[1] CONFAVREUX CB. Bone: from a reservoir of minerals to a regulator of energy metabolism. Kidney Int. 2011;79121:S14-19.
[2] FUKUMOTO S, MARTIN TJ. Bone as an endocrine organ. Trends Endocrinol Metab. 2009;20(5):230-236.
[3] GUNTUR AR, ROSEN CJ. Bone as an endocrine organ. Endocr Pract. 2012;18(5):758-762.
[4] SINGER M, DEUTSCHMAN CS, SEYMOUR CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-810.
[5] CECCONI M, EVANS L, LEVY M, et al. Sepsis and septic shock. Lancet. 2018;392(10141):75-87.
[6] LEE P, NAIR P, EISMAN JA, et al. Bone Failure in Critical Illness. Review Crit Care Med. 2016;44(12):2270-2274.
[7] BLIUC D, TRAN T, VAN GEEL T, et al. Mortality risk reduction differs according to bisphosphonate class: a 15-year observational study. Osteoporos Int. 2019;30:817-828.
[8] ORFORD NR, BAILEY M, BELLOMO R, et al. The association of time and medications with changes in bone mineral density in the 2 years after critical illness. Crit Care. 2017;21(1):69.
[9] ATAL SS, ATAL S. Ulinastatin - a newer potential therapeutic option for multiple organ dysfunction syndrome. J Basic Clin Physiol Pharmacol. 2016;27(2):91-99.
[10] ORFORD N, CATTIGAN C, BRENNAN SL, et al. The association between critical illness and changes in bone turnover in adults: a systematic review. Osteoporos Int. 2014;25(10):2335-2346.
[11] ORFORD NR, SAUNDERS K, MERRIMAN E, et al. Skeletal morbidity among survivors of critical illness. Crit Care Med. 2011;39(6):1295-1300.
[12] HUANG J, REN R, BAO Y, et al. Ulinastatin Inhibits Osteoclastogenesis and Suppresses Ovariectomy-Induced Bone Loss by Downregulating uPAR. Front Pharmacol. 2018;9:1016.
[13] MENG J, ZHOU C, ZHANG W, et al. Stachydrine prevents LPS-induced bone loss by inhibiting osteoclastogenesis via NF-κB and Akt signalling. J Cell Mol Med. 2019;23(10):6730-6743.
[14] LI S, DAI Q, ZHANG S, et al. Ulinastatin attenuates LPS-induced inflammation in mouse macrophage RAW264.7 cells by inhibiting the JNK/NF-kB signaling pathway and activating the PI3K/Akt/Nrf2 pathway. Acta Pharmacol. 2018;39(8):1294-1304.
[15] CAO C, YIN C, CHAI Y, et al. Ulinastatin mediates suppression of regulatory T cells through TLR4/NF-kB signaling pathway in murine sepsis. Int Immunopharmacol. 2018;64:411-423.
[16] TSOYI K, JANG HJ, NIZAMUTDINOVA IT, et al. Metformin inhibits HMGB1 release in LPS-treated RAW 264.7 cells and increases survival rate of endotoxaemic mice. Br J Pharmacol. 2011;162(7):1498-1508.
[17] JI J, GU Z, LI H, et al. Cryptdin-2 predicts intestinal injury during heatstroke in mice. Int J Mol Med. 2017;41:137-146.
[18] GUO C, YUAN L, WANG J, et al. Lipopolysaccharide (LPS) induces the apoptosis and inhibits osteoblast differentiation through JNK pathway in MC3T3-E1 cells. Inflammation. 2014;37(2):621-631.
[19] ZHAO Y, GAO J, ZHANG Y, et al. Cyclosporine A Promotes Bone Remodeling in LPS-Related Inflammation via Inhibiting ROS/ERK Signaling: Studies. Oxid Med Cell Longev. 2021;2021:8836599-8836599.
[20] 茹江英,丛宇,赵建宁,等.乌司他丁对骨水泥颗粒诱导MC3T3-E1鼠前成骨细胞凋亡的干预作用[J].中国组织工程研究,2014,18(43): 6945-6950.
[21] SU N, SUN Q, LI C, et al. Gain-of-function mutation in FGFR3 in mice leads to decreased bone mass by affecting both osteoblastogenesis and osteoclastogenesis. Hum Mol Genet. 2010;19(7):1199-210.
[22] IKEBUCHI Y, AOKI S, HONMA M, et al. Coupling of bone resorption and formation by RANKL reverse signalling. Nature. 2018;561(7722): 195-200.
[23] TAKAMI M, KIM N, RHO J, et al. Stimulation by toll-like receptors inhibits osteoclast differentiation. J Immunol. 2002;169(3):1516-1523.
[24] 夏维波,章振林,林华,等.原发性骨质疏松症诊疗指南(2017)[J].中国骨质疏松杂志,2019,25(3):281-309.
[25] WALSH MC, TAKEGAHARA N, KIM H, et al. Updating osteoimmunology: regulation of bone cells by innate and adaptive immunity. Nat Rev Rheumatol. 2018;14(3):146-156.
[26] PARK-MIN KH, LORENZO J. Osteoclasts: Other functions. Bone. 2022; 165:116576.
[27] KODE A, MANAVALAN JS, MOSIALOU I, et al. Leukaemogenesis induced by an activating β-catenin mutation in osteoblasts. Nature. 2014;506(7487):240-244..
[28] MAO H, LI L, FAN Q, et al. Endothelium-specific depletion of LRP1 improves glucose homeostasis through inducing osteocalcin. Nat Commun. 2021;12(1):5296-5296.
[29] KHRIMIAN L, OBRI A, RAMOS-BROSSIER M, et al. Gpr158 mediates osteocalcin’s regulation of cognition. J Exp Med. 2017;214(10): 2859-2873.
[30] GU P, TAO D, XU Y, et al. Osteocalcin inhibits myocyte aging through promotion of starvation-induced autophagy via IL-6/STAT3 signaling. Exp Gerontol. 2023;173:112082-112082.
[31] ZHOU R, LIU D, LI R, et al. Low Bone Mass is Associated with Stroke in Chinese Postmenopausal Women: The Chongqing Osteoporosis Study. Cell Biochem Biophys. 2015;71(3):1695-1701.
[32] HU MC, SHIIZAKI K, KURO-O M, et al. Fibroblast Growth Factor 23 and Klotho: Physiology and Pathophysiology of an Endocrine Network of Mineral Metabolism. Annu Rev Physiol. 2013;75(1):503-533.
[33] ZOCH ML, ABOU DS, CLEMENS TL, et al. In vivo radiometric analysis of glucose uptake and distribUTIon in mouse bone. Bone Res. 2016;4(Pt 1): 16004.
[34] WEI J, SHIMAZU J, MAKINISTOGLU MP, et al. Glucose Uptake and Runx2 Synergize to Orchestrate Osteoblast Differentiation and Bone Formation. Cell. 2015;161(7):1576-1591.
[35] RU JY, XU HD, SHI D, et al. Blockade of NF-κB and MAPK pathways by ulinastatin attenuates wear particle-stimulated osteoclast differentiation in vitro and in vivo. Biosci Rep. 2016;36(5):e00399.
[36] LI L, SAPKOTA M, KIM S, et al. Herbacetin inhibits RANKL-mediated osteoclastogenesis in vitro and prevents inflammatory bone loss in vivo. Eur J Pharmacol. 2016;777:17-25.
[37] LIU H, DONG Y, GAO Y, et al. Hesperetin suppresses RANKL-induced osteoclastogenesis and ameliorates lipopolysaccharide-induced bone loss. J Cell Physiol. 2019;234(7):11009-11022.
[38] SHUTO T, JIMI E, KUKITA T, et al. Granulocyte-macrophage colony stimulating factor suppresses lipopolysaccharide-induced osteoclast-like cell formation in mouse bone marrow cultures. Endocrinology. 1994;134(2):831-837.
[39] ISLAM S, HASSAN F, TUMURKHUU G, et al. Bacterial lipopolysaccharide induces osteoclast formation in RAW 264.7 macrophage cells. Biochem Biophys Res Commun. 2007;360(2):346-351.
[40] MÖRMANN M, THEDERAN M, NACKCHBANDI I, et al. Lipopolysaccharides (LPS) induce the differentiation of human monocytes to osteoclasts in a tumour necrosis factor (TNF) α-dependent manner: A link between infection and pathological bone resorption. Mol Immunol. 2008;45(12):3330-3337.
[41] ITOH K, UDAGAWA N, KOBAYASHI K, et al. Lipopolysaccharide promotes the survival of osteoclasts via Toll-like receptor 4, but cytokine production of osteoclasts in response to lipopolysaccharide is different from that of macrophages. J Immunol. 2003;170(7):3688-3695.
[42] CHEN YH, HSUEH KK, CHU PW, et al. AMP-activated protein kinase mediates lipopolysaccharide-induced proinflammatory responses and elevated bone resorption in differentiated osteoclasts. J Cell Biochem. 2022;123(2):275-288.
[43] 《乌司他丁用于临床常见急危重症的专家共识》专家组.乌司他丁用于临床常见急危重症的专家共识[J].中国全科医学,2023,26(26): 3207-3219.
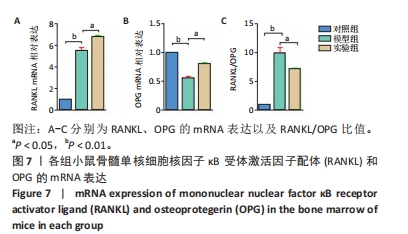
[44] BOYCE BF, XING L. The RANKL/RANK/OPG pathway. Curr Osteoporos Rep. 2007;5(3):98-104.
|