Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (30): 6547-6555.doi: 10.12307/2025.952
Previous Articles Next Articles
Local application of osteoporosis treatment drugs in oral field
Ma Ling, Zhang Zhao
- Department of Prosthodontics, School of Stomatology-Hospital of Stomatology, Hebei Medical University, Hebei Key Laboratory of Stomatology, Hebei Oral Health Technology Innovation Center, Shijiazhuang 050017, Hebei Province, China
-
Received:2024-10-16Accepted:2024-12-17Online:2025-10-28Published:2025-03-29 -
Contact:Zhang Zhao, MD, Associate chief physician, Department of Prosthodontics, School of Stomatology-Hospital of Stomatology, Hebei Medical University, Hebei Key Laboratory of Stomatology, Hebei Oral Health Technology Innovation Center, Shijiazhuang 050017, Hebei Province, China -
About author:Ma Ling, Master candidate, Physician, Department of Prosthodontics, School of Stomatology-Hospital of Stomatology, Hebei Medical University, Hebei Key Laboratory of Stomatology, Hebei Oral Health Technology Innovation Center, Shijiazhuang 050017, Hebei Province, China -
Supported by:Research Project on Prevention and Treatment of Geriatric Diseases of the Department of Finance of Hebei Province, No. 361029 (to ZZ); Leader of the 2020 Government-funded Excellent Talent Training Project in Clinical Medicine of Department of Finance of Hebei Province, No. 2020048149-2 (to ZZ); Directive Project of Medical Science Research Project Plan of Health Commission of Hebei Province, No. 20190098 (to ZZ)
CLC Number:
Cite this article
Ma Ling, Zhang Zhao. Local application of osteoporosis treatment drugs in oral field[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6547-6555.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

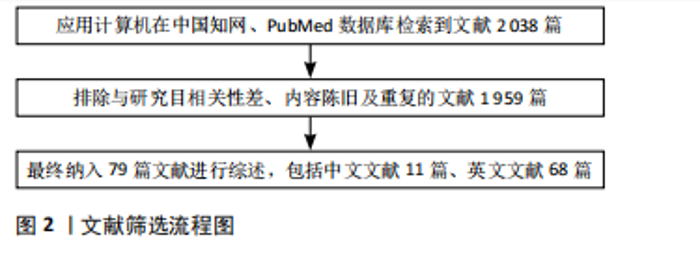
功的关键,初期稳定性是种植体骨整合的主要决定因素。 2.1.1 双膦酸盐类 在骨-种植体界面局部给予双膦酸盐类药物有2种主要方法[6],即通过涂层或固定技术直接从种植体表面给药,或使用载体将药物局部递送于植入部位。多项实验研究表明,双膦酸盐类药物局部小剂量应用能够有效促进牙种植体表面成骨,降低种植体周围骨丢失率,有利于提高种植体的稳定性[7-12]。ABTAHI等[11]发现含有极少量双膦酸盐(帕米磷酸盐和伊班磷酸盐,约216 ng/cm2)的纳米薄纤维蛋白原涂层可改善早期种植体固定,在功能负荷后5年仍保持其效果,但在吸收活性增加的情况下,例如在不稳定的植入物周围,效果较小,这可能与双膦酸盐的剂量依赖性有关。有研究通过有限元分析方法发现唑来膦酸作为种植体表面涂层能够改善种植体的固定,且仅对种植体周围的骨骼有影响,这减少了双膦酸盐全身应用可能产生的不良反应[13]。然而,JAHAN等[14]将种植体浸入阿仑膦酸钠溶液(20 mg/mL)并用相同溶液冲洗种植窝洞后虽然显示出牙槽嵴骨质流失量减少,但差异没有统计学意义。AL-ASSAF等[15]在种植窝洞内加入阿仑膦酸钠凝胶(含阿仑膦酸钠100 μg/种植窝洞)后,与对照组相比,种植体稳定性有相似的变化模式,并且种植体稳定性取决于愈合时间,组间没有显著差异。最近的一项多中心、双盲、随机对照研究结果显示,唑来膦酸涂层种植体(0.7 μg/种植体)与无涂层种植体相比,从基线到 12 周时的种植体稳定性指数没有显著差异[16],负载1年后两组种植体边缘骨吸收值没有显著差异,这可能与研究对象为全身健康人群有关,种植体植入后的初始稳定性即保持在较高水平;另外还可能与唑来膦酸涂层释放的唑来膦酸剂量有关,需要进一步研究。值得一提的是,上述研究中均没有观察到任何严重的不良反应。未来还需进行更大样本量的试验来评估双膦酸盐局部应用后的长期安全性,进一步探索用药剂量,有望将双膦酸盐类药物负载在种植体表面,局部小剂量控制药物释放,以期在减少药物不良反应的前提下促进骨整合和种植体固定。 2.1.2 他汀类药物 他汀类药物是高脂血症的有效治疗药物,局部应用他汀类药物可以增强骨整合,在限制种植体周围骨吸收方面显示出有希望的效果[17-18]。辛伐他汀是一种常用的他汀类药物,研究发现辛伐他汀可通过增加骨形态发生蛋白2基因表达促进成骨细胞的增殖,还能通过抑制破骨细胞膜上胆固醇的产生来抑制破骨细胞的形成[19]。MANSOUR等[20]将辛伐他汀颗粒(2.2 mg)连同种植体一起植入犬下颌第三磨牙拔牙窝内,发现辛伐他汀颗粒促进了种植体周围成骨,有利于种植体的骨整合。然而局部应用他汀类药物对种植体的影响大多选用胫骨,大鼠胫骨与人类牙槽骨的结构不同,人类口腔内的微生物菌群比大鼠胫骨更复杂,并且在大鼠胫骨模型中无法再现人类植入物周围的咬合力。开发用于种植体的辛伐他汀表面改性策略对于评估辛伐他汀的局部递送方法具有重要意义。 2.1.3 地诺单抗 随着种植牙手术的指数级增长,种植体周围炎已经变得普遍,表现为种植体周围软组织感染和骨质流失,最终导致种植体失败。有研究发现,局部牙龈注射抗RANKL抗体可以减少种植体周围炎小鼠的骨质流失,并且协同抗炎治疗可能增强这种作用,结合抗炎治疗方案可能是改善种植体周围骨质流失的更有效策略[21]。 2.1.4 甲状旁腺激素 当以低剂量间歇性给药时,甲状旁腺激素可能会刺激皮质和小梁骨生长,聚乙二醇可以用作种植牙体中引导骨再生技术的屏障膜,有研究表明含有甲状旁腺激素肽(1-34)的精氨酸-甘氨酸-天冬氨酸修饰的聚乙二醇水凝胶是获得骨再生的有效基质系统,可明显促进犬牙种植体周围新骨形成,能够实现骨再生[22]。 VALDERRAMA等[23]研究表明甲状旁腺激素(1-34)与精氨酸-甘氨酸-天冬氨酸修饰的聚乙二醇水凝胶结合的效果仅能略微改善犬牙种植体周围缺损处的骨形成。孙智慧等[24]发现局部应用重组人甲状旁腺激素(1-34)能够促进早期种植体周围新骨形成,提高种植体-骨界面结合强度,增强种植体稳定性。 上述4种药物局部应用于种植体似乎能提高种植体的稳定性,见表1,然而这些结果是否能够在人类临床环境中产生长期影响尚不明确,未来需进行样本量更大的实验以进一步探索这些药物局部应用的最佳剂量、应用方式,以及药物局部应用于种植体的类型及促进骨整合的机制等。 2.2 牙周炎方面 牙周炎主要是由牙菌斑生物膜引起的慢性感染性疾病,会导致牙周支持组织的破坏,是成年人牙齿缺失的主要原因。 2.2.1 双膦酸盐类药物 局部应用双膦酸盐可有效阻断牙槽骨吸收,作为龈下刮治和根面平整术的辅助治疗手段,可增强对实验性牙周炎大鼠的疗效[25],双膦酸盐的局部递送对患有慢性牙周炎以及患有牙周炎的吸烟患者、2型糖尿病和慢性胰腺炎患者的治疗效果均有改善作用[26-29],并且比口服给药更有效[30]。将1%阿仑膦酸钠局部递送至Ⅱ级根分叉缺损位置对骨再生同样有积极作用[31]。另外,由于富血小板纤维蛋白有助于介导骨再生和软组织成熟,KANORIYA等[32]发现富血小板纤维蛋白+1%阿仑膦酸盐联合应用于慢性牙周炎患者的骨缺损治疗,可显著改善临床及放射学参数,这一结果说明富血小板纤维蛋白和阿仑膦酸盐在牙周组织再生方面具有潜在的协同作用。 许多研究显示牙周手术刺激破骨细胞活动,会造成不同程度的牙槽骨丢失。有研究发现,局部给予阿仑膦酸钠可以减少牙周手术后的骨质流失,可以作为常规牙周治疗的辅助手段,以减少术后骨吸收,在预防牙周病方面发挥重要作用[33]。KHAJURIA等[34]开发了一种基于壳聚糖的利塞膦酸盐锌羟基磷灰石膜(CRZHDF),在限制牙槽骨吸收方面展现出优势,对牙周骨重塑和抑制牙槽骨"
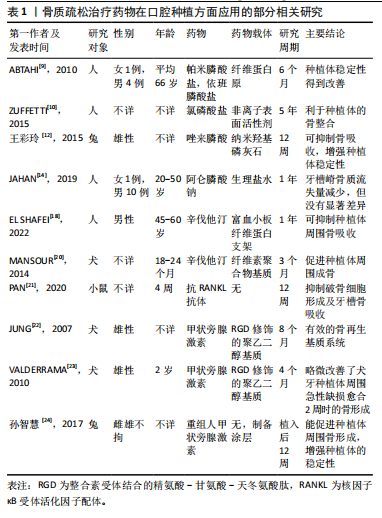
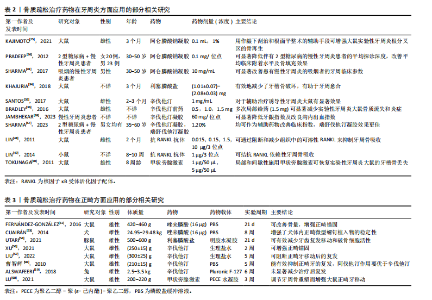
吸收显示出积极作用,推测可能是通过抑制破骨细胞活性实现的。 2.2.2 他汀类药物 局部应用辛伐他汀已被证明可以刺激体内啮齿动物和体外人牙周韧带细胞的骨形成。在一项针对实验性牙周炎大鼠模型的研究中,局部应用辛伐他汀治疗后骨质流失显著减少,同时牙龈组织中基质金属蛋白酶8的表达水平也显著降低[35],表明辛伐他汀可能作为一种辅助疗法,与牙周常规治疗相结合,以促进牙周组织的再生和修复。BRADLEY等[36]评估了一种新型辛伐他汀前药对实验性牙周炎大鼠骨质流失和炎症的影响,发现多次局部注射含1.5 mg辛伐他汀的前药可显著减少实验性牙周炎大鼠的骨质流失和炎症发生。临床和影像学证实局部应用他汀类药物能够增强牙周常规治疗的效果[37-41]。瑞舒伐他汀在辅助龈下刮治和根面平整对骨缺损的填充及相对附着水平的增益效果上高于辛伐他汀[42]。另有研究对比了1%阿仑膦酸钠凝胶、1.2%辛伐他汀凝胶治疗牙周炎的疗效,最终阿仑磷酸钠组具有更显著的治疗效果[43]。 MARTANDE等[44]首次将自体富血小板纤维蛋白和阿托伐他汀联合治疗慢性牙周炎患者骨内三壁缺损,然而阿托伐他汀似乎不能增强富血小板纤维蛋白治疗慢性牙周炎骨缺损的再生潜能。而在GAUTAM等[45]临床试验中瑞舒伐他汀与富血小板血浆联合应用治疗慢性牙周炎骨缺损取得了更优的临床效果,这可能与瑞舒伐他汀具有更显著的抗炎作用及对骨形成的刺激效应有关。 然而,他汀类药物的临床转化一直受到水溶性差、缺乏骨亲和力和全身暴露等相关不良反应(如肝毒性)的阻碍,为了解决这些挑战,CHEN等[46]设计并合成了一种基于热响应性水凝胶的新型辛伐他汀制剂,与剂量相当的辛伐他汀相比,这种新型制剂在减少炎症细胞和保存牙槽骨结构方面表现出更好的作用。另外基于N-(2-羟丙基)甲基丙烯酰胺共聚物的热响应性聚合物辛伐他汀前药也可能成为一种有希望的牙周炎临床有效治疗药物[47]。 2.2.3 地诺单抗 在牙周病变中T淋巴细胞和B淋巴细胞表达丰富的 NF-κB 配体受体激活剂,局部牙龈注射抗RANKL抗体后可溶性RANKL浓度显著降低,牙槽骨表面的破骨细胞减少,治疗效果显著改善,说明抗RANKL抗体可通过降低可溶性RANKL水平来干扰免疫细胞介导的牙周骨吸收[48],随后LIN等[49]在实验性小鼠牙周炎模型中验证了这一结论。 2.2.4 甲状旁腺激素 牙周韧带细胞在牙周修复过程中具有调节作用,一项细胞学实验证实,短时间连续甲状旁腺激素给药刺激牙周韧带细胞向成骨细胞表型分化,这提示局部应用甲状旁腺激素可能是牙周治疗的一种选择,为后续开发局部甲状旁腺激素给药方案奠定了一定的理论基础。TOKUNAGA等[50]将甲状旁腺激素(1-34)注射到实验性牙周炎大鼠第二磨牙的骨膜下,发现局部应用甲状旁腺激素可促进大鼠牙槽骨形成,加速牙周组织的再生。 总体而言,常规牙周治疗联合上述药物局部应用的治疗效果显著优于其单一治疗或与安慰剂联合使用,并且对吸烟人群以及血糖控制良好的糖尿病患者的疗效均有显著改善。见表2。不同类型的药物在疗效方面存在差异,还需要进一步研究局部给药系统、有效剂量和给药频率、可能的不良反应以及哪种药物更适合牙周炎,需要更长的研究周期和多中心试验来进一步研究临床益处和对周围组织可能的不良影响。 2.3 正畸方面 2.3.1 双膦酸盐类 正畸治疗中的2个主要问题是支抗丧失和正畸后复发。减轻支抗丧失的传统方法包括头套、各种口内矫治器等,这些方法与患者的依从性关系密切,药理学方法在提供锚定方面具有很大的潜力,当施加正畸力时,局部应用双膦酸盐类药物可实现锚固,能够有效地抑制破骨细胞生成,从而改善骨量和增强正畸锚固[51-52]。目前,微型种植体是提供最大锚固的首选方法,正畸微型螺钉植入物可以选择性地控制牙齿运动并将不良反应降至最低。Cuairán等[53]发现局部给予小剂量的唑来膦酸可以长期维持正畸微型螺钉植入物的稳定性。 正畸后复发是一个复杂的过程,其病因尚不清楚。据报道,局部注射利塞膦酸盐可以有效抑制复发,但会产生全身效应,例如会增加胫骨的骨密度,UTARI等[54]发现含明胶水凝胶的利塞膦酸盐的释放变慢,证实了明胶水凝胶对利塞膦酸盐的控释作用,并且复发明显减少,高剂量组比低剂量组更有效地抑制了复发。 2.3.2 他汀类药物 有研究发现局部注射他汀类药物能够用于正畸锚固及阻止正畸后复发[55-57],辛伐他汀通过抗炎作用在正畸牙齿移动过程中促进牙周组织张力侧的成骨活动。辛伐他汀能够激活腺苷酸活化蛋白激酶,通过AMP活化蛋白激酶/丝裂原活化蛋白激酶/NF-κB信号通路抑制炎症反应,同时还能促进成骨相关基因如骨形态发生蛋白2的表达,从而在牙周组织张力侧促进成骨,进而增强正畸瞄固。曹智辉等[58]在大鼠牙龈局部注射他汀类药物,结果显示局部应用他汀类药物抑制正畸牙复发的效果明显。但有研究发现局部应用辛伐他汀虽然能帮助骨重塑,但在兔正畸牙移动模型中,牙齿复发21 d后局部注射辛伐他汀并没有显著减少治疗后复发[59],推测这是由于拆除矫治器具后的初始阶段,牙齿在牙槽骨内会发生反弹性移位。因此使用他汀类药物抑制破骨细胞生成可能是一种可行的治疗策略,仍需进一步研究。 2.3.3 甲状旁腺激素 局部持续的甲状旁腺激素治疗会增加破骨细胞的活性,促进骨吸收,注入骨膜下的甲状旁腺激素可以促进骨吸收细胞因子的产生,可以诱导有效的骨吸收以促进正畸牙齿的移动,LU等[60]将含有甲状旁腺激素的水凝胶置于接受正畸治疗的大鼠上颌第一磨牙的微穿孔内,发现局部注射甲状旁腺激素可通过调节牙周骨重塑而增强大鼠正畸牙移动,进一步体现了局部应用甲状旁腺激素的潜在临床应用价值,甲状旁腺激素在控释水凝胶中的局部使用也被认为可以介导牙周骨重塑并提高正畸效率[61]。 这些研究表明,上述3类药物可能有利于调节正畸牙齿移动,并作为正畸牙齿移动期间牙根吸收和正畸牙齿移动后复发的潜在抑制剂,见表3。 2.4 拔牙后牙槽骨的保存及牙槽骨缺损方面 2.4.1 双膦酸盐类 拔牙导致牙槽骨的变化主要发生在拔牙后的3-6个月内,并且主要表现在颊侧牙槽壁处,颊面和舌面的骨丢失分布不均。研究发现,双膦酸盐局部应用后可以减少拔牙后牙槽骨尺寸丢失,会促进拔牙窝内类骨质的形成,抑制骨板的吸收,有利于牙槽骨缺损的愈合[62-65]。YAFFE等[66]将含有阿仑磷酸盐的明胶海绵颗粒应用于牙槽骨和黏骨膜瓣之间,发现阿仑磷酸盐的应用减少了牙槽骨的丢失,并且盐酸四环素与阿仑膦酸盐联合使用在减少牙槽骨丢失方面具有协同作用。 2.4.2 他汀类药物 局部应用辛伐他汀可以促进拔牙后骨形成和保留牙槽嵴[67-68],可通过调节生长因子的表达来影响牙槽骨重塑,含辛伐他汀的明胶支架可以促进成骨细胞分化以及抑制破骨细胞吸收,而且牙槽嵴的增加有利于后期种植体的植入[69],局部应用辛伐他汀似乎是一种经济、简便的促进骨再生的方法。有研究将含有辛伐他汀粉末(20 mg)的胶原蛋白海绵置于因破坏第二磨牙远中牙槽骨而拔除的下颌阻生第三磨牙的拔牙窝内,发现第二磨牙远中牙槽骨修复水平和骨密度明显增高,辛伐他汀有促进骨形成的能力,并且与胶原蛋白海绵联合应用不会造成额外伤害,安全可靠[70]。然而在Ⅱ类根分叉病变模型中,MORRIS等[71]发现与对照组相比,含0.5 mg辛伐他汀的凝胶注射后显示出更显著的骨质流失"

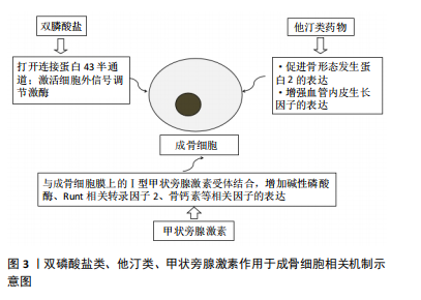
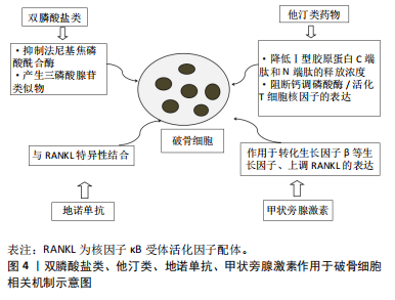
现象,骨高度降低,这一现象可能与在结缔组织内创造足够的空间来保留30 μL体积的凝胶困难有关。综上所述,需要开展更大样本量、更长时间的随访研究以进一步探讨辛伐他汀对牙槽骨形成的影响以及进一步探索辛伐他汀促进牙槽骨形成的具体机制。 基于以上研究发现,双膦酸盐类药物和他汀类药物的局部应用展现出了转化为临床实践的潜力,以促进拔牙后牙槽骨的形成和保存,而地诺单抗及甲状旁腺激素相关报道较少,此综述中未做具体描述。 2.5 再植牙 牙齿完全性脱位占全球所有牙齿创伤病例的16%。将牙齿放回牙槽窝是治疗完全性脱位牙的首选方法,牙根吸收和强直是再植牙植入后的主要并发症。 2.5.1 双膦酸盐类 使用阿仑膦酸钠预处理可以使再植牙愈合的牙周韧带支撑功能得到更好地恢复,阻止牙根吸收[72]。长期观察中发现局部使用阿仑膦酸钠在再植4个月后的牙齿中仍然对根和骨吸收有抑制作用[73],这可能是通过刺激骨形成细胞的增殖和分化以及抑制破骨细胞的功能来促进骨形成。MORI等[74]对唑来膦酸的有效剂量进行了探索,发现20 μmol/L唑来膦酸是发挥最大作用下的最小剂量,20 μmol/L唑来膦酸溶液在延迟再植牙根面处理中的应用有待进一步研究。在动物模型中,表面应用唑来膦酸钠和阿仑膦酸钠可减少再植牙的根吸收。然而研究发现在根管内使用双膦酸盐的有效性仍有争议,可能会导致更差或不显著的结果[75]。 2.5.2 地诺单抗 有研究在实验性大鼠模型中模拟了再植牙延迟再植的情况,结果证明了牙齿再植前用地诺单抗根面处理在预防延迟再植牙齿强直及替代吸收方面具有一定的效果[76],然而,目前缺乏足够有力的临床证据来支持该治疗方法的广泛推广。 牙齿再植前进行相关处理有利于减少牙根吸收和强直等并发症的发生,提高牙齿再植术的成功率,目前的研究中,双膦酸盐和地诺单抗显示出了良好的效果,后续应开展进一步深入研究,以提高再植牙的远期生存率。 药物相关性颌骨坏死是一种罕见但可能严重的不良事件,与高累计剂量的双膦酸盐或地诺单抗有关。在评估药物相关性颌骨坏死发生的可能性时,主要因素是患者对双膦酸盐或地诺单抗的累计暴露,需同时考虑每次治疗的剂量和从治疗开始给予的给药次数。然而,迄今为止,尚未确定不会发生药物相关性颌骨坏死的明确阈值。药物相关性颌骨坏死在接受高累积剂量双膦酸盐或地诺单抗的患者中比接受较低剂量的患者中更普遍。研究表明,接受低剂量双膦酸盐或地诺单抗的药物相关性颌骨坏死的发病率被认为仅略高于一般人群,超过90%的药物相关性颌骨坏死发生在接受高剂量静脉注射双膦酸盐或皮下注射地诺单抗的癌症患者中。通过将药物直接递送至牙槽骨区域,可以有效减少全身用药剂量。这种局部给药策略不仅促进了局部骨质和骨量的改善,而且减轻了对骨重塑过程的抑制作用,从而进一步降低了因药物引起的颌骨坏死风险。 2.6 其他药物 在骨质疏松治疗领域,中医药的应用日益广泛,其中包括骨碎补、丹参、骨补脂等,这些中药成分能够对OPG/RANK/RANKL、Wnt/β-Catenin及MAPKs等关键信号通路产生影响,例如研究发现骨补脂素具有抗炎和雌激素样作用,可作为雌激素受体激动剂发挥抗炎作用,为它用于辅助治疗和预防牙周炎提供了理论依据[77]。一项研究通过在实验性正畸牙齿移动大鼠模型中局部注射丹参酮ⅡA,从加力装置去除的前1 d开始注射,连续注射4周,能够有效减轻正畸治疗后牙齿移动的复发[78], 其作用机制可能涉及调节骨保护素与破骨细胞分化因子的比例,进而影响破骨细胞的活动。骨碎补局部应用于牙槽骨根分叉病变区域,能够有效促进牙槽骨的再生过程。有学者提出将骨碎补通过离子导入技术直接作用于正畸移动牙齿的牙周组织内,以促进牙槽骨的改建过程,从而加快牙齿移动的速度[79],此方法旨在通过局部应用骨碎补来增强牙周组织的血液循环,进而促进骨小梁的改建,同时利用离子导入技术使药物直达作用部位,以实现疗效的持久性和安全性,这种方法可能有助于缩短正畸治疗的总疗程。 雌激素能够抑制破骨细胞的分化,其作用机制可能是通过下调支持细胞中破骨细胞生成细胞因子的表达,雌激素受体广泛存在于牙周组织中,雌激素还可增强人牙周韧带干细胞增殖和成骨分化的潜力,有利于其在组织再生方面的应用,关于雌激素是否能通过局部应用改善牙槽骨骨量有待于进一步研究。 双磷酸盐类、他汀类、甲状旁腺激素作用于成骨细胞、破骨细胞相关机制,见图3,4。"
| [1] SALARI N, DARVISHI N, BARTINA Y, et al. Global prevalence of osteoporosis among the world older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1): 669. [2] 陈子根,邓敦,吕秀秀,等.慢性牙周炎与骨质疏松症的相关性分析[J].浙江临床医学,2023,25(9):1319-1321. [3] 邱韵,王宇蓝,张玉峰.骨质疏松症对牙种植的影响及临床考量[J].中国口腔种植学杂志,2024,29(4):336-341. [4] LEMOS CAA, DE OLIVEIRA AS, FAÉ DS, et al. Do dental implants placed in patients with osteoporosis have higher risks of failure and marginal bone loss compared to those in healthy patients? A systematic review with meta-analysis. Clin Oral Investig. 2023;27(6):2483-2493. [5] PALOMO L, BUENCAMINO-FRANCISCO MC, CAREY JJ, et al. Is long-term bisphosphonate therapy associated with benefits to the periodontium in postmenopausal women? Menopause. 2011;18(2):164-170. [6] ALENEZI A, CHRCANOVIC B, WENNERBERG A. Effects of Local Drug and Chemical Compound Delivery on Bone Regeneration Around Dental Implants in Animal Models: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2018;33(1):e1-e18. [7] KC K, BHATTARAI BP, SHRESTHA S, et al. Effect of locally delivered bisphosphonates on alveolar bone: a systematic review and meta-analysis. J Evid Based Dent Pract. 2021;21(3):101580. [8] HONG I, JOO JM, KWON YH, et al. Local delivery of pamidronate with collagen matrix mitigates buccal bone resorption following immediate implant placement - An experimental in vivo study. J Periodontal Res. 2024. doi: 10.1111/jre.13342. [9] ABTAHI J, TENGVALL P, ASPENBERG P. Bisphosphonate coating might improve fixation of dental implants in the maxilla: a pilot study. Int J Oral Maxillofac Surg. 2010;39(7):673-677. [10] ZUFFETTI F, TESTORI T, CAPELLI M, et al. The topical administration of bisphosphonates in implant surgery: a randomized split-mouth prospective study with a follow-up up to 5 years. Clin Implant Dent Relat Res. 2015;17 Suppl 1:e168-e176. [11] ABTAHI J, HENEFALK G, ASPENBERG P. Randomised trial of bisphosphonate-coated dental implants: Radiographic follow-up after five years of loading. Int J Oral Maxillofac Surg. 2016;45(12):1564-1569. [12] 王彩玲,王俐杰,樊世锋,等.局部应用唑来膦酸对兔即刻种植钛螺纹钉骨结合的影响[J].中国医学工程,2015,23(11):6-7+9. [13] ASHRAFI M, GHOLAMIAN F, DOBLARE M. A comparison between the effect of systemic and coated drug delivery in osteoporotic bone after dental implantation. Med Eng Phys. 2022;107:103859. [14] JAHAN S, KAUSHIK M, WADHAWAN A. Comparative Evaluation of Peri-implant Soft and Hard Tissue with and without Application of Bisphosphonate on Implant Surface and Osteotomy Site - A Clinico-radiographic, Cone-beam Computed Tomographic Study. Contemp Clin Dent. 2019;10(2):208-213. [15] AL-ASSAF DA, BEDE SY. The Effects of Local Alendronate With or Without Recombinant Human Bone Morphogenetic Protein 2 on Dental Implant Stability and Marginal Bone Level: A Randomized Controlled Study. J Craniofac Surg. 2022;33(4):1003-1007. [16] MOKHTARI RA, OLSSON M, ÖSTMAN PO, et al. A randomized, multicenter, double-blinded parallel study to evaluate the safety and performance of zoledronate-coated versus uncoated dental implants in partially edentulous patients. Clin Implant Dent Relat Res. 2024;26(1):78-87. [17] ISSA DR, ELAMROUSY W, GAMAL AY. Alveolar ridge splitting and simvastatin loaded xenograft for guided bone regeneration and simultaneous implant placement: randomized controlled clinical trial. Clin Oral Investig. 2024;28(1):71. [18] EL SHAFEI SF, RAAFAT SN, AMIN AH, et al. Effect of local application of platelet-rich fibrin scaffold loaded with simvastatin on peri-implant bone changes. J Indian Prosthodont Soc. 2022;22(2):152-160. [19] SUN H, MENG S, CHEN J, et al. Effects of Hyperlipidemia on Osseointegration of Dental Implants and Its Strategies. J Funct Biomater. 2023;14(4):194. [20] MANSOUR G, AL ASHWAH A, KOURA A. Evaluation of simvastatin grafting around immediate dental implants in dogs. Implant Dent. 2014;23(2):195-199. [21] PAN K, HU Y, WANG Y, et al. RANKL blockade alleviates peri-implant bone loss and is enhanced by anti-inflammatory microRNA-146a through TLR2/4 signaling. Int J Implant Dent. 2020;6(1):15. [22] JUNG RE, COCHRAN DL, DOMKEN O, et al. The effect of matrix bound parathyroid hormone on bone regeneration. Clin Oral Implants Res. 2007;18(3):319-325. [23] VALDERRAMA P, JUNG RE, THOMA DS, et al. Evaluation of parathyroid hormone bound to a synthetic matrix for guided bone regeneration around dental implants: a histomorphometric study in dogs. J Periodontol. 2010;81(5):737-747. [24] 孙智慧,郑宇,王俐杰,等.局部应用重组人甲状旁腺激素(1-34)对即刻种植骨整合的作用[J].中国组织工程研究,2017,21(26): 4210-4216. [25] KAJIMOTO NC, DE PAIVA BUISCHI Y, LOOMER PM, et al. Adjuvant therapy with 1% alendronate gel for experimental periodontitis treatment in rats. J Periodontal Implant Sci. 2021;51(6):374-385. [26] PRADEEP AR, SHARMA A, RAO NS, et al. Local drug delivery of alendronate gel for the treatment of patients with chronic periodontitis with diabetes mellitus: a double-masked controlled clinical trial. J Periodontol. 2012;83(10):1322-1328. [27] ARENA C, CAPONIO VCA, ZHURAKIVSKA K, et al. Added effect of 1% topical alendronate in intra-bony and inter-radicular defects as part of step II periodontal therapy: a systematic review with meta-analysis and trial sequential analysis. BMC Oral Health. 2022;22(1):15. [28] SHARMA A, RAMAN A, PRADEEP AR. Role of 1% alendronate gel as adjunct to mechanical therapy in the treatment of chronic periodontitis among smokers. J Appl Oral Sci. 2017;25(3):243-249. [29] DUTRA BC, OLIVEIRA AMSD, OLIVEIRA PAD, et al. Effect of 1% sodium alendronate in the non-surgical treatment of periodontal intraosseous defects: a 6-month clinical trial. J Appl Oral Sci. 2017;25(3):310-317. [30] ZYMPERDIKAS VF, YAVROPOULOU MP, KAKLAMANOS EG, et al. Bisphosphonates as Supplement to Dental Treatment: A Network Meta-Analysis. J Dent Res. 2021;100(4):341-351. [31] CHATZOPOULOS GS, KOIDOU VP, TSALIKIS L. Local drug delivery in the treatment of furcation defects in periodontitis: a systematic review. Clin Oral Investig. 2023;27(3):955-970. [32] KANORIYA D, PRADEEP AR, SINGHAL S, et al. Synergistic Approach Using Platelet-Rich Fibrin and 1% Alendronate for Intrabony Defect Treatment in Chronic Periodontitis: A Randomized Clinical Trial. J Periodontol. 2016;87(12):1427-1435. [33] BINDERMAN I, ADUT M, YAFFE A. Effectiveness of local delivery of alendronate in reducing alveolar bone loss following periodontal surgery in rats. J Periodontol. 2000;71(8):1236-1240. [34] KHAJURIA DK, ZAHRA SF, RAZDAN R. Effect of locally administered novel biodegradable chitosan based risedronate/zinc-hydroxyapatite intra-pocket dental film on alveolar bone density in rat model of periodontitis. J Biomater Sci Polym Ed. 2018;29(1):74-91. [35] SANTOS BF, SOUZA EQ, BRIGAGÃO MR, et al. Local application of statins in the treatment of experimental periodontal disease in rats. J Appl Oral Sci. 2017;25(2):168-176. [36] BRADLEY AD, ZHANG Y, JIA Z, et al. Effect of Simvastatin Prodrug on Experimental Periodontitis. J Periodontol. 2016;87(5):577-582. [37] 叶欣,段学静,吴益华,等.他汀类药物对牙周炎骨代谢调节作用的体内外研究进展[J].山东医药,2023,63(8):86-90. [38] JAMBHEKAR S, SOMAN M, SHRIVASTAVA R, et al. Comparative Evaluation of Tetracycline Hydrochloride Fiber and Simvastatin Gel as an Adjunct to Scaling and Root Planing in Periodontitis Patients. Cureus. 2023;15(7):e42314. [39] KILLEEN AC, KRELL LE, BERTELS M, et al. Effect of locally applied simvastatin on clinical attachment level and alveolar bone in periodontal maintenance patients: A randomized clinical trial. J Periodontol. 2022;93(11):1682-1690. [40] DAS RK, BHARATHWAJ VV, SINDHU R, et al. Comparative Analysis of Various Forms of Local Drug Delivery Systems on a Class 2 Furcation - A Systematic Review. J Pharm Bioallied Sci. 2023;15(Suppl 1):S742-S746. [41] ELGENDY HA, MAKKY AMA, ELAKKAD YE, et al. Syringeable atorvastatin loaded eugenol enriched PEGylated cubosomes in-situ gel for the intra-pocket treatment of periodontitis: statistical optimization and clinical assessment. Drug Deliv. 2023;30(1):2162159. [42] SHARMA P, SINGH A, MALLAPRAGADA S. Sub-gingival delivery of simvastatin and rosuvastatin for treatment of chronic periodontitis with diabetes mellitus: A randomized controlled clinical-radiographic pilot study. J Oral Biol Craniofac Res. 2023;13(2):315-320. [43] SHETTY B, KAREGOWDA P, KHAN SF, et al. Comparison of simvastatin 1.2% gel and alendronate 1% gel in chronic periodontitis as local drug delivery: A randomized clinical trial. J Indian Soc Periodontol. 2022;26(6):591-599. [44] MARTANDE SS, KUMARI M, PRADEEP AR, et al. Platelet-Rich Fibrin Combined With 1.2% Atorvastatin for Treatment of Intrabony Defects in Chronic Periodontitis: A Randomized Controlled Clinical Trial. J Periodontol. 2016;87(9):1039-1046. [45] GAUTAM K, KAPOOR A, MATHUR S, et al. Comparative Evaluation of Autogenous Bone Graft and Autologous Platelet-Rich Fibrin with and Without 1.2 mg in situ Rosuvastatin Gel in the Surgical Treatment of Intrabony Defect in Chronic Periodontitis Patients. Contemp Clin Dent. 2022;13(1):69-77. [46] CHEN N, REN R, WEI X, et al. Thermoresponsive Hydrogel-Based Local Delivery of Simvastatin for the Treatment of Periodontitis. Mol Pharm. 2021;18(5):1992-2003. [47] XU X, JIA Z, CHEN N, et al. The Development of Thermoresponsive Polymeric Simvastatin Prodrug for the Treatment of Experimental Periodontitis in Rats. Mol Pharm. 2023;20(11):5631-5645. [48] LIN X, HAN X, KAWAI T, et al. Antibody to receptor activator of NF-κB ligand ameliorates T cell-mediated periodontal bone resorption. Infect Immun. 2011;79(2):911-917. [49] LIN J, BI L, YU X, et al. Porphyromonas gingivalis exacerbates ligature-induced, RANKL-dependent alveolar bone resorption via differential regulation of Toll-like receptor 2 (TLR2) and TLR4. Infect Immun. 2014; 82(10):4127-4134. [50] TOKUNAGA K, SETO H, OHBA H, et al. Topical and intermittent application of parathyroid hormone recovers alveolar bone loss in rat experimental periodontitis. J Periodontal Res. 2011;46(6):655-662. [51] FERNÁNDEZ-GONZÁLEZ FJ, LÓPEZ-CABALLO JL, CAÑIGRAL A, et al. Osteoprotegerin and zoledronate bone effects during orthodontic tooth movement. Orthod Craniofac Res. 2016;19(1):54-64. [52] HARIKRISHNAN S, RAMASAMY N. Effect of local administration of bisphosphonate on orthodontic anchorage - A systematic review of animal studies. J Orthod Sci. 2022;11:31. [53] CUAIRÁN C, CAMPBELL PM, KONTOGIORGOS E, et al. Local application of zoledronate enhances miniscrew implant stability in dogs. Am J Orthod Dentofacial Orthop. 2014;145(6):737-749. [54] UTARI TR, ANA ID, PUDYANI PS, et al. The intrasulcular application effect of bisphosphonate hydrogel toward osteoclast activity and relapse movement. Saudi Dent J. 2021;33(5):292-298. [55] KABRA S, THOSAR NR, MALVIYA NS. Exploring the Synergistic Effect of Simvastatin in Oral Health Applications: A Literature Review. Cureus. 2023;15(8):e44411. [56] XU L, SUN X, ZHU G, et al. Local delivery of simvastatin maintains tooth anchorage during mechanical tooth moving via anti-inflammation property and AMPK/MAPK/NF-kB inhibition. J Cell Mol Med. 2021; 25(1):333-344. [57] LIU X, MUHAMMED FK, LIU Y. Simvastatin encapsulated in exosomes can enhance its inhibition of relapse after orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2022;162(6):881-889. [58] 曹智辉,王帆开,王先军.辛伐他汀与阿伐他汀对鼠正畸牙移动影响的比较[J].苏州大学学报(医学版),2010,30(4):738-740. [59] ALSWAFEERI H, ELKENANY W, MOWAFY M, et al. Effect of local administration of simvastatin on postorthodontic relapse in a rabbit model. Am J Orthod Dentofacial Orthop. 2018;153(6):861-871. [60] LU W, LI X, YANG Y, et al. PTH/PTHrP in controlled release hydrogel enhances orthodontic tooth movement by regulating periodontal bone remodaling. J Periodontal Res. 2021;56(5):885-896. [61] YI M, YIN Y, SUN J, et al. Hormone and implant osseointegration: Elaboration of the relationship among function, preclinical, and clinical practice. Front Mol Biosci. 2022;9:965753. [62] KAUFFMANN F, HÖHNE C, ASSAF AT, et al. The Influence of Local Pamidronate Application on Alveolar Dimensional Preservation after Tooth Extraction-An Animal Experimental Study. Int J Mol Sci. 2020;21(10):3616. [63] SAULACIC N, MUÑOZ F, KOBAYASHI E, et al. Effects of local application of alendronate on early healing of extraction socket in dogs. Clin Oral Investig. 2020;24(4):1579-1589. [64] JIANG J, XIAO J, WANG D, et al. Application of Implantable Polylactic-Co-Glycolic Acid Microcapsule in Repairing Alveolar Bone Defects. Evid Based Complement Alternat Med. 2021;2021:5580785. [65] 崔彩雯,张健,马婷,等.唑来膦酸局部应用对大鼠拔牙创软硬组织的影响[J].口腔颌面修复学杂志,2011,12(5):261-264. [66] YAFFE A, HERMAN A, BAHAR H, et al. Combined local application of tetracycline and bisphosphonate reduces alveolar bone resorption in rats. J Periodontol. 2003;74(7):1038-1042. [67] HARSHA G, MADHAVI S, ARTHI S, et al. Evaluation of efficacy of simvastatin in bone regeneration following local application in third molar extraction socket: A randomized control trial. Natl J Maxillofac Surg. 2023;14(2):286-293. [68] DINIZ JA, BARBIRATO DDS, DO NASCIMENTO EHL, et al. Tomographic evaluation of the effect of simvastatin topical use on alveolar bone microarchitecture, pain and swelling after mandibular third molar extraction: a randomized controlled trial. Clin Oral Investig. 2022;26(4):3533-3545. [69] ESMAEILI V, BOOSTANI H, AHMADPOUR F. Efficacy of spongy xenogeneic scaffold loaded with simvastatin in the treatment of severe alveolar horizontal defect: A clinical and histological study. Niger J Clin Pract. 2023;26(4):369-375. [70] 韦子翔.辛伐他汀联合胶原蛋白海绵对下颌第二磨牙远中牙槽骨缺损的影响[D].百色:右江民族医学院,2023. [71] MORRIS MS, LEE Y, LAVIN MT, et al. Injectable simvastatin in periodontal defects and alveolar ridges: pilot studies. J Periodontol. 2008;79(8):1465-1473. [72] 邸天凯,陈宇江,汪璐璐,等.促进撕脱性损伤牙延期再植后牙周愈合的研究进展[J].中国实用口腔科杂志,2021,14(6):728-733. [73] KOMATSU K, SHIMADA A, SHIBATA T, et al. Long-term effects of local pretreatment with alendronate on healing of replanted rat teeth. J Periodontal Res. 2008;43(2):194-200. [74] MORI GG, JANJACOMO DM, NUNES DC, et al. Effect of zoledronic acid used in the root surface treatment of late replanted teeth: a study in rats. Braz Dent J. 2010;21(5):452-457. [75] THONG YL, MESSER HH, ZAIN RB, et al. Intracanal bisphosphonate does not inhibit replacement resorption associated with delayed replantation of monkey incisors. Dent Traumatol. 2009;25(4):386-393. [76] DA SILVA LAB, LONGO DL, STUANI MBS, et al. Effect of root surface treatment with denusomab after delayed tooth replantation. Clin Oral Investig. 2021;25(3):1255-1264. [77] LI H, XU J, LI X, et al. Anti-inflammatory activity of psoralen in human periodontal ligament cells via estrogen receptor signaling pathway. Sci Rep. 2021;11(1):8754. [78] 张世英,刘继光,赵刚.丹参酮ⅡA局部注射正畸牙移动后复发阶段破骨细胞分化因子的表达[J].中国组织工程研究,2014,18(11): 1730-1736. [79] 李祎铮,李永明.加速正畸牙齿移动新方法:中药骨碎补局部离子导入[J].临床医学研究与实践,2018,3(1):194-195. |
| [1] | Qin Hao, Kang Teng, Liu Gang. Long non-coding RNA directly or indirectly affects osteoporosis through p38MAPK signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(1): 175-184. |
| [2] | Abuduwupuer·Haibier, Alimujiang·Yusufu, Maihemuti·Yakufu, Maimaitimin·Abulimiti, Tuerhongjiang·Abudurexiti. Meta-analysis of efficacy and safety of terlipatide and bisphosphate in the treatment of postmenopausal osteoporosis fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 639-645. |
| [3] | Wu Ruiqi, Zhang Xuan, Zhou Yi, Meng Lin, Li Hongyu. Two-sample Mendelian randomization analysis of the relationship between statins and the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(26): 4106-4112. |
| [4] | Zhou Jing, Zhang Zhao. Osteoprotegerin/receptor activator of nuclear factor kappa-B/receptor activator of nuclear factor kappa-B ligand and the application of relevant target therapy in oral medicine [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3736-3742. |
| [5] | Fang Xiang, Zhou Zhengxin, Zhu Lei, Rui Ren, Xu Maoyu, Zhu Caiyu. Effect of Gubitongxiao granules in a mouse model of steroid-induced necrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(16): 2599-2604. |
| [6] | Sun Jinyi, Wang Qinying, Li Ying, Meng Maohua, Chen Helin, Zeng Xiao, Shu Jiayu, Li Wenjie, Luo Yuncai, Dong Qiang. The role of silent information regulator in periodontitis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(11): 1737-1742. |
| [7] | Sun Xiaotong, Cheng Yi, Bi Lan, Wang Huida. Effect of parathyroid hormone and parathyroid hormone-related peptides on tissue remodeling during orthodontics [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(14): 2234-2241. |
| [8] | Huang Zhicai, Xie Liuqin, Wang Guangsu, Zhang Guoxing, Tang Zhenglong. Parathyroid hormone promotes bone healing in rabbits after free reduction of mandibular condyle fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(14): 2172-2178. |
| [9] | Zhang Shengmin, Cao Changhong, Liu Chao. Adipose-derived stem cells integrated with concentrated growth factors prevent bisphosphonate-related osteonecrosis of the jaws in SD rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2982-2987. |
| [10] | Chen Jiayun, Li Anan, Lü Zhaohui, Wu Zixuan, Cai Minjie, Huang Xuyan . Effect of long-term use of proton pump inhibitors on bone mineral density and bone metabolism: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(17): 2775-2780. |
| [11] | Xie Liuqin, Huang Zhicai, Wang Guangsu, Zhang Guoxing, Li-Du Chenhui, Li Xiao, Tang Zhenglong. Effect of parathyroid hormone on cartilage healing in a rabbit model of mandibular condylar fracture [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(32): 5114-5121. |
| [12] |
Dong Xiling, Zhang Xiaoming, Liu Tongbin.
Recombinant human parathyroid hormone (1-34): pro-osteogenic action and application in oral field [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(26): 4231-4236. |
| [13] | Wang Hui . Optimization of culture and secretion of parathyroid cells via increasing the parathyroid hormone level in cell supernatant [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(25): 4025-4030. |
| [14] | Bo Mao-sheng1, Zhao Jian-ning1, Hong Ye2. Correlation of the signaling pathways of bone metabolism and lipid metabolism with bone metabolism related diseases: theoretical advance and research direction [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(20): 3269-3274. |
| [15] | Zhou Qi, Wei Li, Jiang Li-ting, Li Ning, Gao Yi-ming. Effects of bisphosphonates on the expression of Bcl-2, Bax and Caspase-3 in condylar cartilage of osteoporosis rats [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(27): 3970-3976. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||