中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (19): 3061-3068.doi: 10.12307/2024.162
• 细胞相关实验/试验研究Cell related experimental/trial studies • 上一篇 下一篇
基于子宫内膜结构与子宫螺旋动脉血流参数构建人工授精妊娠预测模型及验证
庾广聿1,范嘉琪1,陈施蓓1,高磊磊2,余 晴1,周 超1,于春梅3,金 珍4
- 1广西壮族自治区南溪山医院辅助生殖科,广西壮族自治区桂林市 541002;浙江省人民医院,2妇科,4生殖内分泌科,浙江省杭州市 310000;3常州市妇幼保健院生殖中心,江苏省常州市 213000
Construction and validation of pregnancy prediction model of artificial insemination by husband based on endometrial structure and uterine spiral artery blood flow parameters
Yu Guangyu1, Fan Jiaqi1, Chen Shibei1, Gao Leilei2, Yu Qing1, Zhou Chao1, Yu Chunmei3, Jin Zhen4
- 1Department of Assisted Reproductive Medicine, Nanxishan Hospital of Guangxi Zhuang Autonomous Region, Guilin 541002, Guangxi Zhuang Autonomous Region, China; 2Department of Obstetrics and Gynecology, 4Department of Reproductive Endocrinology, Zhejiang Provincial People’s Hospital, Hangzhou 310000, Zhejiang Province, China; 3Reproductive Center, Changzhou Maternal and Child Health Hospital, Changzhou 213000, Jiangsu Province, China
摘要:

文题释义:
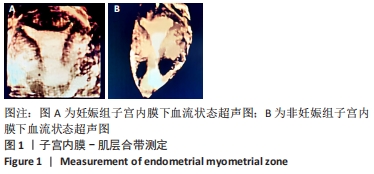
夫精宫腔内人工授精:是指在女方排卵前后12 h内,将丈夫的精液经洗涤处理,去除精浆及精液中的死精子、白细胞、抗体等成分后,将优选出质量好的精液注入女方宫腔内的一种方法。该方法可以提高精子的密度和活力,相对提高怀孕的概率。但目前夫精宫腔内人工授精的成功率为10%-15%。子宫肌层内层平均交界区测定:启动阴道超声三维超声检查模式,通过借助容积对比成像软件,对多平面图像进行操作,获得较为满意的子宫外部轮廓和宫腔冠状面图像。采用容积对比成像技术(设定层厚2 mm)完成成像的渲染,将三维成像数据存储在仪器中,可测出从基底子宫内膜到外子宫肌层内层平均交界区和最大交界区厚度水平。
背景:现子宫内膜结构及子宫螺旋动脉血流参数对夫精宫腔内人工授精(artificial insemination by husband,AIH)妊娠率的影响水平尚不明确,该研究通过校准其他混杂因素后,确定了其独立影响因素,并构建了预测模型,具有较好的临床应用效能。
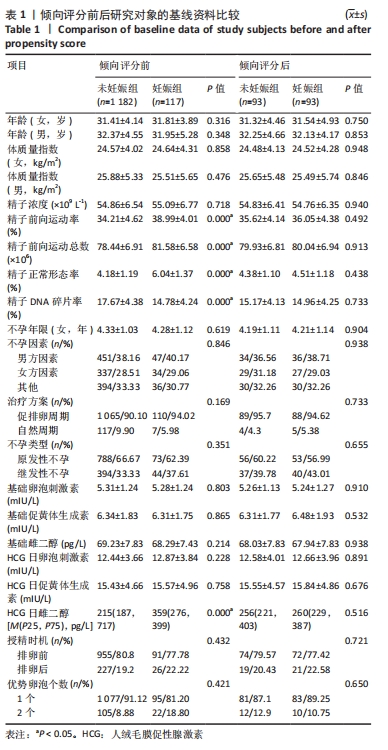
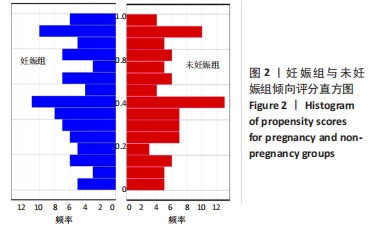
目的:基于子宫内膜结构及子宫螺旋动脉血流参数构建AIH临床妊娠预测模型及验证。方法:回顾性分析2017年1月至2021年1月于常州市妇幼保健院接受AIH助孕治疗患者共1 299例,将其中1 182例未临床妊娠者纳入未妊娠组,117例临床妊娠者纳入妊娠组;通过1∶1倾向评分匹配,妊娠组与未妊娠组各匹配成功93例;采用单、多因素分析筛选子宫内膜结构及子宫螺旋动脉血流参数对AIH结局的影响因素,通过受试者工作曲线确定各独立影响因素的最佳截断值,限制性立方样条法分析各独立影响因素对AIH妊娠影响的风险趋势,临床决策曲线与临床影响曲线对该联合预测模型的临床应用效能进行检验。
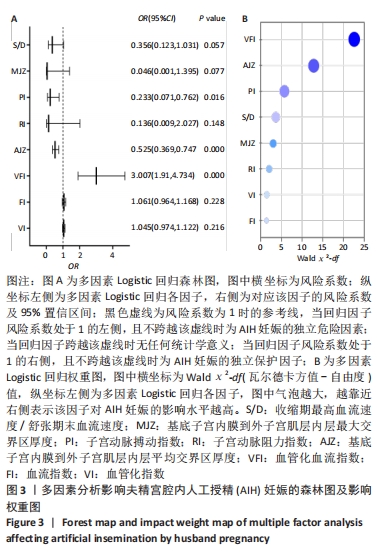
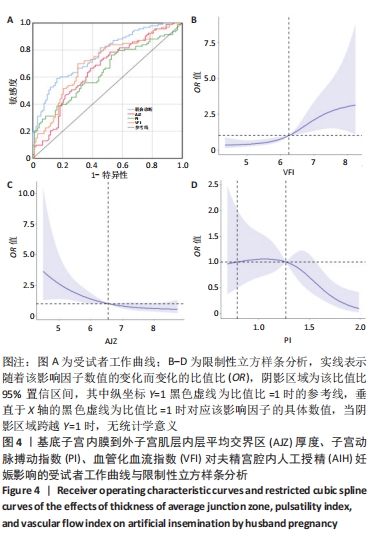
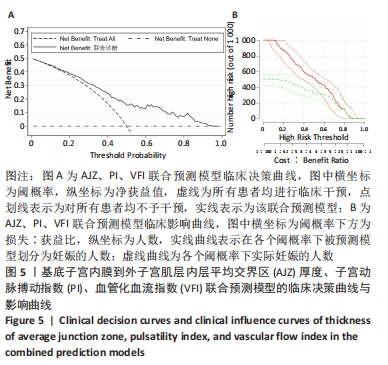
结果与结论:①倾向评分后妊娠组与未妊娠组各非内膜因素均无显著统计学意义,数据具有较好的均衡性(P > 0.05);②单因素分析结果显示,内膜下血管化指数、血流指数、血管化血流指数、子宫动脉阻力指数、子宫动脉搏动指数、收缩期最高血流速度/舒张期末血流速度、基底子宫内膜到外子宫肌层内层平均交界区、最大交界区厚度为AIH妊娠的影响因素(P < 0.05);③多因素Logistic回归结果显示,基底子宫内膜到外子宫肌层内层平均交界区厚度、子宫动脉搏动指数、血管化血流指数为AIH妊娠的独立影响因素,影响大小依次为血管化血流指数>基底子宫内膜到外子宫肌层内层平均交界区厚度>子宫动脉搏动指数;④受试者工作曲线显示,血管化血流指数的曲线下面积为0.704(0.629,0.779),最佳截断值为6.26;基底子宫内膜到外子宫肌层内层平均交界区厚度的曲线下面积为0.660(0.582,0.739),最佳截断值为6.38;子宫动脉搏动指数的曲线下面积为0.642(0.563,0.721),最佳截断值为1.18;⑤限制性立方样条曲线显示,当血管化血流指数> 6.24时,其对AIH妊娠具有显著的正影响趋势;基底子宫内膜到外子宫肌层内层平均交界区厚度≤6.55 mm时,其对AIH妊娠具有显著的正影响趋势;当子宫动脉搏动指数> 1.27时,其对AIH妊娠具有负影响风险;⑥临床决策曲线与临床影响曲线显示,该联合预测模型在阈概率值为0.17-0.93时具有临床最大净获益,且在该阈概率范围内损失与获益的比值始终小于1,显示出该联合预测模型具有较好的临床效能;⑦结果表明,通过倾向评分与多因素Logistic回归校正子宫内膜外其他混杂因素后,基底子宫内膜到外子宫肌层内层平均交界区厚度、子宫动脉搏动指数、血管化血流指数为AIH妊娠的独立影响因素,通过对其最佳截断值的确定与风险趋势性评估,证实该联合预测模型具有较好的预测价值与临床应用效能。
https://orcid.org/0009-0006-1485-1457 (庾广聿)
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
中图分类号: