Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (23): 3709-3714.doi: 10.12307/2024.455
Previous Articles Next Articles
Effects of icariin on proliferation and differentiation of MC3T3-E1 cells in an inflammatory environment
Han Yue, Wang Yufei, Liu Wanqing, Dong Ming, Niu Weidong
- Department of Endodontics, School of Stomatology, Dalian Medical University, Dalian 116044, Liaoning Province, China
-
Received:2023-07-03Accepted:2023-08-21Online:2024-08-18Published:2023-09-13 -
Contact:Niu Weidong, MD, Professor, Doctoral supervisor, Department of Endodontics, School of Stomatology, Dalian Medical University, Dalian 116044, Liaoning Province, China -
About author:Han Yue, Master candidate, Physician, Department of Endodontics, School of Stomatology, Dalian Medical University, Dalian 116044, Liaoning Province, China -
Supported by:the National Natural Science Foundation of China, Nos. 82270971 and 82100998 (to NWD); General Project of Liaoning Provincial Department of Education, No. LJKZ0841 (to NWD); Liaoning Provincial Science and Technology Program, No. 2021JH2/10300027 (to NWD); Liaoning Provincial Natural Science Foundation, No. 2022-BS-237 (to NWD)
CLC Number:
Cite this article
Han Yue, Wang Yufei, Liu Wanqing, Dong Ming, Niu Weidong. Effects of icariin on proliferation and differentiation of MC3T3-E1 cells in an inflammatory environment[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3709-3714.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
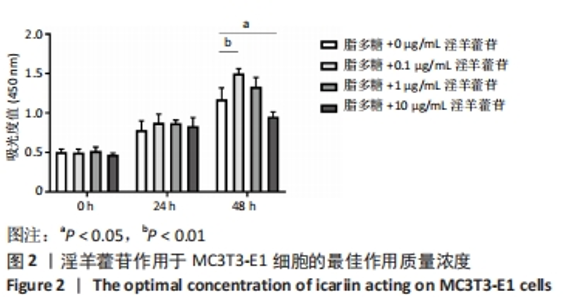
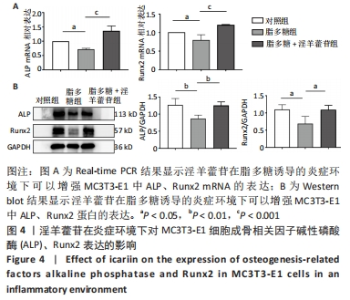
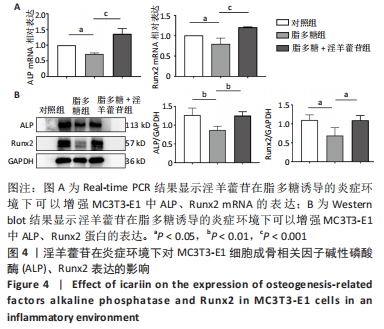
2.1 脂多糖作用于MC3T3-E1细胞的最佳作用质量浓度与时间 2.1.1 最佳作用质量浓度 加入0,0.1,1,10,100 μg/mL脂多糖刺激MC3T3-E1细胞24 h,可以看到10,100 μg/mL时细胞增殖活性明显降低,差异有显著性意义(P < 0.05),说明高质量浓度的脂多糖刺激对MC3T3-E1细胞产生了毒性作用,最终确定以1 μg/mL为最佳作用质量浓度,见图1A。 2.1.2 最佳作用时间 以0,1 μg/mL脂多糖分别刺激MC3T3-E1细胞0,24,48 h,结果显示24 h时脂多糖组细胞的增殖活性降低,48 h 时脂多糖组细胞的增殖活性明显下降,差异有显著性意义(P < 0.05),因此确定最佳实验时间24 h,见图1B。"
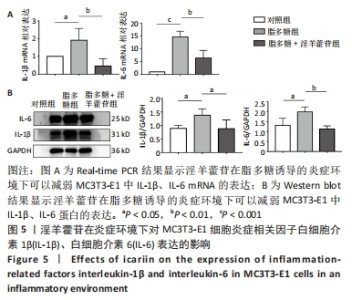
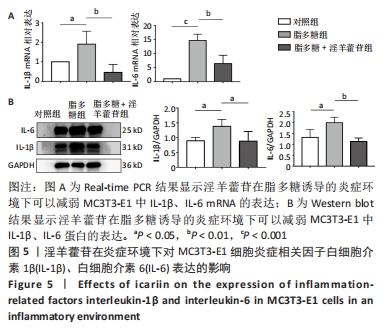
2.5 淫羊藿苷在脂多糖刺激的炎症环境下对MC3T3-E1细胞炎症相关因子白细胞介素1β、白细胞介素6表达的影响 Real-time PCR结果显示,与对照组相比,脂多糖组炎症相关因子白细胞介素1β、白细胞介素6 mRNA表达水平明显升高,在淫羊藿苷作用48 h后,与脂多糖组相比,脂多糖+淫羊藿苷组白细胞介素1β、白细胞介素6 mRNA表达水平明显降低,差异有显著性意义(P < 0.05),见图5A;Western blot 结果显示,与对照组相比,脂多糖组炎症相关因子白细胞介素1β、白细胞介素6 蛋白表达水平明显升高,与脂多糖组相比,脂多糖+淫羊藿苷组白细胞介素1β、白细胞介素6蛋白表达水平明显降低,差异有显著性意义(P < 0.05),见图5B。"
| [1] CAVALLA F, LETRA A, SILVA RM, et al. Determinants of Periodontal/Periapical Lesion Stability and Progression. J Dent Res. 2021;100(1):29-36. [2] MÖLLER AJ, FABRICIUS L, DAHLÉN G, et al. Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res. 1981;89(6):475-484. [3] DAHLÉN G. Microbiology and treatment of dental abscesses and periodontal-endodontic lesions. Periodontol 2000. 2002;28:206-239. [4] LIN X, CHI D, MENG Q, et al. Single-Cell Sequencing Unveils the Heterogeneity of Nonimmune Cells in Chronic Apical Periodontitis. Front Cell Dev Biol. 2022;9:820274. [5] GALLER KM, WEBER M, KORKMAZ Y, et al. Inflammatory Response Mechanisms of the Dentine-Pulp Complex and the Periapical Tissues. Int J Mol Sci. 2021;22(3):1480. [6] LUO X, WAN Q, CHENG L, et al. Mechanisms of bone remodeling and therapeutic strategies in chronic apical periodontitis. Front Cell Infect Microbiol. 2022;12:908859. [7] YU W, ZHONG L, YAO L, et al. Bone marrow adipogenic lineage precursors promote osteoclastogenesis in bone remodeling and pathologic bone loss. J Clin Invest. 2021;131(2):e140214. [8] WEI W, LI J, LIU X, et al. Inhibition of RGS10 Aggravates Periapical Periodontitis via Upregulation of the NF-κB Pathway. J Endod. 2022; 48(10):1308-1318. [9] HAJISHENGALLIS G. New developments in neutrophil biology and periodontitis. Periodontol 2000. 2020;82(1):78-92. [10] TAN X, HUANG D, ZHOU W, et al. Dickkopf-1 may regulate bone coupling by attenuating wnt/β-catenin signaling in chronic apical periodontitis. Arch Oral Biol. 2018;86:94-100. [11] XU R, GUO D, ZHOU X, et al. Disturbed bone remodelling activity varies in different stages of experimental, gradually progressive apical periodontitis in rats. Int J Oral Sci. 2019;11(3):27. [12] WANG X, QUINN PJ. Lipopolysaccharide: Biosynthetic pathway and structure modification. Prog Lipid Res. 2010;49(2):97-107. [13] WITTGOW WC JR, SABISTON CB JR. Microorganisms from pulpal chambers of intact teeth with necrotic pulps. J Endod. 1975;1(5):168-171. [14] FELIPE PEREIRA R, WILLIAN LATTARI TESSARIN G, YAMAMOTO CHIBA F, et al. Apical periodontitis promotes insulin resistance and alters adaptive immunity markers in rats. Saudi Dent J. 2021;33(8):979-986. [15] LOMBARDO BEDRAN TB, MARCANTONIO RA, SPIN NETO R, et al. Porphyromonas endodontalis in chronic periodontitis: a clinical and microbiological cross-sectional study. J Oral Microbiol. 2012;4. doi: 10.3402/jom.v4i0.10123. [16] WANG R, YANG D, YU YQ, et al. Effect of inhibition of Porphyromonas endodontalis on osteoblast differentiation. Shanghai Kou Qiang Yi Xue. 2021;30(4):350-354. [17] FU X, SUN X, ZHANG C, et al. Genkwanin Prevents Lipopolysaccharide-Induced Inflammatory Bone Destruction and Ovariectomy-Induced Bone Loss. Front Nutr. 2022;9:921037. [18] YANG D, LI R, QIU LH, et al. Effects of lipopolysaccharides extracted from Porphyromonas endodontalis on the expression of IL-1beta mRNA and IL-6 mRNA in osteoblasts. Shanghai Kou Qiang Yi Xue. 2009;18(2):194-197. [19] FANG C, HE M, LI D, et al. YTHDF2 mediates LPS-induced osteoclastogenesis and inflammatory response via the NF-κB and MAPK signaling pathways. Cell Signal. 2021;85:110060. [20] HONG C, YANG L, ZHANG Y, et al. Epimedium brevicornum Maxim. Extract exhibits pigmentation by melanin biosynthesis and melanosome biogenesis/transfer. Front Pharmacol. 2022;13:963160. [21] LUO Z, DONG J, WU J. Impact of Icariin and its derivatives on inflammatory diseases and relevant signaling pathways. Int Immunopharmacol. 2022;108:108861. [22] MING LG, CHEN KM, XIAN CJ. Functions and action mechanisms of flavonoids genistein and icariin in regulating bone remodeling. J Cell Physiol. 2013;228(3):513-521. [23] KARSENTY G, WAGNER EF. Reaching a genetic and molecular understanding of skeletal development. Dev Cell. 2002;2(4):389-406. [24] TAKAYANAGI H. Osteoimmunology: shared mechanisms and crosstalk between the immune and bone systems. Nat Rev Immunol. 2007;7(4): 292-304. [25] LI Y, LING J, JIANG Q. Inflammasomes in Alveolar Bone Loss. Front Immunol. 2021;12:691013. [26] ALQURIA TA, ALFIRDOUS RA, GUPTA S, et al. Comparison of conventional and contemporary root canal disinfection protocols against bacteria, lipoteichoic acid (LTA), and lipopolysaccharide (LPS). Sci Rep. 2023;13(1):1206. [27] SUDO H, KODAMA HA, AMAGAI Y, et al. In vitro differentiation and calcification in a new clonal osteogenic cell line derived from newborn mouse calvaria. J Cell Biol. 1983;96(1):191-198. [28] TIAGO DM, CANCELA ML, LAIZÉ V. Proliferative and mineralogenic effects of insulin, IGF-1, and vanadate in fish osteoblast-like cells. J Bone Miner Metab. 2011;29(3):377-382. [29] NIU T, ROSEN CJ. The insulin-like growth factor-I gene and osteoporosis: a critical appraisal. Gene. 2005;361:38-56. [30] KITASE Y, PRIDEAUX M. Targeting osteocytes vs osteoblasts. Bone. 2023;170:116724. [31] CAO FY, LONG Y, WANG SB, et al. Fluorescence light-up AIE probe for monitoring cellular alkaline phosphatase activity and detecting osteogenic differentiation. J Mater Chem B. 2016;4(26):4534-4541. [32] VIMALRAJ S. Alkaline phosphatase: Structure, expression and its function in bone mineralization. Gene. 2020;754:144855. [33] SILLER AF, WHYTE MP. Alkaline Phosphatase: Discovery and Naming of Our Favorite Enzyme. J Bone Miner Res. 2018;33(2):362-364. [34] KOMORI T. Molecular Mechanism of Runx2-Dependent Bone Development. Mol Cells. 2020;43(2):168-175. [35] INADA M, YASUI T, NOMURA S, et al. Maturational disturbance of chondrocytes in Cbfa1-deficient mice. Dev Dyn. 1999;214(4):279-290. [36] KOMORI T, YAGI H, NOMURA S, et al. Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell. 1997;89(5):755-764. [37] KOMORI T. Regulation of Proliferation, Differentiation and Functions of Osteoblasts by Runx2. Int J Mol Sci. 2019;20(7):1694. [38] MALKOV MI, LEE CT, TAYLOR CT. Regulation of the Hypoxia-Inducible Factor (HIF) by Pro-Inflammatory Cytokines. Cells. 2021;10(9):2340. [39] LOPEZ-CASTEJON G, BROUGH D. Understanding the mechanism of IL-1β secretion. Cytokine Growth Factor Rev. 2011;22(4):189-195. [40] ZHANG H, LIU L, JIANG C, et al. MMP9 protects against LPS-induced inflammation in osteoblasts. Innate Immun. 2020;26(4):259-269. [41] ZHOU M, GUO M, SHI X, et al. Synergistically Promoting Bone Regeneration by Icariin-Incorporated Porous Microcarriers and Decellularized Extracellular Matrix Derived From Bone Marrow Mesenchymal Stem Cells. Front Bioeng Biotechnol. 2022;10:824025. [42] CAO H, KE Y, ZHANG Y, et al. Icariin stimulates MC3T3-E1 cell proliferation and differentiation through up-regulation of bone morphogenetic protein-2. Int J Mol Med. 2012;29(3):435-439. [43] XIAO Q, CHEN A, GUO F. Effects of Icariin on expression of OPN mRNA and type I collagen in rat osteoblasts in vitro. J Huazhong Univ Sci Technolog Med Sci. 2005;25(6):690-692. [44] SHAUKAT A, SHAUKAT I, RAJPUT SA, et al. Icariin Alleviates Escherichia coli Lipopolysaccharide-Mediated Endometritis in Mice by Inhibiting Inflammation and Oxidative Stress. Int J Mol Sci. 2022;23(18):10219. [45] LI X, KHAN I, XIA W, et al. Icariin enhances youth-like features by attenuating the declined gut microbiota in the aged mice. Pharmacol Res. 2021;168:105587. [46] LIU J, LI D, SUN X, et al. Icariine Restores LPS-Induced Bone Loss by Downregulating miR-34c Level. Inflammation. 2016;39(5):1764-1770. [47] YU X, DONG M, WANG L, et al. Nanotherapy for bone repair: milk-derived small extracellular vesicles delivery of icariin. Drug Deliv. 2023;30(1):2169414. |
| [1] | Wang Shanshan, Shu Qing, Tian Jun. Physical factors promote osteogenic differentiation of stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1083-1090. |
| [2] | Wang Wen, Zheng Pengpeng, Meng Haohao, Liu Hao, Yuan Changyong. Overexpression of Sema3A promotes osteogenic differentiation of dental pulp stem cells and MC3T3-E1 [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 993-999. |
| [3] | Li Lisi, Zhang Chengdong, Li Xiaolong, Ye Ziyu, Pu Chao, Yang Zaijun, Shi Feng, Xiao Dongqin. Growth differentiation factor-5 modified by bisphosphonate promotes osteogenic differentiation of MC3T3-E1 cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 373-379. |
| [4] | Xiao Dongyan, He Wei, Xiao Zhiying, Liao Yue, Mao Jiahao, He Yihuai, Jiang Zhigang. Protective effect and mechanism of icariin against carbon tetrachloride-induced acute liver injury in mice [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3654-3660. |
| [5] | Yang Qihang, Pu Rui, Chen Ziyang, Leng Siyi, Song Yongjing, Liu Hui, Du Guangyou. Role and mechanism of intestinal flora metabolites in obesity regulation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 308-314. |
| [6] | Wang Zhen, Xu Shunen, Tang Geng, Luo Siwei, Teng Jianxiang, Xie Mengli, He Jialin, Ye Chuan. Biocompatibility and electrical output performance of composite piezoelectric film and osteogenic differentiation of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 1969-1975. |
| [7] | Yuan Yuanyuan, Pan Lu, Zhou Shaolan, Liang Yan, Xu Jianwei, Xu Wen. Effect of miR-26b on proliferation, migration and osteogenic differentiation of stem cells from human exfoliated deciduous teeth and human umbilical cord mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 2017-2023. |
| [8] | Yang Runze, Wang Wei, Chen San, Zhou Xuedong, Wu Jiayuan. Effect of exosomes and the preconditioning method on pulp regeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 2105-2113. |
| [9] | Fan Yongjing, Wang Shu, Jin Wulong. Characteristics, advantages and application of osteogenic differentiation of jaw bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 100-106. |
| [10] | Wei Yurou, Tian Jiaqing, He Xianshun, Zhan Zhiwei, Wei Tengfei, Lin Tianye, He Wei, Wei Qiushi. Effect of lentiviral silencing of Piezo1 on osteogenic differentiation and TAZ expression in human bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 12-19. |
| [11] | Zhang Yuanshu, He Xu, Xue Yuan, Jin Yesheng, Wang Kai, Shi Qin, Rui Yongjun. Irisin alleviates palmitic acid-induced osteogenic inhibition in bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 26-31. |
| [12] | Zhou Minghua, Hu Xiaoyu. LncRNA SNHG4 regulates miR-152-3p during osteoblastic differentiation of periodontal ligament stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 38-43. |
| [13] | Yang Zhishan, Tang Zhenglong. YAP/TAZ, a core factor of the Hippo signaling pathway, is involved in bone formation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1264-1271. |
| [14] | Liu Wentao, Feng Xingchao, Yang Yi, Bai Shengbin. Effect of M2 macrophage-derived exosomes on osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 840-845. |
| [15] | Long Yanming, Xie Mengsheng, Huang Jiajie, Xue Wenli, Rong Hui, Li Xiaojie. Casein kinase 2-interaction protein-1 regulates the osteogenic ability of bone marrow mesenchymal stem cells in osteoporosis rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 878-882. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||