation results in less tibial tunnel widening compared with interference screw fixation. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1036-1044.
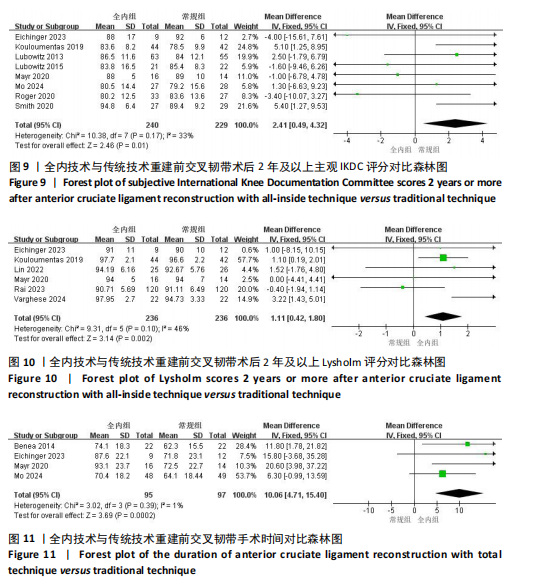
[17] ROGER J, BERTANI A, VIGOUROUX F, et al. ACL reconstruction using a quadruple semitendinosus graft with cortical fixations gives suitable isokinetic and clinical outcomes after 2 years. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2468-2477.
[18] KOULOUMENTAS P, KAVROUDAKIS E, CHARALAMPIDIS E, et al. Superior knee flexor strength at 2 years with all-inside short-graft anterior cruciate ligament reconstruction vs a conventional hamstring technique. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3592-3598.
[19] BALDASSARRI M, PERAZZO L, GHINELLI D, et al. Return to Sport after ACL Surgery: A Comparison between Two Different Reconstructive Techniques. J Knee Surg. 2019;32(6):513-518.
[20] RUSSU OM, CIORCILA E, FEIER AM, et al. Early Outcomes in Anterior Cruciate Ligament Reconstruction: Full Tibial tunnel technique compared to all-inside technique. Revista de Chimie. 2019;69(12):3753-3755.
[21] MAYR R, SMEKAL V, KOIDL C, et al. Tunnel widening after ACL reconstruction with aperture screw fixation or all-inside reconstruction with suspensory cortical button fixation: Volumetric measurements on CT and MRI scans. Knee. 2017;24(5):1047-1054.
[22] LUBOWITZ JH, SCHWARTZBERG R, SMITH P. Cortical Suspensory Button Versus Aperture Interference Screw Fixation for Knee Anterior Cruciate Ligament Soft-Tissue Allograft: A Prospective, Randomized Controlled Trial. Arthroscopy. 2015;31(9):1733-1739.
[23] BENEA H, D’ASTORG H, KLOUCHE S, et al. Pain evaluation after all-inside anterior cruciate ligament reconstruction and short term functional results of a prospective randomized study. Knee. 2014;21(1):102-106.
[24] LUBOWITZ JH, SCHWARTZBERG R, SMITH P. Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy. 2013;29(7): 1195-1200.
[25] GERFROIT A, MARTY-DILOY T, LABOUDIE P, et al. Correlation between Anterior Cruciate Ligament-Return to Sport after Injury Score at 6 Months after Anterior Cruciate Ligament Reconstruction and Mid-Term Functional Test Results: An Observational Study at 5-Year Follow-Up. J Clin Med. 2024; 13(15):4498.
[26] ASHFAQUE MU, ASIF N, KHAN MJ, et al. Radiological study of bone tunnel widening following ACL reconstruction and its effect on clinical outcome: A retrospective study. J Orthop Rep. 2025;4(3):100510.
[27] 李翼,杨文博,孟春庆,等.全内技术在前交叉韧带重建中的应用进展[J].生物骨科材料与临床研究,2024,21(4):82-86.
[28] LIN TY, CHUNG CC, CHEN WC, et al. Complications following all-inside anterior cruciate ligament reconstruction. Int Orthop. 2022;46(11):2569-2576.
[29] MAHIROGULLARI M, KEHRIBAR L, SURUCU S, et al. Comparative Results of Anterior Cruciate Ligament Reconstruction with Full Tibial Tunnel: Quadrupled Semitendinosus Suspensory Femoral and Tibial Fixation versus Quadrupled Semitendinosus and Gracilis Suspensory Femoral and Tibial Screw and Staple Fixation. J Knee Surg. 2023;36(10):1069-1076.
[30] SCHÜTZENBERGER S, KELLER F, GRABNER S, et al. ACL reconstruction with femoral and tibial adjustable versus fixed-loop suspensory fixation: a retrospective cohort study. J Orthop Surg Res. 2022;17(1):244.
[31] XIANG S, AO Z, REN Z, et al. Comparison of a full tibial tunnel or an all-inside technique for anterior cruciate ligament reconstruction: An observational study. Medicine (Baltimore). 2024;103(42):e40135.
[32] LV X, WANG M, ZHAO T, et al. All-inside versus complete tibial tunnel techniques in anterior cruciate ligament reconstruction: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2023;18(1):127.
[33] MARISCALCO MW, FLANIGAN DC, MITCHELL J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29(12):1948-1953.
[34] RAHARDJA R, ZHU M, LOVE H, et al. Factors associated with revision following anterior cruciate ligament reconstruction: A systematic review of registry data. Knee. 2020;27(2):287-299.
[35] SNAEBJÖRNSSON T, HAMRIN-SENORSKI E, SVANTESSON E, et al. Graft Diameter and Graft Type as Predictors of Anterior Cruciate Ligament Revision: A Cohort Study Including 18,425 Patients from the Swedish and Norwegian National Knee Ligament Registries. J Bone Joint Surg Am. 2019;101(20):1812-1820.
[36] JAGADEESH N, DHAWAN T, SHEIK F, et al. Does Hamstring Graft Size Affect Functional Outcome and Incidence of Revision Surgery After Primary Anterior Cruciate Ligament (ACL) Reconstruction? Cureus. 2022;14(1):e21158.
[37] SARAKATSIANOS V, CRISTIANI R, FORSSBLAD M, et al. Patient’s Height and Sex Predict Graft Diameter: A Cohort Study of 4,519 Patients With Primary Anterior Cruciate Ligament Reconstruction Using Semitendinosus Autograft. Arthroscopy. 2024;40(10):2588-2591.
[38] LIN TJ. Editorial Commentary: Quadrupled Semitendinosus Autograft Is a Suitable Graft Choice for Anterior Cruciate Reconstruction, Regardless of Diameter, in Patients With Lower Risk for Rerupture. Arthroscopy. 2024. doi: 10.1016/j.arthro.2024.09.031.
[39] DESAI VS, ANDERSON GR, WU IT, et al. Anterior Cruciate Ligament Reconstruction With Hamstring Autograft: A Matched Cohort Comparison of the All-Inside and Complete Tibial Tunnel Techniques. Orthop J Sports Med. 2019;7(1):2325967118820297.
[40] GOYAL T, DAS L, PAUL S, et al. Outcomes of retro-drilled all-inside tibial tunnel vs complete tibial tunnel techniques in anterior cruciate ligament reconstruction-a comparative study. Eur J Orthop Surg Traumatol. 2022;32(3):523-532.
[41] YANG W, HUANG Z, SHAO Z, et al. A Modified Technique for All-Inside Anterior Cruciate Ligament Reconstruction (ACLR): True Femoral Socket. Arthrosc Tech. 2023; 12(11):e2049-e2058.
[42] MONACO E, FABBRI M, REDLER A, et al. Anterior cruciate ligament reconstruction is associated with greater tibial tunnel widening when using a bioabsorbable screw compared to an all-inside technique with suspensory fixation. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2577-2584.
[43] SANDERS TL, PAREEK A, HEWETT TE, et al. Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):222-228.
[44] MIN JH, YOON HK, OH HC, et al. Graft choice to decrease the revision rate of anterior cruciate ligament reconstruction: a nationwide retrospective cohort study. Sci Rep. 2024;14(1):20004.
[45] ZHU S, LI R. All-Inside Anterior Cruciate Ligament Reconstruction Had Clinical Outcome Similar to the Transtibial Technique Except for Improved Side-to-Side Difference and Tegner Activity Scale: A Systematic Review and Meta-analysis. Arthroscopy. 2024;40(8):2276-2288.
[46] BRESSY G, BRUN V, FERRIER A, et al. Lack of stability at more than 12 months of follow-up after anterior cruciate ligament reconstruction using all-inside quadruple-stranded semitendinosus graft with adjustable cortical button fixation in both femoral and tibial sides. Orthop Traumatol Surg Res. 2016;102(7):867-872.
|