中国组织工程研究 ›› 2026, Vol. 30 ›› Issue (12): 3075-3082.doi: 10.12307/2026.664
• 组织构建临床实践 clinical practice in tissue construction • 上一篇 下一篇
悬吊保护下佩戴智能助行器主动辅助偏瘫患者行走:随机对照试验
马善新1,郑建玲2,程 健1,林 禧1,李秋缘1,王 丽1,曾杨康1,宋鲁平3
- 1深圳大学总医院康复医学科,广东省深圳市 518055;2中国康复研究中心北京博爱医院物理疗法科,北京市 100068;3深圳市南山区人民医院康复医学科,广东省深圳市 518300
-
收稿日期:2025-04-02接受日期:2025-08-06出版日期:2026-04-28发布日期:2025-09-30 -
通讯作者:宋鲁平,女,1964年生,山东省人,汉族,博士,主任医师,深圳市南山区人民医院康复医学科,广东省深圳市 518300 -
作者简介:马善新,男,1986年生,广西壮族自治区南宁市人,壮族,硕士,副主任医师,主要从事肌骨超声及脑卒中康复研究。 并列第一作者:郑建玲,中国康复研究中心北京博爱医院物理疗法科,北京市 100068 -
基金资助:深圳市南山区科技发展计划项目(NS2022150),项目负责人:马善新
Early intelligent active assistance in walking for hemiplegic patients under suspension protection: #br# a randomized controlled trial
Ma Shanxin1, Zheng Jianling2, Cheng Jian1, Lin Xi1, Li Qiuyuan1, Wang Li1, Zeng Yangkang1, Song Luping3
- 1Department of Rehabilitation Medicine, Shenzhen University General Hospital, Shenzhen 518055, Guangdong Province, China; 2Department of Physical Therapy, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing 100068, China; 3Department of Rehabilitation Medicine, Shenzhen Nanshan People’s Hospital, Shenzhen 518300, Guangdong Province, China
Ma Shanxin, MS, Associate chief physician, Department of Rehabilitation Medicine, Shenzhen University General Hospital, Shenzhen 518055, Guangdong Province, China
-
Received:2025-04-02Accepted:2025-08-06Online:2026-04-28Published:2025-09-30 -
Contact:Song Luping, PhD, Chief physician, Department of Rehabilitation Medicine, Shenzhen Nanshan People’s Hospital, Shenzhen 518300, Guangdong Province, China -
About author:Zheng Jianling, Department of Physical Therapy, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing 100068, China Ma Shanxin and Zheng Jianling contributed equally to this work. -
Supported by:Shenzhen Nanshan District Science and Technology Development Plan Project, No. NS2022150 (to MSX)
摘要:
背景:偏瘫是常见的脑卒中相关病症,其运动功能障碍方面的问题相关研究较多,但痉挛方面却研究不足。异常的肌肉张力极大地阻碍了偏瘫患者行走功能的恢复。
目的:探讨脑脑卒中患者早期悬吊保护下佩戴智能助行器(Personal assistant machine,PAM)进行训练,能否提高步行能力,预防肌肉痉挛。
方法:将来自深圳大学总医院及中国康复研究中心的32例早期脑卒中患者随机分配至试验组(n=16)和对照组(n=16)。两组均在悬吊保护下进行为期4周的步态训练,每周5 d,每日30 min。试验组接受了额外的PAM训练。干预前1周内及干预4周后采用Cortex 动作捕捉系统进行三维步态分析、通过Brunnstrom分期、Fugl-Meyer运动功能下肢部分(FMA-LE)评分、Fugl-Meyer平衡功能(FMB)评分和改良Ashworth(MAS)评分进行评估。
结果与结论:经过4周的干预,所有评估指标在组内均发生了显著变化。试验组的MAS评分略有显著增加(P < 0.05,d=|0.15|),而对照组则增加幅度较大(P < 0.05,d=|1.48|)。试验组在步行速度(从16.5 cm/s
提升至38.44 cm/s,P < 0.05,d=|4.01|)、步频(从46.44步/min提升至64.94步/min,
P < 0.05,d=|2.32|)、步长(从15.50 cm提升至29.81 cm,P < 0.05,d=|3.44|)以及患侧屈髋峰值和患侧屈膝峰值(d=|1.82|至|2.17|)方面均有更大幅度的提升。经过4周的治疗,试验组在步行速度(38.44 cm/s vs. 26.63 cm/s,P < 0.05,d=|2.75|)、步长、患侧屈髋峰值和患侧屈膝峰值(d=|1.31|至|1.45|)、步频(64.94步/min vs. 59.38
步/min,P < 0.05,d=|0.85|)以及支撑相减少(双侧:24.31% vs. 28.38%,P < 0.05,d=|0.88|;非患侧:66.19% vs. 70.13%,P < 0.05,d=|0.94|)方面均相较于对照组显著改善。上述结果证实,对于早期偏瘫患者,在悬吊保护下佩戴智能助行器进行步态训练,有助于建立正确的步态模式并预防肌肉痉挛,从而促进运动功能的改善。
https://orcid.org/0000-0001-9248-5833 (Ma Shanxin); https://orcid.org/0009-0001-4704-5164 (Song Luping)
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
中图分类号:
引用本文
马善新, 郑建玲, 程 健, 林 禧, 李秋缘, 王 丽, 曾杨康, 宋鲁平. 悬吊保护下佩戴智能助行器主动辅助偏瘫患者行走:随机对照试验[J]. 中国组织工程研究, 2026, 30(12): 3075-3082.
Ma Shanxin, Zheng Jianling, Cheng Jian, Lin Xi, Li Qiuyuan, Wang Li, Zeng Yangkang, Song Luping. Early intelligent active assistance in walking for hemiplegic patients under suspension protection: #br# a randomized controlled trial[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3075-3082.
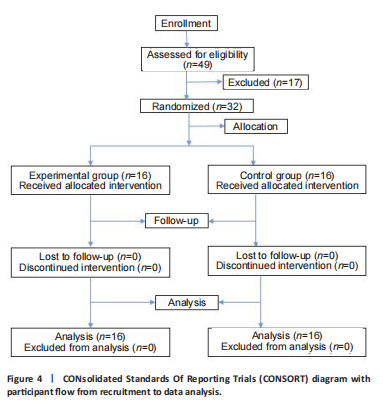
The number of subjects included in the study
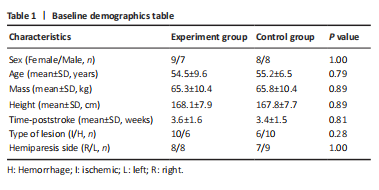
A total of 49 patients with early-stage stroke were screened, of whom 32 met the eligibility criteria and were randomized to undergo the intervention, as illustrated in Figure 4. A comparison of baseline characteristics, presented in Tables 1 and 2, revealed no statistically significant differences in demographic or clinical features among the participants (P > 0.05).
Analysis of differences in outcome indicators among groups of subjects
Changes in the indicators after 4 weeks of intervention in the control group and experimental group are shown in Figures 5–7.
After 4 weeks, the MAS scores exhibited minimal changes in both groups. The experimental group showed a slight but statistically significant increase (from 5.91 to 6.13, P < 0.05, d=|0.15|), whereas the control group demonstrated a substantial increase (from 5.81 to 7.81, P < 0.05, d=|1.48|). Post-intervention, the MAS scores in the control group were significantly higher than those in the experimental group (7.81 vs. 6.13, P < 0.05, d=|1.11|).
Among the spatiotemporal gait parameters assessed, the experimental group displayed highly significant and clinically meaningful improvements in gait velocity (from 16.5 to 38.44 cm/s, P < 0.05, effect size d=|4.01|), step frequency (from 46.44 to 64.94 steps/min, P < 0.05, d=|2.32|), and stride length (from 15.50 to 29.81 cm, P < 0.05, d=|3.44|). In contrast, the control group exhibited changes of greater magnitude but with moderate effect sizes (d=|1.35| to |1.73|) for the same parameters post-intervention.
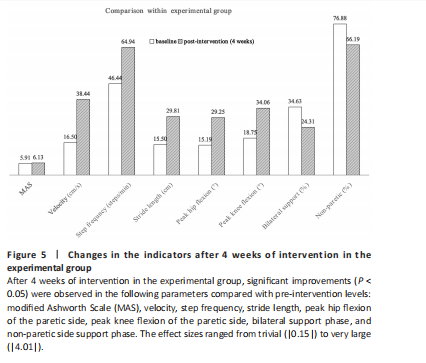
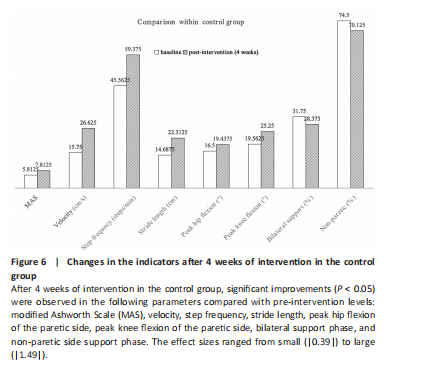
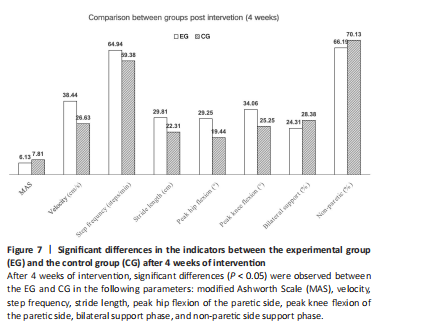
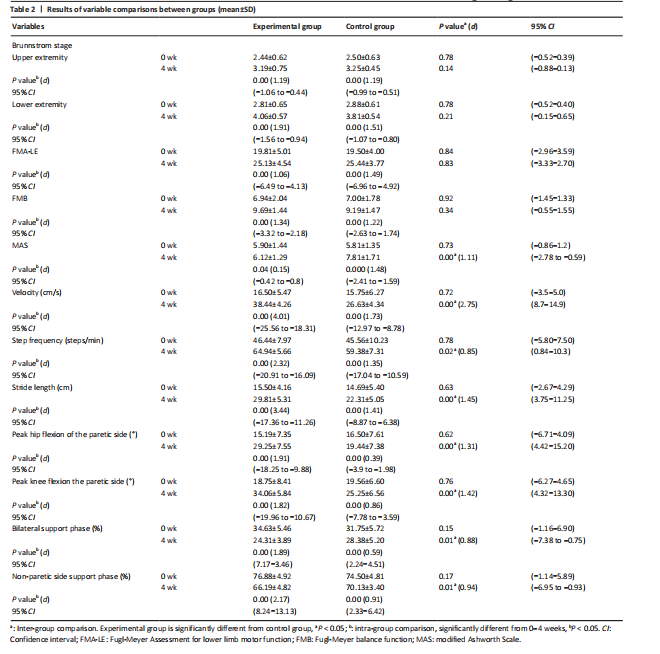
Both groups demonstrated statistically significant improvements in peak flexion angles of the hip and knee joints (P < 0.05), along with significant reductions in both bilateral and non-paretic support phases (P < 0.05). Within the experimental group, effect sizes for these kinematic measures ranged from large to very large (d=|1.82| to |2.17|), while in the control group, they ranged from small to moderate (d=|0.39| to |0.91|). Comparison between groups after intervention indicated no significant differences in Brunnstrom, FMA and FMB scores (P > 0.05). Following a 4-week intervention, the EG demonstrated statistically significant improvements in gait parameters compared to the CG. Specifically, EG exhibited a 28.6% increase in walking velocity (from 26.63 cm/s to 38.44 cm/s; P < 0.05), with a very large treatment effect size (d=|2.75|). Additionally, EG showed significant and substantial increases in other kinematic outcomes: Stride length increased by 25.3% (from 22.31 cm to 29.81 cm; P < 0.05, d=|1.45|), peak hip flexion improved by 33.5% (from 19.44° to 29.25°; P < 0.05, d=|1.31|), and peak knee flexion increased by 25.9% (from 25.25° to 34.06°; P < 0.05, d = 1.42). Moderate yet statistically significant differences were observed in temporal-spatial parameters. Specifically, step frequency exhibited a significant increase (64.94 steps/min vs. 59.38 steps/min; P < 0.05, d=|0.85|). Concurrently, the support phase decreased significantly: bilaterally, it was reduced from 28.375% to 24.31% (P < 0.05, d=|0.88|), and in the non-paretic side, it decreased from 70.13% to 66.19% (P < 0.05, d=|0.94|). Adverse reaction analysis None of the test subjects experienced adverse reactions during the trial.

| [1] FEIGIN VL, BRAININ M, NORRVING B, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18-23. [2] MALIK AN, TARIQ H, AFRIDI A, et al. Technological advancements in stroke rehabilitation. J Pak Med Assoc. 2022;72(8):1672-1674. [3] MORI H, TAMARI M, MARUYAMA H. Relationship between walking ability of patients with stroke and effect of body weight-supported treadmill training. J Phys Ther Sci. 2020;32(3):206-209. [4] MEHRHOLZ J, T HOMAS S, KUGLER J, et al. Electromechanical-assisted training for walking after stroke. Cochrane Database Syst Rev. 2020;10(10):CD006185. [5] HSU CY, CHENG YH, LAI CH, et al. Clinical non-superiority of technology-assisted gait training with body weight support in patients with subacute stroke: a meta-analysis. Ann Phys Rehabil Med. 2020;63(6):535-542. [6] GIOYANNINI S, IACOVELLI C, BRAE F, et al. Robotic-assisted rehabilitation for balance and gait in stroke patients (ROAR-S): study protocol for a preliminary randomized controlled trial. Trials. 2022;23(1):872. [7] DE MIGUEL-FERNÁNDEZ J, LOBO-PRAT J, PRINSEN E, et al. Control strategies used in lower limb exoskeletons for gait rehabilitation after brain injury: a systematic review and analysis of clinical effectiveness. J Neuroeng Rehabil. 2023;(20):23. [8] NAKAJIMA T, SANKAI Y, TAKATA S, et al. Cybernic treatment with wearable cyborg Hybrid Assistive Limb (HAL) improves ambulatory function in patients with slowly progressive rare neuromuscular diseases: a multicentre, randomised, controlled crossover trial for efficacy and safety (NCY-3001). Orphanet J Rare Dis. 2021;16(1):304. [9] NADOERF F, WRIGHT MA, LOPEZ-MATAS H, et al. User-centered design of a personal-use exoskeleton: a clinical investigation on the feasibility and usability of the ABLE exoskeleton device for individuals with spinal cord injury to perform skills for home and community environments. Front Neurosci. 2024;18:1437358. [10] BATTAGLIA M, BORG MB, LORO A, et al. post-stroke spasticity: follow-up and functional implications of chronic long-term treatment with botulinum toxin. Eur J Phys Rehabil Med. 2024;60(4):581-590. [11] BAYLE N, MAISONOBE P, RAYMOND R, et al. Composite active range of motion (CXA) and relationship with active function in upper and lower limb spastic paresis. Clin Rehabil. 2020;34(6):803-811. [12] CHERNI Y, HAJIZADEH M, DAL MASO F, et al. Effects of body weight support and guidance force settings on muscle synergy during Lokomat walking. Eur J Appl Physiol. 2021;121(11):2967-2980. [13] Förster A, Gass A, Kern R, et al. Brain imaging in patients with transient ischemic attack: a comparison of computed tomography and magnetic resonance imaging. Eur Neurol. 2012;67(3):136-141. [14] RIZVI MR, SHARNMA A, MALKI A, et al. Enhancing cardiovascular health and functional recovery in stroke survivors: a randomized controlled trial of stroke-specific and cardiac rehabilitation protocols for optimized rehabilitation. J Clin Med. 2023;12(20):6589. [15] LI L, LIU R, HE J, et al. Effects of threshold respiratory muscle training on respiratory muscle strength, pulmonary function and exercise endurance after stroke: a meta-analysis. J Stroke Cerebrovasc Dis. 2024:33(8):107837. [16] SCHRODER J, TRUIJERN S, VANRIEKNGE T, et al. Feasibility and effectiveness of repetitive gait training early after stroke: a systematic review and meta-analysis. J Rehabil Med. 2019;51(2):78-88. [17] LIANG S, HONG ZQ, CAI Q, et al. Effects of robot-assisted gait training on motor performance of lower limb in poststroke survivors: a systematic review with meta-analysis. Eur Rev Med Pharmacol Sci. 2024;28(3):879-898. [18] JOHNSTON TE, KELLER S, DENZER-WEILER C, et al. A clinical practice guideline for the use of ankle-foot orthoses and functional electrical stimulation post-stroke. J Neurol Phys Ther. 2021;45:112-196. [19] LEE Y, KIM GB, SHIN S. Association between lower limb strength asymmetry and gait asymmetry: implications for gait variability in stroke survivors. J Clin Med. 2025;14(2):380. [20] SEO JW, KANG GH, KIM CH, et al. Characteristics of gait event and muscle activation parameters of the lower limb on the affected side in patients with hemiplegia after stroke: a pilot study. Arch Rehabil Res Clin Transl. 2023;5(4): 100274. [21] SENDA J, ITO K, KOTAKE T, et al. Investigation of inpatient convalescent rehabilitation outcomes in branch atheromatous disease. J Stroke Cerebrovasc Dis. 2023;32(3):106937. [22] ZHIYAN H, NIN L, BAOYUN C, et al. Rehabilitation nursing for cerebral stroke patients within a suitable recovery empty period. Iran J Public Health. 2017; 46(2):180-185. [23] MAO HF, HSUEH IP, Tang PF, et al. Analysis and comparison of the psychometric properties of three balance measures for stroke patients. Stroke. 2002;33(4):1022-1027. [24] HERNAN ED, FORERO SM, GALEANO CP, et al. Intra and inter-rater reliability of Fugl-Meyer assessment of lower extremity early after stroke. Braz J Phys Ther. 2021;25(6):709-718. [25] BOHANNON RW, SMITH MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67(2):206-207. [26] PISCITELLI D, PELLICCIARI L, VIDMAR T, et al. Is it time to go beyond the modified ashworth scale? Letter to the editor on “reliability of the modified Ashworth scale after stroke for 13 muscle groups”. Arch Phys Med Rehabil. 2023;104(10): 1735-1736. [27] VIDMAR T, GOLJAR KN, PUH U. Reliability of the modified ashworth scale after stroke for 13 muscle groups. Arch Phys Med Rehabil. 2023; 104(10):1606-1611. [28] GILLESPIE J, ARNOLD D, TRAMMELL M, et al. Utilization of overground exoskeleton gait training during inpatient rehabilitation: a descriptive analysis. J Neuroeng Rehabil. 2023;20(1):102. [29] BATTERHAM AM, HOPKINS WG. Making meaningful inferences about magnitudes. Int J Sports Physiol Perform. 2006;1(1):50-57. [30] SKVORTSOV DV, KAURKIN SN, IVANOVA GE. Targeted biofeedback training to improve gait parameters in subacute stroke patients: a single-blind randomized controlled trial. Sensors (Basel). 2024;24(22):7212. [31] MAZZUCCHELLI M, MAZZOLENI D, CAMPANINI I, et al. Evidence-based improvement of gait in post-stroke patients following robot-assisted training: a systematic review. NeuroRehabilitation. 2022;51(4):595-608. [32] HUBER J, ELWERTl N, POWELL ES, et al. Effects of dynamic body weight support on functional independence measures in acute ischemic stroke: a retrospective cohort study. J Neuroeng Rehabil. 2023;20(1):6. [33] MEYER A, H RDLICKA HC, CUTLER E, et al. A novel body weight-supported postural perturbation module for gait and balance rehabilitation after stroke: preliminary evaluation study. JMIR Rehabil Assist Technol. 2022; 9(1):e31504. [34] NAGHDI S, A NSARI NN, RASTGOO M, et al. A pilot study on the effects of low frequency repetitive transcranial magnetic stimulation on lower extremity spasticity and motor neuron excitability in patients after stroke. J Bodyw Mov Ther. 2015;19(4):616-623. [35] CHEN S, Z HANGh W, WANG D, et al. How robot-assisted gait training affects gait ability, balance and kinematic parameters after stroke: a systematic review and meta-analysis. Eur J Phys Rehabil Med. 2024;60(3):400-411. [36] XU P, HUANG Y, WANG J, et al. Repetitive transcranial magnetic stimulation as an alternative therapy for stroke with spasticity: a systematic review and meta-analysis. J Neurol. 2021;268(11):4013-4022. [37] KOLDAS D OGAN Ş. Robot-assisted gait training in stroke. Turk J Phys Med Rehabil. 2024;70(3):293-299. [38] MA ZZ, WU JJ, HUA XY, et al. Evidence of neuroplasticity with brain-computer interface in a randomized trial for post-stroke rehabilitation: a graph-theoretic study of subnetwork analysis. Front Neurol. 2023;14: 1135466. [39] DELUCA C, MORETTO G, DI MATTEO A, et al. Hemi-and monoataxia in cerebellar hemispheres and peduncles stroke lesions: topographical correlations. Cerebellum. 2012;11(4):917-924. [40] KAYABINAR B, ALEMDAROGLU-GURBUZ İ, YILMAZ Ö. The effects of virtual reality augmented robot-assisted gait training on dual-task performance and functional measures in chronic stroke: a randomized controlled single-blind trial. Eur J Phys Rehabil Med. 2021;57(2):227-237. [41] DATTOLA R, GIRLANDA P, VITA G, et al. Muscle rearrangement in patients with hemiparesis after stroke: an electrophysiological and morphological study. Eur Neurol. 1993;33(2):109-114. [42] HERING GO, BERTSCHINGER R, STEOPAN J. A quadriceps femoris motor pattern for efficient cycling. PLoS One. 2023;18(3):e0282391. [43] WLODARCZYK L, CICHON N, SALUK-BIJAK J, et al. Neuroimaging techniques as potential tools for assessment of angiogenesis and neuroplasticity processes after stroke and their clinical implications for rehabilitation and stroke recovery prognosis. J Clin Med. 2022;11(9):2473. [44] RUFF J, UDEH B, LINDER S. Cardiac rehabilitation for persons with stroke: a cost-effectiveness analysis. Clin Rehabil. 2025;39(2):153-160. |
| [1] | 王 峥, 程 吉, 于金龙, 刘文红, 王召红, 周鲁星. 水凝胶材料在脑卒中治疗中的应用进展与未来展望[J]. 中国组织工程研究, 2026, 30(8): 2081-2090. |
| [2] | 高 峰, 张 俊, 余文君, 单于玉婧, 赵 乐, 胡雨婷, 王俊华, 刘永富. 佩戴腕手矫形器对脑卒中患者手功能障碍作用的Meta分析[J]. 中国组织工程研究, 2026, 30(8): 2124-2131. |
| [3] | 陶代菊, 苏海玉, 王宇琪, 沈志强, 何 波. 高/低表达miR-122-5p稳转PC12细胞株的构建和鉴定[J]. 中国组织工程研究, 2026, 30(7): 1790-1799. |
| [4] | 周 坚, 张 涛, 周威力, 赵星丞, 王 军, 沈 杰, 钱 丽, 陆 明. 抗阻训练对骨质疏松并肌少症患者股四头肌质量及膝关节功能的影响[J]. 中国组织工程研究, 2026, 30(5): 1081-1088. |
| [5] | 杨媛媛, 周珊珊, 成小菲, 冯露叶, 汤继芹. 非侵入性脑刺激治疗脑卒中后下肢运动功能障碍的网状Meta分析[J]. 中国组织工程研究, 2026, 30(4): 1008-1018. |
| [6] | 侯 兵, 赵鸿斐, 车鹏程, 王梓祎, 高 赞, 陈琳渝, 王金芝, 窦 娜. 经颅直流电刺激即刻和3周后上肢运动功能及脑功能分析[J]. 中国组织工程研究, 2026, 30(12): 3066-3074. |
| [7] | 程 乐, 朱才丰, 周冰原, 高大红, 崔晓雅, 李 静, 王雪伟, 杨高尚, 陈希阳. 靶向炎症细胞因子治疗脑卒中的机制:开放全基因组关联研究大数据分析[J]. 中国组织工程研究, 2026, 30(12): 3198-3216. |
| [8] | 高世爱, 陈金慧, 曹新燕, 冷晓轩, 刘西花. 腹部电刺激与核心稳定训练改善脑卒中假性延髓麻痹患者平衡及咳嗽能力[J]. 中国组织工程研究, 2026, 30(11): 2736-2744. |
| [9] | 张月婷, 李静林, 傅振燚, 晏 斐, 高 宇, 刘佳鑫. 内质网应激促进铁死亡加重脑缺血再灌注损伤[J]. 中国组织工程研究, 2026, 30(11): 2806-2813. |
| [10] | 王德刚, 陈国华, 梅俊华, 王俊力, 郑 丽. 夜间睡眠时长对中老年慢性病共病人群新发心脑血管疾病的影响[J]. 中国组织工程研究, 2026, 30(11): 2814-2822. |
| [11] | 周欣滢, 孙新月, 朱文浩. 胰岛素样生长因子与缺血性脑卒中:基于欧洲人群全基因组的关联分析[J]. 中国组织工程研究, 2026, 30(11): 2909-2919. |
| [12] | 胡 鑫, 万海丽, 杜 亮, 李永杰, 夏 渊. Theta刺激治疗脑卒中患者下肢运动功能和日常活动能力的Meta分析[J]. 中国组织工程研究, 2026, 30(10): 2576-2583. |
| [13] | 田 梦, 娄天伟, 张永臣, 贾红玲. 组织蛋白酶F有潜力成为脑卒中风险预测血清生物标记物:GWAS数据库数据分析[J]. 中国组织工程研究, 2026, 30(10): 2662-2670. |
| [14] | 王 峥, 程 吉, 于金龙, 刘文红, 王召红, 周鲁星. 水凝胶材料在脑卒中治疗中的应用进展与未来展望[J]. 中国组织工程研究, 2025, 29(在线): 1-10. |
| [15] | 王 咪, 马书杰, 刘 杨, 齐 瑞. 缺血性脑卒中铁死亡特征基因NFE2L2的鉴定与验证[J]. 中国组织工程研究, 2025, 29(7): 1466-1474. |
In recent years, the integration of body weight support systems with smart assistive devices has introduced innovative approaches to stroke rehabilitation. The body weight support system mitigates fall risks by providing dynamic body weight support, enabling multiplanar gait training in a safe environment [6]. Intelligent walking aids, such as exoskeletons and wearable gait-assist devices, utilize sensors to monitor joint kinematics in real time and guide standardized movements through mechanical feedback [7]. For example, the hybrid assistive limb employs surface electromyography to drive hip and knee torque assistance, significantly enhancing gait symmetry in stroke patients [8], while the Ekso GT utilizes inertial measurement units to deliver real-time gait-phase cues, thereby reducing compensatory trunk tilt [9]. However, current devices predominantly focus on mid-to-late rehabilitation phases, with limited evidence supporting their efficacy in preventing early-stage spasticity and establishing correct motor patterns.
Post-stroke spasticity, a prevalent secondary complication, is closely linked to the reactivation of abnormal spinal reflex pathways and impaired cortical inhibitory function [10]. Clinical studies suggest that improper movement patterns during the early stages of recovery reinforce the neuroplastic basis of spasticity through gamma-loop mechanisms [11]. Therefore, simultaneously suppressing abnormal muscle tone elevation and reinforcing correct motor patterns during initial gait training is critical for optimizing rehabilitation outcomes. Smart assistive devices present a promising solution due to their biomechanical modulation capabilities: they dynamically adjust support torque to restrict aberrant joint motion while promoting motor learning through visual-auditory feedback [12]. However, clinical evidence validating their efficacy in early-stage stroke rehabilitation remains limited.
Our study introduces an innovative protocol integrating the suspension protection system (SPS) and personal assistant machine (PAM) for early-stage gait training. The SPS provides pure protective support, alleviating fear of falling to enable high-intensity repetitive training without rigid trunk restraint, while PAM’s real-time biomechanical feedback standardizes movement patterns, suppressing spasticity triggers through peripheral sensory modulation and central motor control enhancement. Through a randomized controlled trial, we aim to evaluate its efficacy in improving ambulation and reducing spasticity in stroke patients.
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
Design
The study utilized a prospective, randomized controlled trial design. Quantitative data were compared using independent t-tests (between groups) and paired t-tests (within groups), while categorical data were analyzed with chi-square tests and non-parametric data with Mann-Whitney U tests.
Time and setting
The experiment was conducted from January 2023 to June 2023 in the Department of Rehabilitation Medicine at Shenzhen University General Hospital and the Department of Rehabilitation Medicine at China Rehabilitation Research Center.
Participants
Between January and June 2023, the China Rehabilitation Research Center (Beijing Boai Hospital, Beijing, China) and the Department of Rehabilitation Medicine at Shenzhen University General Hospital, China screened the medical records of stroke patients based on the following inclusion and exclusion criteria. All procedures outlined in this study were approved by the Medical Ethics Committee of Shenzhen University General Hospital (serial number: KYLL-20230103A) on March 28, 2022, and by the Medical Ethics Committee of China Rehabilitation Research Center (serial number: CRRC-IEC-RF-SC-005-01) on May 9, 2020.
Inclusion criteria: (1) Age at onset: 18–75 years, with signed informed consent; (2) Absence of significant cognitive impairment [Mini-Mental State Examination (MMSE) score > 25]; (3) Initial diagnosis of stroke according to the World Health Organization’s clinical definition, confirmed by a single lesion on computed tomography (CT) or magnetic resonance imaging (MRI) [13]; (4) Stroke onset within 3 months prior to screening; (5) Brunnstrom stages II to IV; (6) Ability to complete all trial procedures.
Exclusion criteria: (1) Uncontrolled orthostatic hypotension (patients may be included after effective management); (2) Presence of other severe neurological disorders (e.g., dementia, dysphasia); (3) Severe psychiatric conditions; (4) Unstable physical impairments (e.g., fractures, severe osteoporosis); (5) Inability to bear weight during walking.
Baseline demographic, neurological, and physical characteristics were extracted from medical records and assessed during the initial study visit.
The study utilized a prospective, randomized controlled trial design. Initially, a baseline assessment was conducted, followed by the randomization process, which assigned participants to either the experimental group or the control group using a predetermined randomization table. An independent researcher generated the random sequence, arranged in blocks of 10. To ensure allocation concealment, the assignments were placed in opaque, sequentially numbered, sealed envelopes. An independent researcher, uninvolved in participant recruitment or follow-up assessments, managed and sequentially opened the envelopes to allocate participants. Four weeks later, a post-intervention assessment was conducted. After 4 weeks, the second investigation sequence (post hoc test) was carried out. This study was registered on April 6, 2023, with the Chinese Clinical Trial Registry (Registration Number: ChiCTR2300070247) and has been written in accordance with the Consolidated Standards Of Reporting Trials (CONSORT) checklist for reporting randomized controlled trials.
Methods
Intervention
Guided by evidence on aerobic exercise-induced neuroplasticity in stroke recovery and aligned with the American Heart Association’s post-stroke rehabilitation guidelines, we implemented a structured 60-minute aerobic training protocol. Systematic physiological monitoring, including heart rate, blood pressure, core temperature, and subjective fatigue metrics, was conducted to ensure intervention safety [14].
Both groups completed a standardized, intensive 4-week protocol involving daily therapeutic sessions. The intervention comprised 5 consecutive training days per week, each structured as follows: (1) Evidence-based physiotherapy (30 minutes), focusing on postural control through core stabilization exercises, progressive resistance training for lower extremity strength enhancement, dynamic balance retraining using force plate biofeedback, and locomotor endurance development via cycle ergometry [15]; (2) Task-specific ambulation training (30 minutes), implementing graded overground walking protocols with body weight support as needed, in alignment with current stroke gait rehabilitation guidelines [16, 17]. While the control group received the same therapeutic content and duration as the experimental group, the sole methodological difference was the exclusion of PAM during ambulation sessions.
The intervention employed two devices: (1) the PAM is an intelligent powered wearable lower limb walking assistive device developed by Gulin Electric Appliance (Shenzhen) Co., Ltd., with the product model PAM-01 (Figure 1). During the walking training process, the integrated APP intelligent motion sensor detects the angular velocity of hip flexion and provides external auxiliary power to assist the hip joint, thereby facilitating forward walking. The level of assistance and the movement mode can be customized according to the severity of hemiplegia. The device offers three adjustable assistance modes (stage IV–3.0 kgf, stage III–4.0 kgf, and stage II–5.0 kgf), while the assistance for the unaffected limb can be set to 0 kgf. (2) The SPS (model: XY-K-G3, manufactured by Xiangyu Medical Co. Guangzhou), as depicted in Figure 2, consists of a bracket, a lifting column, and a weight-bearing sling. This system is designed solely to provide protection and does not incorporate a weight reduction function. It is equipped with casters to facilitate mobility and support walking training on the ground.
Preparation for training involved the following sequential procedures: positioning the PAM onto the patient’s posterior aspect, aligning its structural frame with the iliac crest level; securing the anterior stabilization belt across the abdominal region at umbilical height; attaching bilateral shoulder harnesses in a crosswise configuration from the posterior thoracic region to the acromioclavicular joints; and affixing the torque-generating assemblies proximal to the patellofemoral joints to augment hip flexion kinematics (Figure 2).
Ankle stabilization was achieved through elastic bandage application to maintain dorsiflexion alignment, effectively addressing equinovarus deformity and optimizing swing-phase kinematics [18]. Footwear standardization required the use of personal shoes, with ad libitum use of ankle-foot orthoses permitted during ambulation training.
During exercise sessions, therapists implemented a personalized support strategy, informed by prior gait disturbance research, to address individual gait deficiencies [19]. They ensured knee stability-both anteriorly and posteriorly-during each step, enhancing joint control and preventing hyperextension or excessive flexion [20]. In cases of muscle weakness or impaired motor control in the affected limbs, a dual-therapist approach was employed: one therapist focused on trunk rotation and center of gravity shifts, while the other closely monitored and managed knee movement to prevent overextension during weight-bearing. As participants progressed, their reliance on therapist support gradually diminished, ultimately achieving independent ambulation. Participants self-paced their progression, with therapists providing minimal verbal cues and physical assistance as needed.
Quality control
The quality control system in this study covers the entire process: the design phase employs standardized protocols, randomization and blinding, and scientific sample size calculation; the implementation phase standardizes personnel training and subject management, ensuring data integrity through collection and verification; for multi-center studies, standardized operating procedures are established, with an independent committee conducting endpoint adjudication and safety monitoring; the analysis phase follows predefined statistical protocols, implements dual verification of results, and ensures full disclosure (including negative data).
Outcome measures
Baseline assessments were conducted within 7 days prior to the intervention’s initiation, with post-training evaluations completed within 7 days following the intervention’s conclusion. All outcome assessments were performed by certified and experienced physiotherapists who were blinded to group allocations. The evaluation measures included the Brunnstrom Stage, Fugl-Meyer balance function (FMB) scale, Fugl-Meyer Assessment for lower limb motor function (FMA-LE), modified Ashworth Scale (MAS), and gait patterns.
The Brunnstrom Stage classification system categorizes patients into six distinct stages based on their motor performance following a stroke: the flaccidity stage (Stage I), spasticity stage (Stage II), synergistic movement stage (Stage III), partial voluntary movement stage (Stage IV), separated movement stage (Stage V), and normal movement stage (Stage VI). Each stage, numbered from I to VI, represents a specific level of motor function, with higher stages indicating improved motor performance and recovery [21].
The FMB assessment comprises seven items, evaluating both sitting and standing postures. Each item is scored on a scale ranging from 0 to 2, where 0 indicates an inability to perform the task, 1 represents partial completion, and 2 denotes full execution [22-23].
The FMA-LE has been established as a reliable tool for assessing motor impairment, demonstrating high inter-rater and intra-rater reliability, particularly in the early post-stroke phase. This assessment consists of seven categories (reflexes, hip, knee, and ankle movements), encompassing a total of 17 subitems, with a maximum possible score of 34. Higher scores reflect superior motor function of the lower extremities [24].
The MAS was employed to evaluate muscle tone in the paretic lower limb, demonstrating moderate to excellent intra-rater reliability (κ=0.55–0.97) and moderate inter-rater reliability (κ=0.41–0.54) specifically for lower limb muscles [25-27]. The scale ranges from MAS 0, indicating no increase in muscle tone, to MAS 4, representing severe joint rigidity. Total scores were calculated for the elbow flexor, elbow extensor, wrist flexor, knee extensor, knee flexor, and ankle plantar flexor muscles in the affected upper limb.
Regarding gait pattern analysis, two qualified therapists utilized the Cortex Motion Capture System (Motion Analysis Corporation, USA) to perform three-dimensional gait analysis both before and after a four-week intervention period.
Reflective markers were positioned on anatomical bony landmarks, and participants walked a 5-meter straight path at their self-selected normal speed for 2–3 trials (Figure 3). Based on prior research and clinical expertise, key parameters for evaluating intervention efficacy were identified: (1) temporospatial parameters (velocity, step frequency, step length, and stance phase) and (2) kinematic parameters (peak hip and knee flexion angles). Therapists extracted valid gait data that met predefined criteria for further analysis [28].
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 28.0.1.0, Chicago, IL, USA). Results were considered statistically significant at P < 0.05 based on two-tailed tests. Additionally, 95% confidence intervals (CIs) were calculated to determine the range within which the true effect size was likely to exist. Categorical data were analyzed using the chi-square (χ²) test. The normality of the data and the homogeneity of variances were assessed using the Shapiro-Wilk test and Levene’s test, respectively. Depending on the data distribution, parametric tests were applied to normally distributed data, while non-parametric tests were used for non-normally distributed data. For between-group comparisons, independent t-tests were employed for parametric data, whereas Mann-Whitney U tests were utilized for non-parametric data, based on the distribution characteristics of each variable. Furthermore, paired-samples t-tests were conducted to evaluate whether significant changes occurred within each group across all outcome measures following the intervention.Cohen’s effect sizes (d) for all comparisons were classified as trivial (< 0.2), small (0.2–0.6), moderate (0.6–1.2), large (1.2–2.0), and very large (> 2.0) (Batterham & Hopkins, 2006). Statistical significance was assumed at P < 0.05 [29].
Neurophysiological basis of gait parameter improvement
The walking speed (velocity) in the experimental group increased from 16.5 cm/s to 38.44 cm/s (d=4.01), a significantly greater improvement compared with the control group (26.63 cm/s, d=2.75). This aligns with recent trends in the application of intelligent walking aids in stroke rehabilitation. For instance, Skvortsov et al. [30] found in a randomized controlled trial on subacute stroke patients that walking devices integrating inertial sensors and biofeedback could increase walking speed by up to 121%. The mechanism may stem from task-oriented training reactivating the corticospinal tract. The PAM system, by dynamically adjusting support force and synchronizing with the gait cycle, likely enhances the coupling efficiency between the motor cortex and the central pattern generator in the spinal cord. This hypothesis is further supported by the significant increase in peak hip flexion and peak knee flexion of the paretic side (d=1.82–2.17) in this study, as expanding lower limb joint range of motion requires precise regulation of multi-muscle coordination by the central nervous system. Traditional suspension training, lacking dynamic assistance, struggles to achieve such neural adaptations [31].
Additionally, the improvement in gait symmetry (reduced stance phase percentage) in the experimental group may be attributed to the assistance provided by PAM. While suspension systems reduce the psychological fear of falling, traditional training often forces patients to rely on the unaffected side for balance. The intelligent assistance module of the dynamic body weight support system, through pressure sensors, monitors real-time center of gravity shifts and dynamically adjusts support torque on the affected side, thereby reducing compensatory gait patterns [32]. This technological feature may explain the significant optimization in bilateral stance phase percentage (24.31% vs. 28.38%) and unaffected side stance phase percentage (66.19% vs. 70.13%) in the experimental group. Similarly, Meyer et al. [33] developed an intelligent weight reduction system that improved gait symmetry by 37% in stroke patients by adjusting harness tension vectors, a mechanism highly consistent with the findings of this study.
Potential mechanisms of spasticity prevention and control
The significant increase in MAS scores in the control group (d=1.48) highlights the limitations of traditional suspension training: while it reduces fall risk, the lack of correction for abnormal movement patterns may exacerbate spasticity. In contrast, the experimental group showed only a slight increase in MAS scores (d=0.15), suggesting PAM intervention may suppress spasticity through two mechanisms. First, real-time tactile and visual feedback reinforces the cortical representation of correct movement patterns, inhibiting abnormal excitability of spinal α-motor neurons. Second, adaptive gait training coordinates the activation timing of agonist and antagonist muscles, reducing tension imbalance caused by muscle synergy dysfunction [34]. For example, the increase in peak hip flexion of the paretic side (d=2.17) may result from enhanced co-activation of the iliopsoas and rectus femoris, alongside reduced co-contraction of the quadriceps and hamstrings, thereby minimizing tension conflict between flexor and extensor muscle groups [35].These findings align with recent neuromodulation research on spasticity intervention. Xu et al. [36] suggest that task-specific training, as demonstrated by repetitive transcranial magnetic stimulation, can suppress spasticity-related synaptic plasticity abnormalities by upregulating GABAergic interneuron activity. The repetitive gait cycles in PAM training may enhance cortical inhibitory control through a similar mechanism, delaying or mitigating spasticity progression. Additionally, the precise control of gait cycles by intelligent walking aids may reduce mechanical stretching of muscles caused by abnormal patterns like foot inversion or circumduction, which are known triggers of post-stroke spasticity [37].
Advantages of early intervention time window
This study selected the early stage (within 4 weeks post-stroke) as the intervention window, based on the critical period theory of neuroplasticity. In the acute phase post-stroke, the peri-infarct penumbra contains numerous dormant neurons, with synaptic remodeling capacity peaking within 2–6 weeks after onset. PAM training, through high-intensity repetitive task stimulation, may accelerate the reorganization of motor pathways during this phase [38]. For example, in the experimental group, the step frequency increased from 46.44 steps/min to 64.94 steps/min (d=2.32), reflecting rapid improvement in the central nervous system’s ability to regulate gait rhythm, likely due to early remodeling of cerebellar-brainstem pathways [39]. In contrast, gait training in chronic patients often relies on peripheral adaptation rather than central reorganization, limiting its efficacy [40].
Additionally, the protective effects of early intervention on muscle structure cannot be overlooked. Within 2 weeks post-stroke, the cross-sectional area of affected lower limb muscles can decrease by up to 30%, and the shift toward fast-twitch (Type II) fibers further increases spasticity risk [41]. PAM training, by providing moderate load stimulation, may delay muscle atrophy and promote the preservation of slow-twitch (Type I) fibers. The significant increase in peak knee flexion (d=1.82) in the experimental group may partly result from maintained eccentric contraction capacity of the quadriceps, closely related to the functional integrity of slow-twitch fibers [42].
Limitations and future research directions
While this study highlights the potential value of PAM training, several limitations should be noted. First, the small sample size (n=32) may affect statistical power, particularly for highly variable metrics like MAS scores. Second, the 4-week intervention period limits the assessment of long-term efficacy and the durability of spasticity prevention and control. Third, the study did not employ neuroimaging or neurophysiological measures (e.g., motor evoked potentials) to explore central remodeling mechanisms. Future research could address these limitations by conducting multicenter, large-sample cohort studies with extended follow-up periods, incorporating techniques such as diffusion tensor imaging or functional near-infrared spectroscopy to analyze neuroplasticity changes [43].
Additionally, the personalized adaptation of PAM technology requires further optimization. While the current system adjusts support based on body weight, it does not account for individualized gait characteristics (e.g., step width, foot angle). Integrating machine learning algorithms to develop personalized assistance models may represent the next breakthrough in this field [35]. Finally, economic costs and device accessibility may hinder clinical adoption, necessitating further health economic evaluations to clarify its cost-effectiveness ratio [44].
Clinical implications
The findings of this study provide significant guidance for stroke rehabilitation practice. First, early intervention (within 4 weeks post-stroke) with intelligent walking aids can significantly improve walking ability and suppress spasticity progression, suggesting its inclusion in acute-phase rehabilitation protocols. Second, the combination of suspension protection and intelligent assistance effectively balances safety (reducing falls) and training intensity (inducing neural adaptation), making it particularly suitable for patients with moderate dysfunction (muscle strength grades 2–3). Third, clinical teams should closely monitor early warning signs of spasticity (e.g., rapid increase in MAS scores) and promptly adjust treatment plans to prevent abnormal movement patterns from becoming entrenched.
Conclusion
This study shows that early gait training using the PAM under the SPS improves walking ability in stroke patients and reduces muscle spasticity by optimizing movement patterns. These benefits may come from combined nervous system adaptations, including renewed brain-spinal cord connections, better muscle coordination, and regulation of abnormal muscle activity. Future research should confirm long-term effects and mechanisms through larger studies and advanced assessments, helping advance personalized, tech-driven stroke rehabilitation.
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
偏瘫是常见的与脑脑卒中相关的病症,其运动功能障碍方面的问题常被研究,但痉挛方面却研究不足。异常的肌肉张力极大地阻碍了偏瘫患者行走功能的恢复。#br# 中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程#br#
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||