| [1] Cheh G,Bridwell KH,Lenke LG,et al.Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up.Spine (Phila Pa 1976).2007;32(20):2253-2257.
[2] Gillet P.The fate of the adjacent motion segments after lmbar fusion. J Spinal Disord Tech.2003;16:338-345.
[3] Throckmorton TW,Hilibrand AS,Mencio GA,et al.The impact of adjacent level disc degeneration on health status outcomes following lumbar fusion.Spine. 2003; 28:2546-2550.
[4] Frymoyer JW,Hanley EN Jr,Howe J,et al.A comparison of radiographic ?ndings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine.1979;4:435-440.
[5] Kumar MN,Jacquot F,Hall H.Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine surgery for degenerative disc disease.Eur Spine J.2001;10:209-313.
[6] Whitecloud TSI,Davis JM,Olive PM.Operative treatment of the degenerated segment adjacent to a lumbar fusion.Spine.1994;19:531-536.
[7] Penta M,Sandhu A,Fraser RD.Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion.Spine.1995;20:743-747.
[8] Javedan SP,Dickman CA.Cause of adjacent-segment disease after spinal fusion. Lancet.1999;354:530-531.
[9] Gruber HE,Gordon B,Williams C.A new small animal model for the study of spine fusion in the sand rat: pilot studies.Laboratory Animals.2009;43:272-277.
[10] Adelt D,Samani J,Kim WK.Coflex interspinous stabilization: clinical and radiographic results from an internationa1 muhicenter retrospective study.Paradigm Spine.2007;1(2):25-31.
[11] Alexander R,Christian S,Michael H,et al.Does an interspinous device (Co?exTM) improve the outcomeof decompressive surgery in lumbar spinal stenosis? One-yearfollow up of a prospective case control study of 60 patients.Eur Spine.2010;19:283-289.
[12] Frank T,Gary L,Nicholas D,et al Determination of the in vivo posterior loading environment of the Coflex interlaminar-interspinous implant.Spine.2010;10: 244-252.
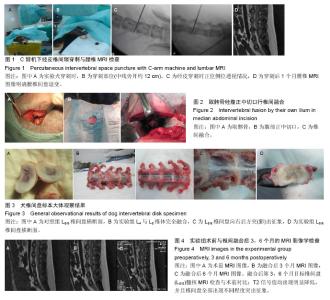
[13] 彭俊,徐建广.犬椎间盘经皮针刺退变模型的建立[J].中国组织工程研究,2012,16(24): 4463-4466.
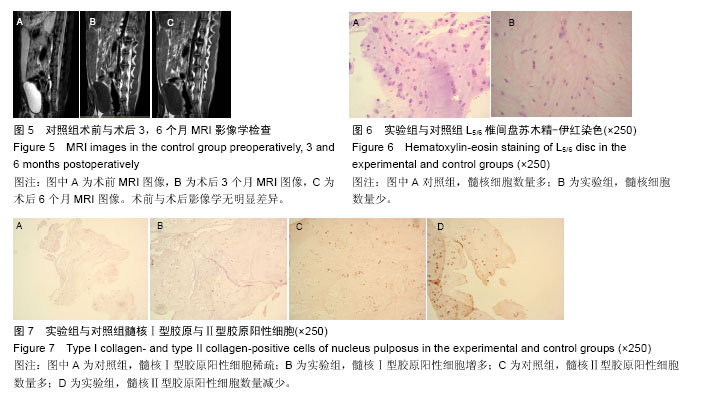
[14] Videman T,Nummi P,Battie MC,et al.Digital assessment of MRI for lumbar disc desiccation:a comparison of digital versus subjective assessments and digital intensity profiles versus discogram and macroanatomic findings.Spine.1994;19:192-198.
[15] Arai Takahashi M,Kurosawa H.Compative s tudy of iliac bonegraft and carbon cage with local bone graft in pos terior lumbar interbodyfus ion.J Orthop Surg(Hong Kong).2002;10(1):1-7.
[16] Phillips FM,Reuben J,Wetzel FT.Intervertebral disc generaion adiacent to a lumbar fusion.An experimental rabbit model.J bone Joint Surg Br.2002;84(2):289-294.
[17] Chen SN,Chen CK,Liu CL,et al.Stress analysis of the disc adjacent to interbody fusion in lumbar spine.Med Eng Phys.2001;23(7):483-491.
[18] Khan SN,Lane JM.Spianl fusion surgery: animal model for tissue-engineered bone constructs.Biomaterial. 2004; 25(9):1475-1485.
[19] Eck JC,Humphreys SC,Lim TH,et al.Biomechanical study on the effect of cervical spine fusion on adjacent 2 level intradiscal pressure and segmental motion. Spine.2002;27(22):2431-2434.
[20] Kumar MN,Baklanov A,Chopin D.Correlation between sagittal plane changes and adjacent segment degeneration follwing lumbar spine fusion.Eur Spine. 2001;10(4):314-319.
[21] Lipson SJ,Muir H.1980 Volvo award in basic science: proteoglycans in experimental intervertebral disc degenernation.Spine.1981;6(3):194-210.
[22] Singh K,Masuda K,An HS.Animal models for human disc degeneration.Spine J.2005;5:267s-229s.
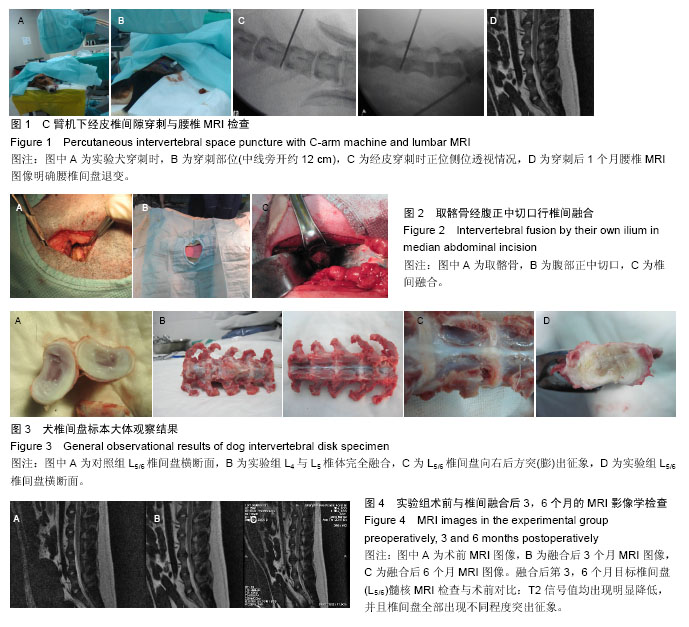
[23] 黄丽洁,苟鹏,贾琳,等.犬腰椎椎间融合手术入路的比较[J].中国实验动物学报,2004,12(2):114-116.
[24] Weidinbaum J,Foster RJ,Best BA,et al.Correlating MRI with the bioc hemical content of the normal human intervertabral disc.J Orthop Res.1992;10:552-561.
[25] Chatani M,Matayoshi Y,Masaki N,et al.Radiation therapy of the nasopharyngeal carcinoma. Treatment results and prognostic factors.Strahlenther Onkol. 1993;169(9):527-533. |