中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (48): 7175-7184.doi: 10.3969/j.issn.2095-4344.2016.48.005
• 脊柱植入物 spinal implant • 上一篇 下一篇
前路颈椎间盘切除和椎体次全切除植骨融合治疗临近两椎节脊髓型颈椎病
沈 强1,丁 浩1,朱宗昊1,朱 亮1,魏小康1,贺旭峰2
- 1上海交通大学附属上海市第一人民医院骨科,上海市 200080;2上海中医药大学附属曙光医院创伤科,上海市 200025
-
修回日期:2016-09-12出版日期:2016-11-25发布日期:2016-11-25 -
作者简介:沈强,男,1962年生,山东省人,汉族, 1985年第二军医大学毕业,博士,主任医师,教授,研究方向为脊柱外科。 -
基金资助:上海市科技支撑项目(12441900702)
Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for treating two-level contiguous cervical spondylotic myelopathy
Shen Qiang1, Ding Hao1, Zhu Zong-hao1, Zhu Liang1, Wei Xiao-kang1, He Xu-feng2
- 1Department of Orthopedic Surgery, Shanghai First People’s Hospital, Shanghai Jiao Tong University, Shanghai 200080, China; 2Department of Traumatology, Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 200025, China
-
Revised:2016-09-12Online:2016-11-25Published:2016-11-25 -
About author:Shen Qiang, M.D., Chief physician, Professor, Department of Orthopedic Surgery, Shanghai First People’s Hospital, Shanghai Jiao Tong University, Shanghai 200080, China -
Supported by:The Key Project for Medical Science from the Shanghai Committee of Science and Technology of China, No.12441900702
摘要:
文章快速阅读:
.jpg)
中图分类号:
引用本文
沈 强,丁 浩,朱宗昊,朱 亮,魏小康,贺旭峰. 前路颈椎间盘切除和椎体次全切除植骨融合治疗临近两椎节脊髓型颈椎病[J]. 中国组织工程研究, 2016, 20(48): 7175-7184.
Shen Qiang, Ding Hao, Zhu Zong-hao, Zhu Liang, Wei Xiao-kang, He Xu-feng. Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for treating two-level contiguous cervical spondylotic myelopathy[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(48): 7175-7184.
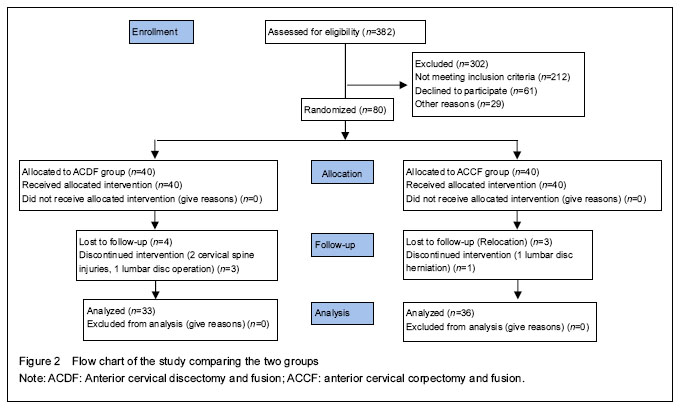
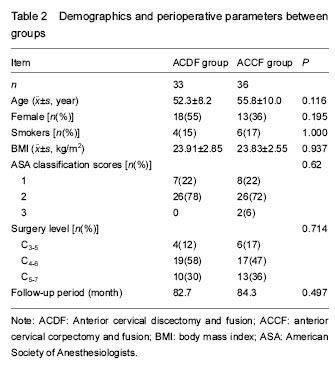
The demographic data, including age, sex, smoking status, body mass index, ASA classification scores, surgery level in each group and follow-up period were summarized in Table 2.
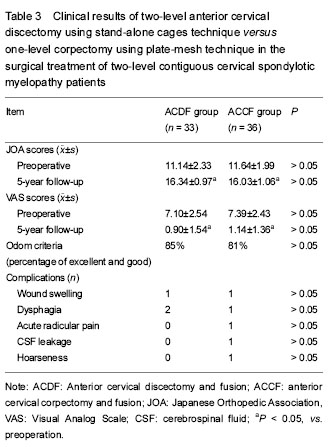
Clinical outcome

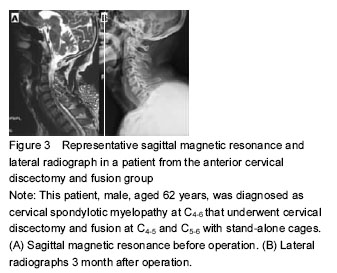
Typical cases
Case two: This patient, male, aged 44 years, was diagnosed as CSM at C5-7 that underwent cervical corpectomy and fusion at C5-7 with titanium mesh and plate and screw fixation (Figure 4).

| [1] Rao RD, Currier BL, Albert TJ, et al. Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management. J Bone Joint Surg Am. 2007;89(6):1360-1378.[2] Topuz K, Colak A, Kaya S, et al. Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: results of 3-year follow-up. Eur Spine J. 2009;18(2):238-243. [3] Chen Y, Wang X, Lu X, et al. Comparison of titanium and polyetheretherketone (PEEK) cages in the surgical treatment of multilevel cervical spondylotic myelopathy: a prospective, randomized, control study with over 7-year follow-up. Eur Spine J. 2013;22(7): 1539-1546. [4] Jang JW, Lee JK, Lee JH, et al. Effect of posterior subsidence on cervical alignment after anterior cervical corpectomy and reconstruction using titanium mesh cages in degenerative cervical disease. J Clin Neurosci. 2014;21(10):1779-1785. [5] 5. Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J. 2012;21(8):1551-1557. [6] Oh MC, Zhang HY, Park JY, et al. Two-level anterior cervical discectomy versus one-level corpectomy in cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2009;34(7):692-696. [7] Mason RL, Gunst RF, Hess JL. Statistical Design and Analysis of Experiments: With Applications to Engineering and Science. 2nd ed. New Jersey: John Wiley and Sons, Inc. 2003:14-19.[8] Hacker RJ, Cauthen JC, Gilbert TJ, et al. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine (Phila Pa 1976). 2000;25(20):2646-2654; discussion 2655.[9] Fessler RG, Steck JC, Giovanini MA. Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery. 1998;43(2):257-265; discussion 265-267.[10] Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6): 602-617.[11] Matz PG, Pritchard PR, Hadley MN. Anterior cervical approach for the treatment of cervical myelopathy. Neurosurgery. 2007;60(1 Supp1 1):S64-70.[12] Cheng L, Nie L, Zhang L, et al. Fusion versus Bryan Cervical Disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop. 2009; 33(5):1347-1351.[13] Kim SW, Limson MA, Kim SB, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J. 2009;18(2):218-231. [14] Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J. 2012;21(8):1551-1557.[15] Yang L, Gu Y, Liang L, et al. Stand-alone anchored spacer versus anterior plate for multilevel anterior cervical diskectomy and fusion. Orthopedics. 2012; 35(10):e1503-1510. [16] Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 1988;11(6):931-934.[17] Cho DY, Liau WR, Lee WY, et al. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002;51(6):1343-1349; discussion 1349-1350.[18] Cho DY, Lee WY, Sheu PC. Treatment of multilevel cervical fusion with cages. Surg Neurol. 2004;62(5):378-385, discussion 385-386.[19] Dufour T, Huppert J, Louis C, et al. Radiological analysis of 37 segments in cervical spine implanted with a peek stand-alone device, with at least one year follow-up. Br J Neurosurg. 2010;24(6):633-640.[20] Kolstad F, Nygaard ØP, Andresen H, et al. Anterior cervical arthrodesis using a "stand alone" cylindrical titanium cage: prospective analysis of radiographic parameters. Spine (Phila Pa 1976). 2010;35(16):1545-1550.[21] Ha SK, Park JY, Kim SH, et al. Radiologic Assessment of Subsidence in Stand-Alone Cervical Polyetheretherketone (PEEK) Cage. J Korean Neurosurg Soc. 2008;44(6):370-374.[22] Hwang SL, Hwang YF, Lieu AS, et al. Outcome analyses of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. J Spinal Disord Tech. 2005;18(4):326-331.[23] Uribe JS, Sangala JR, Duckworth EA, et al. Comparison between anterior cervical discectomy fusion and cervical corpectomy fusion using titanium cages for reconstruction: analysis of outcome and long-term follow-up. Eur Spine J. 2009;18(5):654-662. [24] Park Y, Maeda T, Cho W, et al. Comparison of anterior cervical fusion after two-level discectomy or single-level corpectomy: sagittal alignment, cervical lordosis, graft collapse, and adjacent-level ossification. Spine J. 2010;10(3):193-199. [25] Han YC, Liu ZQ, Wang SJ, et al. Is anterior cervical discectomy and fusion superior to corpectomy and fusion for treatment of multilevel cervical spondylotic myelopathy? A systemic review and meta-analysis. PLoS One. 2014;9(1):e87191. [26] Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007;16(9):1395-1400.[27] Schmieder K, Wolzik-Grossmann M, Pechlivanis I, et al. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006;4(6):447-453.[28] Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine (Phila Pa 1976). 1982;7(6):536-539.[29] Apfelbaum RI, Kriskovich MD, Haller JR. On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine (Phila Pa 1976). 2000;25(22): 2906-2912.[30] Heeneman H. Vocal cord paralysis following approaches to the anterior cervical spine. Laryngoscope. 1973;83(1):17-21.[31] Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976). 2002;27(22):2453-2458.[32] Riley LH 3rd, Skolasky RL, Albert TJ, et al. Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976). 2005;30(22):2564-2569.[33] Hilibrand AS, Fye MA, Emery SE, et al. Increased rate of arthrodesis with strut grafting after multilevel anterior cervical decompression. Spine (Phila Pa 1976). 2002;27(2):146-151.[34] Wang JC, McDonough PW, Endow KK, et al. A comparison of fusion rates between single-level cervical corpectomy and two-level discectomy and fusion. J Spinal Disord. 2001;14(3):222-225. |
| [1] | 张同同, 王中华, 文 杰, 宋玉鑫, 刘 林. 3D打印模型在颈椎肿瘤手术切除与重建中的应用[J]. 中国组织工程研究, 2021, 25(9): 1335-1339. |
| [2] | 刘正蓬, 王雅辉, 张义龙, 明 颖, 孙志杰, 孙 贺. 3D打印椎间融合器置入治疗脊髓型颈椎病:颈椎曲度及椎间高度恢复的半年随访[J]. 中国组织工程研究, 2021, 25(6): 849-853. |
| [3] | 罗选翔, 经 历, 潘 彬, 冯 虎. 甲钴胺联合鼠神经生长因子促进脊髓型颈椎病术后神经功能的恢复[J]. 中国组织工程研究, 2021, 25(5): 719-722. |
| [4] | 孙玛骥, 王秋安, 张星晨, 郭 冲, 袁 峰, 郭开今. 新型颈椎前路经椎弓根固定钉板系统的研制及生物力学分析[J]. 中国组织工程研究, 2021, 25(24): 3821-3825. |
| [5] | 刘金玉, 丁逸苇, 卢正操, 高天君, 崔洪鹏, 李 雯, 杜 薇, 丁 宇. 有限元分析全可视化内镜下椎板开窗减压治疗脊髓型颈椎病的生物力学特点[J]. 中国组织工程研究, 2021, 25(24): 3850-3854. |
| [6] | 张启福, 马永红, 王 涛, 胡一博, 张鹤令, 宗群川. 颈椎前路椎体次全切植骨融合和后路单开门椎管扩大成形治疗多节段脊髓型颈椎病:对颈椎活动度的影响#br#[J]. 中国组织工程研究, 2021, 25(24): 3870-3874. |
| [7] | 唐小凯, 李伟明. Nel样分子1型蛋白在脊柱融合术后促进骨性融合的作用与机制[J]. 中国组织工程研究, 2021, 25(24): 3914-3920. |
| [8] | 张振华, 刘姿辰, 禹宝庆. 聚己内酯及其复合材料在组织工程骨构建中的地位与问题[J]. 中国组织工程研究, 2021, 25(22): 3571-3577. |
| [9] | 林东鑫, 黄学成, 秦庆广, 杨 洋, 邓羽平, 谭晋川, 王 勉, 苏炜炜, 黄 涛, 黄文华. 基于运动捕捉技术比较2种颈椎手法治疗后颈椎活动范围的差异[J]. 中国组织工程研究, 2021, 25(21): 3281-3285. |
| [10] | 李岳飞, 李 瑞, 任佳彬, 刘 鑫, 孙 宁, 刘维克, 毕经纬, 孙兆忠. 三维CT指导经皮内镜后外侧入路治疗胸椎间盘突出症建立良好的骨性通道[J]. 中国组织工程研究, 2021, 25(21): 3354-3359. |
| [11] | 吴彦禹, 张春霖, 邵成龙, 严 旭, 刘小康, 王永魁, 李东哲. 二维距离法和三维体积法对内镜下微创颈椎管成形后突出椎间盘再吸收的定量测量[J]. 中国组织工程研究, 2021, 25(21): 3390-3394. |
| [12] | 曲星月, 周建强, 徐雪彬, 张少杰, 李志军, 王 星. 儿童下颈椎前路4种内固定模型的螺钉-骨抗拔出有限元分析[J]. 中国组织工程研究, 2021, 25(18): 2816-2821. |
| [13] | 刘金磊, 殷 力, 张 翼, 王海涛, 李庄严, 夏培格, 乔仁秋. 全膝关节置换装假体前氨甲环酸静滴联合局部鸡尾酒复合氨甲环酸多点注射对失血与疼痛的影响[J]. 中国组织工程研究, 2021, 25(18): 2833-2839. |
| [14] | 阮汉江, 金根洋, 李新武, 姚 建, 武 鹏, 张 引, 张 帅, 肖 俊. 三种后路单节段固定方式治疗Ⅱ型Hangman骨折的生物力学性能[J]. 中国组织工程研究, 2021, 25(15): 2309-2314. |
| [15] | 陈 江, 李晋玉, 郑晨颖, 白春晓, 张 帆, 刘楚吟, 赵学千, 袁巧妹, 邸学士, 康晟乾, 贾育松. 双节段颈人工椎间盘置换与颈椎间盘切除融合后颈椎矢状位参数的变化[J]. 中国组织工程研究, 2021, 25(15): 2341-2346. |
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
Design
.jpg)
The cervical lordoses were indicated by the methods of Cobb angle of C2-7 and operated segments. The C2-7 Cobb angle was the angle between the inferior endplate line of C2 and inferior endplate line of C7 in a neutral position. The segmental Cobb angle was the angle between the superior endplate line of the cephalad vertebral body and the inferior endplate line of caudal vertebral body of the operated segments in a neutral position. Lordosis is shown as a positive value and kyphosis is shown as a negative value (Figure 1). The Segmental height was measured using the method of Oh et al. [6] and defined as the distance between the midlines of involvedcranial vertebral bodies and caudal vertebral bodies (Figure 1). Instrument subsidence was recorded when the loss of segmental height correction was over 3 mm. Fusion was considered according to the following accepted criteria: (1) absence of motion between the spinous processes at dynamic lateral radiographs, (2) presence of continuous bridging bony trabeculae at the graft-endplate interface[8].
.jpg)
evaluations included the segmental and C2-7 Cobb angles, segmental heights, the instrument subsidence rates, and the instrument dislocations before and at 5-year follow-up after surgery.
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
文章快速阅读:
.jpg)
前路颈椎间盘切除植骨融合是指自颈部前方经过颈前内脏鞘与血管鞘间隙显露颈椎前方,在两侧颈长肌之间,切除病变椎间隙的前纵韧带,纤维环,髓核,及软骨终板,并切除突入椎管的髓核和椎体后缘增生压迫脊髓的骨赘,达到脊髓前方减压后,该椎间隙植骨融合的手术方式。 中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||