| [1] Kalfas IH. Role of corpectomy in cervical spondylosis. Neurosurg Focus. 2002;12:E11.
[2] Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion?. Spine J. 2004;4(6): S190-S194.
[3] Levin DA, Hale JJ, Bendo JA. Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis. 2007;65(1):29-36.
[4] Zigler J, Delamarter R, Spivak JM, et al. Results of the prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc®-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine. 2007;32(11): 1155-1162.
[5] Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and Myelopathy at Segments Adjacent to the Site of a Previous Anterior Cervical Arthrodesis. J Bone Joint Surg. 1999;81(4): 519-528.
[6] Jiang SD, Jiang LS, Dai LY. Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for multilevel cervical spondylosis: a systematic review. Arch Orthop Trauma Surg. 2012;132(2): 155-161.
[7] Mummaneni PV, Haid RW. The future in the care of the cervical spine: interbody fusion and arthroplasty: Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1(2): 155-159.
[8] 李忠海,侯树勋,吴闻文,等.颈椎动态稳定器治疗颈椎病的早期疗效观察[J].中华外科杂志, 2013,51(8):761-763.
[9] 李忠海,侯树勋,吴闻文,等.单节段颈椎动态稳定器植入术对颈椎曲度和活动度的影响[J].中国骨与关节杂志,2013, 2(10): 574-579.
[10] Li Z, Yu S, Zhao Y, et al. Clinical and radiologic comparison of dynamic cervical implant arthroplasty versus anterior cervical discectomy and fusion for the treatment of cervical degenerative disc disease. J Clin Neurosci. 2014;21(6): 942-948.
[11] Ishihara H, Kanamori M, Kawaguchi Y, et al. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004; 4(6):624-628.
[12] Gao Y, Liu M, Li T, et al. A meta-analysis comparing the results of cervical disc arthroplasty with anterior cervical discectomy and fusion (ACDF) for the treatment of symptomatic cervical disc disease. J Bone Joint Surg Am. 2013;95(6):555-561.
[13] Kushagra V, Spapn DG, Mitchell M, et al. The rate of adjacent segment disease in cervical disc arthroplasty versus single level fusion: a meta-analysis of prospective studies. Spine. 2013;15;38(26):2253-2257.
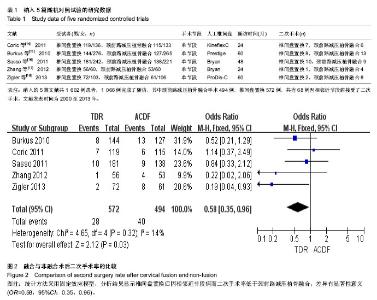
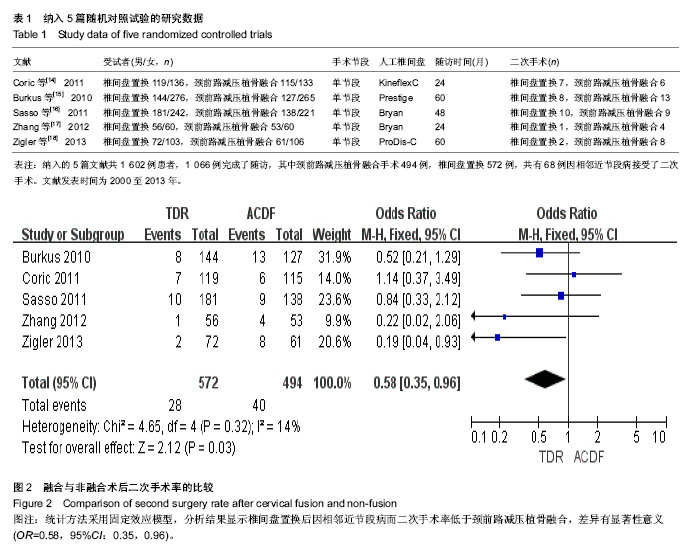
[14] Coric D, Nunley PD, Guyer RD, et al. Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article.J Neurosurg Spine. 2011;15(4):348-358.
[15] Burkus JK, Haid RW, Traynelis VC, et al.Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial.J Neurosurg Spine. 2010;13(3): 308-318.
[16] Sasso RC, Anderson PA, Riew KD, et al.Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011;93(18): 1684-1692.
[17] Zhang X, Zhang X, Chen C, et al.Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China.Spine. 2012;37(6):433-438.
[18] Zigler JE, Delamarter R, Murrey D, et al. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine. 2013;38(3):203-209.
[19] Nabhan A, Ahlhelm F, Shariat K, et al. The ProDisc-C prothesis: clinical and radiological experience 1 year after surgery. Spine. 2007;32(18): 1935-1941.
[20] Porchet F, Metcalf NH. Clinical outcomes with the Prestige II cervical disc: preliminary results from a prospective randomized clinical trial. Neurosurgical Focus. 2004;17(3): 1-43.
[21] Fallah A, Akl EA, Ebrahim S, et al. Anterior cervical discectomy with arthroplasty versus arthrodesis for single-level cervical spondylosis: a systematic review and meta-analysis. PLoS One. 2012;7(8):e43407.
[22] Yin S, Yu X, Zhou S, et al. Is cervical disc arthroplasty superior to fusion for treatment of symptomatic cervical disc disease? A meta-analysis. Clin Orthop Relat Res. 2013; 471(6): 1904-1919.
[23] Jiang H, Zhu Z, Qiu Y, et al. Cervical disc arthroplasty versus fusion for single-level symptomatic cervical disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. 2012;132(2):141-151.
[24] Boselie TF, Willems PC, van Mameren H, et al. Arthroplasty versus fusion in single-level cervical degenerative disc disease. Cochrane Database Syst Rev. 2012;9:CD009173.
[25] Hou Y, Liu Y, Yuan W, et al. Cervical kinematics and radiological changes after Discover artificial disc replacement versus fusion. Spine J. 2014;14(6):867-877.
[26] Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002; 27(22): 2431-2434.
[27] Katsuura A, Hukuda S, Saruhashi Y, et al. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10(4): 320-324.
[28] Takeshima T, Omokawa S, Takaoka T, et al. Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine. 2002;27(15): E348-355.
[29] Song KJ, Choi BW, Jeon TS, et al. Adjacent Segment Degenerative Disease: Is It Due to Disease Progression or a Fusion-Associated Phenomenon? Eur Spine J. 2011;20(11): 1940-1945. |