Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (17): 2775-2780.doi: 10.3969/j.issn.2095-4344.3155
Previous Articles Next Articles
Effect of long-term use of proton pump inhibitors on bone mineral density and bone metabolism: a Meta-analysis
Chen Jiayun1, Li Anan1, Lü Zhaohui2, Wu Zixuan1, Cai Minjie1, Huang Xuyan3
- 1Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China; 2Guangdong Second Hospital of Traditional Chinese Medicine, Guangzhou 510095, Guangdong Province, China; 3Southern Medical University, Guangzhou 510080, Guangdong Province, China
-
Received:2020-05-18Revised:2020-05-20Accepted:2020-06-09Online:2021-06-18Published:2021-01-08 -
Contact:Lü Zhaohui, Master, Chief physician, Professor, Master’s supervisor, Guangdong Second Hospital of Traditional Chinese Medicine, Guangzhou 510095, Guangdong Province, China -
About author:Chen Jiayun, Master candidate, Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
Supported by:the Scientific Research Project of Traditional Chinese Medicine Bureau of Guangdong Province, No. 20202013
CLC Number:
Cite this article
Chen Jiayun, Li Anan, Lü Zhaohui, Wu Zixuan, Cai Minjie, Huang Xuyan . Effect of long-term use of proton pump inhibitors on bone mineral density and bone metabolism: a Meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(17): 2775-2780.
share this article
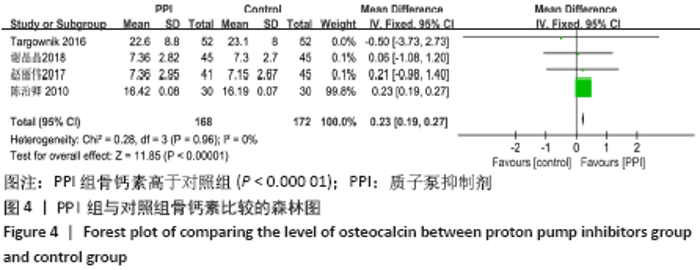
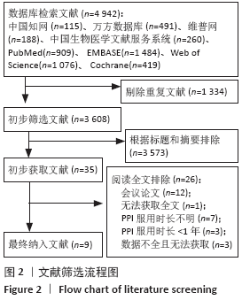
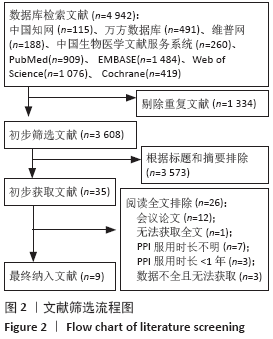
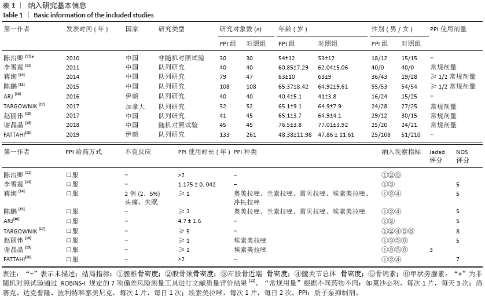
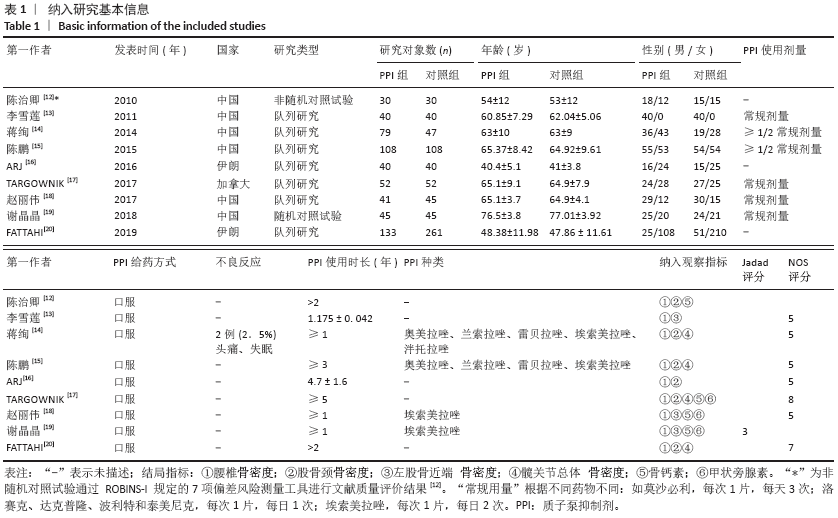
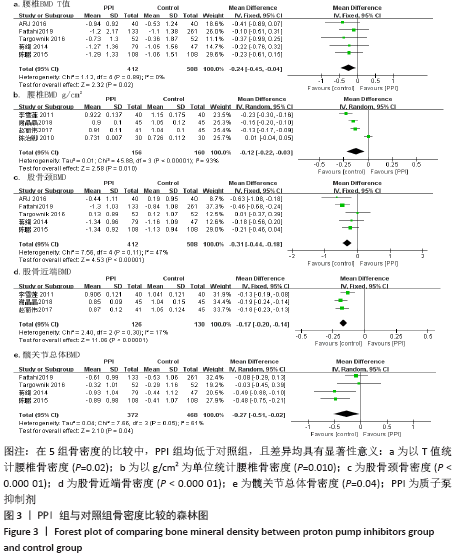
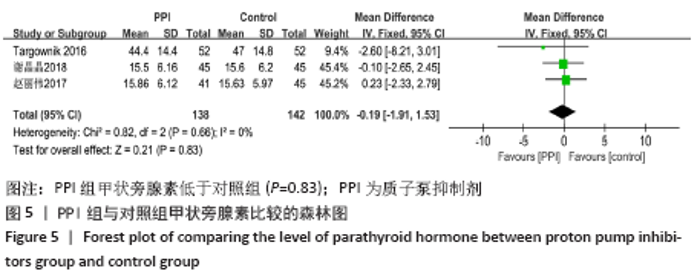
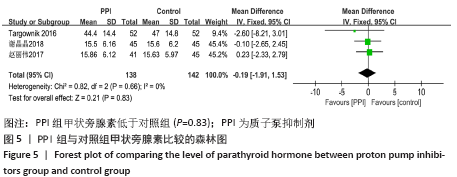
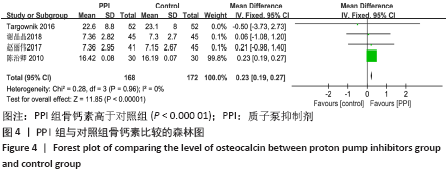
腰椎骨密度:以T值统计腰椎骨密度的文献共有5篇[14-17,20],以g/cm2为单位统计骨密度的文献共有4篇[12-13,18-19]。以 T 值统计腰椎骨密度的5篇文献[14-17,20],异质性分析 P=0.89,I2=0%,在固定效应模型下,分析结果表明PPI组腰椎骨密度低于对照组(MD=-0.24,95%CI:-0.45至 -0.04,P=0.02)。以g/cm2为单位统计腰椎骨密度的4篇文献[12-13,18-19],异质性分析:P < 0.000 01,I2=93%,在随机效应模型下,分析结果表明PPI组腰椎骨密度低于对照组(MD=-0.12,95%CI:-0.22至-0.03,P=0.010)。此异质性较大,研究间无法查明临床上或方法学上的异质性来源,故采用描述性定性分析:有4篇文献结果均表明 PPI 组腰椎骨密度低于对照组(P < 0.05)[12-13,18-19]。 股骨颈骨密度:有6篇文献报道了长期服用 PPI 对股骨颈骨密度的影响[12,14-17,20],其中5篇文献以 T 值统计[14-17,20],1 篇文献以 g/cm2 为单位统计[12]。对以 T 值统计骨密度的5篇文献进行Meta分析[14-17,20],异质性分析:P=0.11,I2=47%,在固定效应模型下,分析结果表明PPI 组股骨颈骨密度低于对照组(MD=-0.31,95%CI:-0.44至-0.18,P < 0.000 01)。对以g/cm2为单位统计骨密度的1篇文献进行描述性定性分析[12]:该文献结果认为 PPI组股骨颈骨密度低于对照组(P < 0.05)。 股骨近端骨密度:由3篇文献报道了长期服用 PPI 对股骨近端骨密度的影响[13,18-19],异质性分析 P=0.30,I2=17%,在固定效应模型下,分析结果表明 PPI 组股骨近端骨密度低于对照组(MD=-0.17,95%CI:-0.20至-0.14,P < 0.000 01)。 髋关节总体骨密度:有4篇文献报道了长期服用 PPI 对髋关节骨密度的影响[14-15,17,20],异质性分析:P=0.05,I2=61%,在随机效应模型下,分析结果表明PPI组髋关节总体骨密度低于对照组(MD=-0.27,95%CI:-0.51至-0.02,P=0.04)。此异质性稍大,通过观察,其中有2篇文献研究对象为白种人[17, 20],2篇文献研究对象为黄种人[14-15],因此,将其分为2组进行分析时,发现各自的异质性均降至0%,异质性检测结果分别为:白种人:P=0.83,I2=0%;黄种人:P=0.97,I2=0%。可见,人种差异可能是异质性的来源。 2.3.2 各组骨钙素差异 纳入的文献中有4篇文献报道了长期服用 PPI 对骨钙素的影响[12,17-19],共340例患者,其中PPI组168例,对照组172 例。异质性分析:P=0.96,I2=0%,在固定效应模型下,分析结果表明 PPI 组骨钙素高于对照组(MD=0.23,95%CI:0.19-0.27,P < 0.000 01),如图4。 "
| [1] SHIN, YH, GONG HS, BAEK GH. Lower Trabecular Bone Score is Associated With the Use of Proton Pump Inhibitors. J Clin Densitom. 2019;22(2):236-242. [2] ITO T, JENSEN RT. Association of long-term proton pump inhibitor therapy with bone fractures and effects on absorption of calcium, vitamin B12, iron, and magnesium. Curr Gastroenterol Rep. 2010;12(6):448-457. [3] THOMSON ABR, SAUVE MD, KASSAM N, et al. Safety of the long-term use of proton pump inhibitors. World J Gastroenterol. 2010;16(19):2323-2330. [4] UMAR S, RANA A, KAPETANOS A. Long-term proton pump inhibitor use in primary care internal medicine resident clinic. Am J Gastroenterol. 2017;112:S597. [5] UEBERSCHAER H, ALLESCHER HD.. Proton pump inhibitor-side effects and complications of long-term proton pump inhibitor administration. Zeitschrift Fur Gastroenterologie. 2017;55(1): 63-74. [6] NASSAR Y, RICHTERS. Proton-pump inhibitor use and fracture risk: an updated systematic review and meta-analysis. J Bone Metabolism. 2018;25(3):141-151. [7] van der Hoorn MMC, Tett SE, de Vries OJ, et al. The effect of dose and type of proton pump inhibitor use on risk of fractures and osteoporosis treatment in older Australian women: a prospective cohort study. Bone. 2015;81:675-682. [8] 张萌萌,张秀珍,邓伟民,等.骨代谢生化指标临床应用专家共识(2020)[J].中国骨质疏松杂志,2020,26(6):1-31. [9] JADAD AR, MOORE RA, CARROLL D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1-12. [10] STERNE JA, HERNáN MA, REEVES BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [11] STANG, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010L25(9):603-605. [12] 陈治卿.骨质疏松与质子泵抑制剂相关性探讨[J].中国骨质疏松杂志,2010,16(7): 504-505, 514. [13] 李雪莲,周力.长期应用质子泵抑制剂对老年男性消化性溃疡患者骨密度的影响[J].贵阳医学院学报, 2011,36(5):528-529. [14] 蒋绚,张庆文,张振宇,等.长期应用质子泵抑制剂的风险观察[J].中华医学杂志, 2014,94(4):284-288. [15] 陈鹏,唐进先,吴冬寒.胃溃疡患者应用质子泵抑制剂的远期风险研究[J].中国中西医结合消化杂志,2015,23(9):615-617, 621. [16] ARJ A, RAZAVI ZADE M, YAVARI M, et al. Proton pump inhibitors use and change in bone mineral density. Int J Rheum Dis. 2016;19(9): 864-868. [17] TARGOWNIK LE, GOERTZEN AL, LUO Y, et al. Long-term proton pump inhibitor use is not associated with changes in bone strength and structure. Am J Gastroenterol. 2017;112(1):95-101. [18] 赵丽伟,刘改芳,吴婧,等.长期服用质子泵抑制剂对老年胃食管反流患者骨密度、骨代谢指标及胃泌素水平的影响[J].中国老年学杂志,2017,37(14):3525-3526. [19] 谢晶晶,方莉莉,陈吓妹.长期服用质子泵抑制剂对老年胃食管反流患者骨度、骨代谢指标及胃泌素水平的影响[J].临床合理用药杂志,2018,11(32):44-45. [20] FATTAHI MR, NIKNAM R, SHAMS M, et al. The Association Between Prolonged Proton Pump Inhibitors Use and Bone Mineral Density. Risk Man Health Policy. 2019;12: 349-355. [21] 毛旭峰,杨樟卫.质子泵抑制剂临床超适应证使用的医疗大数据分析[J].药学实践杂志, 2020,38(2):184-188. [22] FOODD, ADMINISTRATION. FDA Drug Safety Communication: possible increased risk of fractures of the hip, wrist, and spine with the use of proton pump inhibitors. Accessed May. 2010. [23] YANG SD, CHEN Q, WEI HK, et al. Bone fracture and the interaction between bisphosphonates and proton pump inhibitors: a meta-analysis. Int J Clin Exp Med. 2015;8(4):4899-4910. [24] 于丽媛,龚晓健,王永庆.长期使用质子泵抑制剂致骨质疏松的研究进展[J].药学与临床研究,2017,25(3):237-242. [25] HYUN JJ, CHUN HJ, KEUM B, et al. Effect of omeprazole on the expression of transcription factors in osteoclasts and osteoblasts. Int J Mol Med. 2010;26(6):877-883. [26] KARSDAL MA, HENRIKSEN K., SøRENSEN MG, et al. Acidification of the Osteoclastic Resorption Compartment Provides Insight into the Coupling of Bone Formation to Bone Resorption. Am J Pathol. 2005;166(2):467-476. [27] GOLTZMAN D, MANNSTADT M, MARCOCCI C. Physiology of the Calcium-Parathyroid Hormone-Vitamin D Axis. Front Horm Res. 2018;50:1-13. [28] CASTIGLIONI S, CAZZANIGA A, ALBISETTI W, et al. Magnesium and osteoporosis: current state of knowledge and future research directions. Nutrients. 2013;5(8):3022-3033. [29] 商晓盼,李涛,陆雨桐,等.镁离子在骨代谢中的分子机制研究与进展[J].中国组织工程研究,2016,20(48):7280-7287. [30] HARTMAN B, DONNELLY-VANDERLOO M, WATSON T, et al. Proton-pump inhibitor therapy and vitamin B12 status in an inpatient hospital setting. Appl Physiol Nutr Metab. 2016;41(10):1071-1076. [31] HERRMANN M, PETER SCHMIDT J, UMANSKAYA N, et al. The role of hyperhomocysteinemia as well as folate, vitamin B(6) and B(12) deficiencies in osteoporosis: a systematic review. Clin Chem Lab Med. 2007;45(12): 1621-1632. [32] LAPUMNUAYPOL K, THONGPRAYOON C, WIJARNPREECHA K, et al. Risk of fall in patients taking proton pump inhibitors: a meta-analysis. QJM. 2019;112(2):115-121. [33] WALSH JH, RICHARDSON CT, FORDTRAN JS. pH dependence of acid secretion and gastrin release in normal and ulcer subjects. J Clin Invest. 1975;55(3):462-468. [34] BEKTAŞ M, SARAç N, CETINKAYA H, et al. Effects of Helicobacter pylori infection and long-term proton pump inhibitor use on enterochromaffin-like cells. Ann Gastroenterol. 2012;25(2):123-127. [35] BIOSSE-DUPLAN, M. BAROUKH B, DY M, et al. Histamine promotes osteoclastogenesis through the differential expression of histamine receptors on osteoclasts and osteoblasts. Am J Pathol. 2009;174(4):1426-1434. [36] SAHARA T, ITOH K, DEBARI K, et al. Specific biological functions of vacuolar-type H(+)-ATPase and lysosomal cysteine proteinase, cathepsin K, in osteoclasts. Anat Rec A Discov Mol Cell Evol Biol. 2003;270(2):152-161. [37] 王敏娇,司家文,沈国芳.促进骨形成的甲状旁腺激素:作用及机制[j].中国组织工程研究,2015,19(15):2405-2409. |
| [1] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [2] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [5] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [6] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [7] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [8] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [9] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [10] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [11] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [12] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [13] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [14] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| [15] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||