中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (24): 3562-3567.doi: 10.3969/j.issn.2095-4344.2016.24.010
• 组织构建基础实验 basic experiments in tissue construction • 上一篇 下一篇
组织工程预血管化处理对胰岛移植的影响
赵高平1,2,邓绍平1,黄孝伦2,杨卯竹2,魏玲玲2,李姝蓉2,魏 亮2
- 1四川省医学科学院•四川省人民医院,电子科技大学医学院附属医院胃肠外科,四川省成都市 610072;2器官移植转化医学四川省重点实验室,四川省成都市 610072
Effects of pre-vascularization of tissue-engineered constructs on the survival of transplanted pancreatic islets
Zhao Gao-ping1, 2, Deng Shao-ping1, Huang Xiao-lun2, Yang Mao-zhu2, Wei Ling-ling2, Li Shu-rong2, Wei liang2
- 1Department of Gastrointestinal Surgery, Sichuan Academy of Medical Science & Sichuan Provincial People’s Hospital, the Affiliated Hospital of University of Electronic Science and Technology of China, Chengdu 610072, Sichuan Province, China; 2Sichuan Provincial Key Laboratory for Translational Medicine of Organ Transplantation, Chengdu 610072, Sichuan Province, China
摘要:
文章快速阅读:
.jpg) 文题释义:
异种胰岛移植:指将来源不同物种的动物胰腺分离出胰岛细胞,通过门静脉系统、大网膜、脂肪、肌肉间等途径移植到另一物种体内,同时使用免疫抑制剂以延长移植胰岛存活时间或达到不排斥状态。胰岛移植是治疗1型糖尿病的有效方法,但由于捐献的胰腺器官日益缺乏,科学家将目光投向有稳定胰腺来源的动物。由于猪胰岛与人胰岛结构相似,所以动物实验用异种胰岛常来源于幼猪。对于异种胰岛的研究必将会对未来的临床应用有一定的意义。
组织工程血管化策略:主要有两类,第一类是基于内皮细胞等构建新的血管,在这个过程中生长因子也有促进新生血管的作用。第二类是基于支架技术,包括天然生物衍生的支架和人工合成支架。以上两种策略没有明显界限,而是相互重叠。
文题释义:
异种胰岛移植:指将来源不同物种的动物胰腺分离出胰岛细胞,通过门静脉系统、大网膜、脂肪、肌肉间等途径移植到另一物种体内,同时使用免疫抑制剂以延长移植胰岛存活时间或达到不排斥状态。胰岛移植是治疗1型糖尿病的有效方法,但由于捐献的胰腺器官日益缺乏,科学家将目光投向有稳定胰腺来源的动物。由于猪胰岛与人胰岛结构相似,所以动物实验用异种胰岛常来源于幼猪。对于异种胰岛的研究必将会对未来的临床应用有一定的意义。
组织工程血管化策略:主要有两类,第一类是基于内皮细胞等构建新的血管,在这个过程中生长因子也有促进新生血管的作用。第二类是基于支架技术,包括天然生物衍生的支架和人工合成支架。以上两种策略没有明显界限,而是相互重叠。
.jpg) 文题释义:
异种胰岛移植:指将来源不同物种的动物胰腺分离出胰岛细胞,通过门静脉系统、大网膜、脂肪、肌肉间等途径移植到另一物种体内,同时使用免疫抑制剂以延长移植胰岛存活时间或达到不排斥状态。胰岛移植是治疗1型糖尿病的有效方法,但由于捐献的胰腺器官日益缺乏,科学家将目光投向有稳定胰腺来源的动物。由于猪胰岛与人胰岛结构相似,所以动物实验用异种胰岛常来源于幼猪。对于异种胰岛的研究必将会对未来的临床应用有一定的意义。
组织工程血管化策略:主要有两类,第一类是基于内皮细胞等构建新的血管,在这个过程中生长因子也有促进新生血管的作用。第二类是基于支架技术,包括天然生物衍生的支架和人工合成支架。以上两种策略没有明显界限,而是相互重叠。
文题释义:
异种胰岛移植:指将来源不同物种的动物胰腺分离出胰岛细胞,通过门静脉系统、大网膜、脂肪、肌肉间等途径移植到另一物种体内,同时使用免疫抑制剂以延长移植胰岛存活时间或达到不排斥状态。胰岛移植是治疗1型糖尿病的有效方法,但由于捐献的胰腺器官日益缺乏,科学家将目光投向有稳定胰腺来源的动物。由于猪胰岛与人胰岛结构相似,所以动物实验用异种胰岛常来源于幼猪。对于异种胰岛的研究必将会对未来的临床应用有一定的意义。
组织工程血管化策略:主要有两类,第一类是基于内皮细胞等构建新的血管,在这个过程中生长因子也有促进新生血管的作用。第二类是基于支架技术,包括天然生物衍生的支架和人工合成支架。以上两种策略没有明显界限,而是相互重叠。摘要
背景:临床门静脉系统胰岛移植后局部缺氧导致大量胰岛细胞凋亡,影响移植效果。
目的:分析组织工程方法预先在局部形成微血管网络化对移植胰岛存活的影响以及异种胰岛移植的可行性。
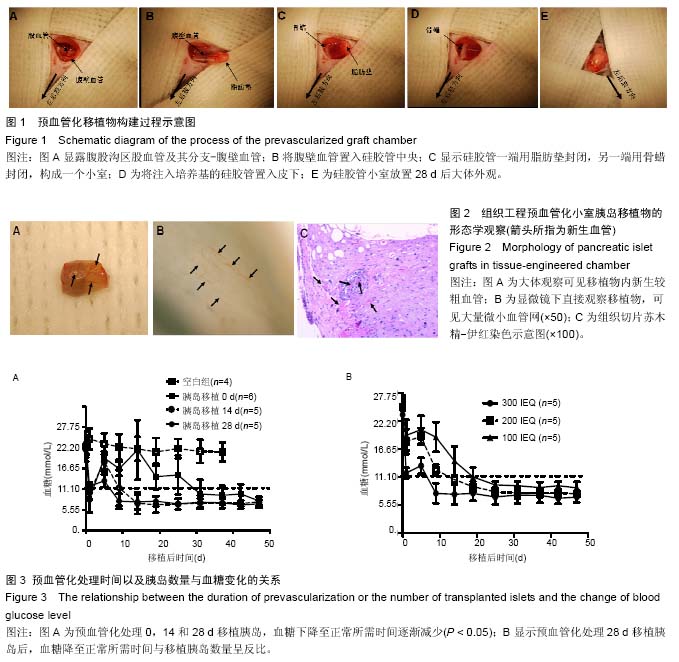
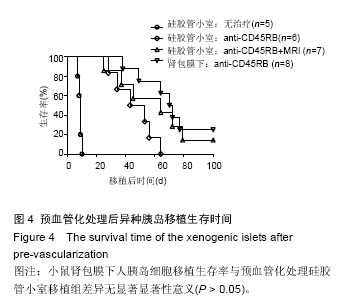
方法:将5 mm长圆柱形中空硅胶管置入糖尿病小鼠腹股沟区,中央包绕腹壁血管,注入MatrigelTM细胞培养基。分别于预血管化处理0,14以及28 d在硅胶管小室中移植同基因300个胰岛当量(IEQ)小鼠胰岛细胞,观察血糖恢复至正常时间。另在28 d于硅胶管小室内分别移植100 IEQ、200 IEQ以及300 IEQ小鼠胰岛细胞,检测血糖变化。最后将1 000 IEQ人胰岛细胞分别移植到已血管化的硅胶管小室或小鼠肾脏包膜下,并用抗CD45RB或/和抗CD40L(MR-1)抗体治疗,比较人胰岛细胞在两者中的生存情况。
结果与结论:①硅胶管小室在构建28 d后可建立丰富的微血管网。②糖尿病小鼠血糖恢复至正常水平所需的时间与预血管化处理时间以及植入的胰岛数量均呈负相关。③移植至硅胶管小室的人胰岛细胞经抗CD45RB抗体治疗后无一例长期存活,加用MR-1抗体后7只中有1只长期存活,与肾包膜下移植组(n=8,平均生存时间> 71 d)比较生存时间差异无显著性意义(P > 0.05)。在胰岛移植之前通过组织工程方法预血管化处理可显著延长移植物的存活时间。将异种胰岛移植在血管化的硅胶管小室内或为以后的临床应用提供有意义的探索。
中国组织工程研究杂志出版内容重点:组织构建;骨细胞;软骨细胞;细胞培养;成纤维细胞;血管内皮细胞;骨质疏松;组织工程
ORCID: 0000-0001-8546-0871(赵高平)
中图分类号:
.jpg) 文题释义:
异种胰岛移植:指将来源不同物种的动物胰腺分离出胰岛细胞,通过门静脉系统、大网膜、脂肪、肌肉间等途径移植到另一物种体内,同时使用免疫抑制剂以延长移植胰岛存活时间或达到不排斥状态。胰岛移植是治疗1型糖尿病的有效方法,但由于捐献的胰腺器官日益缺乏,科学家将目光投向有稳定胰腺来源的动物。由于猪胰岛与人胰岛结构相似,所以动物实验用异种胰岛常来源于幼猪。对于异种胰岛的研究必将会对未来的临床应用有一定的意义。
组织工程血管化策略:主要有两类,第一类是基于内皮细胞等构建新的血管,在这个过程中生长因子也有促进新生血管的作用。第二类是基于支架技术,包括天然生物衍生的支架和人工合成支架。以上两种策略没有明显界限,而是相互重叠。
文题释义:
异种胰岛移植:指将来源不同物种的动物胰腺分离出胰岛细胞,通过门静脉系统、大网膜、脂肪、肌肉间等途径移植到另一物种体内,同时使用免疫抑制剂以延长移植胰岛存活时间或达到不排斥状态。胰岛移植是治疗1型糖尿病的有效方法,但由于捐献的胰腺器官日益缺乏,科学家将目光投向有稳定胰腺来源的动物。由于猪胰岛与人胰岛结构相似,所以动物实验用异种胰岛常来源于幼猪。对于异种胰岛的研究必将会对未来的临床应用有一定的意义。
组织工程血管化策略:主要有两类,第一类是基于内皮细胞等构建新的血管,在这个过程中生长因子也有促进新生血管的作用。第二类是基于支架技术,包括天然生物衍生的支架和人工合成支架。以上两种策略没有明显界限,而是相互重叠。