[1] PAVELKA K. Osteonecrosis. Baillieres Best Pract Res Clin Rheumatol. 2000;14(2):399-414.
[2] HUANG C, QING L, XIAO Y, et al. Insight into Steroid-Induced ONFH: The Molecular Mechanism and Function of Epigenetic Modification in Mesenchymal Stem Cells. Biomolecules. 2023;14(1):4.
[3] WANG X, CHEN X, LU L, et al. Alcoholism and Osteoimmunology. Curr Med Chem. 2021;28(9):1815-1828.
[4] KUBO Y, DRESCHER W, FRAGOULIS A, et al. Adverse Effects of Oxidative Stress on Bone and Vasculature in Corticosteroid-Associated Osteonecrosis: Potential Role of Nuclear Factor Erythroid 2-Related Factor 2 in Cytoprotection. Antioxid Redox Signal. 2021;35(5):357-376.
[5] SHI W, ZHANG X, XU C, et al. Identification of Hub Genes and Pathways Associated with Oxidative Stress of Cartilage in Osteonecrosis of Femoral Head Using Bioinformatics Analysis. Cartilage. 2022;13(1):19476035221074000.
[6] CHANG C, GREENSPAN A, GERSHWIN ME. The pathogenesis, diagnosis and clinical manifestations of steroid-induced osteonecrosis. J Autoimmun. 2020;110:102460.
[7] BAEK SH, KIM KH, LEE WK, et al. Abnormal Lipid Profiles in Nontraumatic Osteonecrosis of the Femoral Head: A Comparison with Osteoarthritis Using Propensity Score Matching. J Bone Joint Surg Am. 2022; 104(Suppl 2):19-24.
[8] LIAO Z, JIN Y, CHU Y, et al. Single-cell transcriptome analysis reveals aberrant stromal cells and heterogeneous endothelial cells in alcohol-induced osteonecrosis of the femoral head. Commun Biol. 2022;5(1):324.
[9] HSU SH, JANG MH, TORNG PL, et al. Positive Association Between Small Dense Low-Density Lipoprotein Cholesterol Concentration and Biomarkers of Inflammation, Thrombosis, and Prediabetes in Non-Diabetic Adults. J Atheroscler Thromb. 2019;26(7):624-635.
[10] LEUTI A, MACCARRONE M, CHIURCHIÙ V. Proresolving Lipid Mediators: Endogenous Modulators of Oxidative Stress. Oxid Med Cell Longev. 2019;2019:8107265.
[11] YANG W, YIN H, WANG Y, et al. New insights into effects of Kaixin Powder on depression via lipid metabolism related adiponectin signaling pathway. Chin Herb Med. 2023; 15(2):240-250.
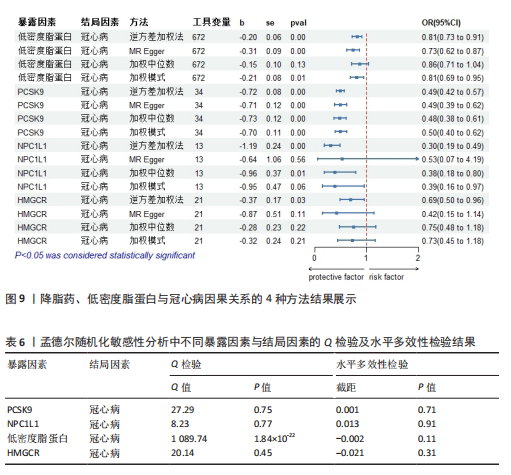
[12] FINCH ER, PAYTON MA, JENKINS DA, et al. Fenofibrate reduces osteonecrosis without affecting antileukemic efficacy in dexamethasone-treated mice. Haematologica. 2021;106(8):2095-2101.
[13] KANG P, GAO H, PEI F, et al. Effects of an anticoagulant and a lipid-lowering agent on the prevention of steroid-induced osteonecrosis in rabbits. Int J Exp Pathol. 2010;91(3):235-243.
[14] ZHENG H, YE B, HUANG K, et al. Laboratory indices in patients with osteonecrosis of the femoral head: a retrospective comparative study. J Orthop Surg Res. 2023;18(1):750.
[15] ZHAO SS, YIU ZZN, BARTON A, et al. Association of Lipid-Lowering Drugs With Risk of Psoriasis: A Mendelian Randomization Study. JAMA Dermatol. 2023;159(3):275-280.
[16] BIRNEY E. Mendelian Randomization. Cold Spring Harb Perspect Med. 2022;12(4): a041302.
[17] ISTVAN ES. Structural mechanism for statin inhibition of 3-hydroxy-3-methylglutaryl coenzyme A reductase. Am Heart J. 2002; 144(6 Suppl):S27-32.
[18] SABATINE MS. PCSK9 inhibitors: clinical evidence and implementation. Nat Rev Cardiol. 2019;16(3):155-165.
[19] WILLIAMS DM, FINAN C, SCHMIDT AF, et al. Lipid lowering and Alzheimer disease risk: A mendelian randomization study. Ann Neurol. 2020;87(1):30-39.
[20] GRAHAM SE, CLARKE SL, WU KH, et al. The power of genetic diversity in genome-wide association studies of lipids. Nature. 2021;600(7890):675-679.
[21] ZUBER V, GRINBERG NF, GILL D, et al. Combining evidence from Mendelian randomization and colocalization: Review and comparison of approaches. Am J Hum Genet. 2022;109(5):767-782.
[22] LIN J, ZHOU J, XU Y. Potential drug targets for multiple sclerosis identified through Mendelian randomization analysis. Brain. 2023;146(8):3364-3372.
[23] HUANG J, ZHAO X, LI X, et al. HMGCR inhibition stabilizes the glycolytic enzyme PKM2 to support the growth of renal cell carcinoma. PLoS Biol. 2021; 19(4):e3001197.
[24] DAY EA, FORD RJ, SMITH BK, et al. Salsalate reduces atherosclerosis through AMPKβ1 in mice. Mol Metab. 2021;53:101321.
[25] LI X, SHEN H, ZHANG M, et al. Glycolytic reprogramming in macrophages and MSCs during inflammation. Front Immunol. 2023; 14:1199751.
[26] REN Z, ZHOU L. Association of statin use with osteoporosis risk: a drug-targeted Mendelian randomization study. Inflammopharmacology. 2024;32(2):1253-1261.
[27] 卿尚兰,徐诣芝.他汀类药物作用于牙槽骨的研究进展[J].检验医学与临床, 2022,19(4):564-566+573.
[28] 武扬,李丽.阿托伐他汀对牙周炎大鼠的影响及可能机制[J].长春中医药大学学 报,2023,39(10):1101-1105.
[29] WANG XY, MA TL, CHEN KN, et al. Accumulation of LDL/ox-LDL in the necrotic region participates in osteonecrosis of the femoral head: a pathological and in vitro study. Lipids Health Dis. 2021;20(1):167.
[30] WANG L, LI S, LUO H, et al. PCSK9 promotes the progression and metastasis of colon cancer cells through regulation of EMT and PI3K/AKT signaling in tumor cells and phenotypic polarization of macrophages. J Exp Clin Cancer Res. 2022;41(1):303.
[31] KÖNIGSBRÜGGE O, SCHMALDIENST S, AUINGER M, et al. Antithrombotic agents for primary and secondary prevention of cardiovascular events in patients with end-stage renal disease on chronic hemodialysis. Atherosclerosis. 2020;298:1-6.
[32] KIM YU, KEE P, DANILA D, et al. A Critical Role of PCSK9 in Mediating IL-17-Producing T Cell Responses in Hyperlipidemia. Immune Netw. 2019;19(6):e41.
[33] PIRILLO A, CATAPANO AL, NORATA GD. Niemann-Pick C1-Like 1 (NPC1L1) Inhibition and Cardiovascular Diseases. Curr Med Chem. 2016;23(10):983-999.
[34] TANG Z, JIANG L, PENG J, et al. PCSK9 siRNA suppresses the inflammatory response induced by oxLDL through inhibition of NF-κB activation in THP-1-derived macrophages. Int J Mol Med. 2012;30(4):931-938.
[35] FERENCE BA, ROBINSON JG, BROOK RD, et al. Variation in PCSK9 and HMGCR and Risk of Cardiovascular Disease and Diabetes. N Engl J Med. 2016;375(22):2144-2153.
[36] CAO K, ZHANG K, MA M, et al. Lactobacillus mediates the expression of NPC1L1, CYP7A1, and ABCG5 genes to regulate cholesterol. Food Sci Nutr. 2021;9(12):6882-6891.
[37] ZHANG Z, QIN S, CHEN Y, et al. Inhibition of NPC1L1 disrupts adaptive responses of drug-tolerant persister cells to chemotherapy. EMBO Mol Med. 2022;14(2):e14903.
[38] HAYCOCK PC, BURGESS S, WADE KH, et al. Best (but oft-forgotten) practices: the design, analysis, and interpretation of Mendelian randomization studies. Am J Clin Nutr. 2016;103(4):965-978.
[39] GILL D, GEORGAKIS MK, WALKER VM, et al. Mendelian randomization for studying the effects of perturbing drug targets. Wellcome Open Res. 2021;6:16.
|