Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (5): 942-950.doi: 10.12307/2025.248
Previous Articles Next Articles
Effect of pravastatin on functional recovery from sciatic nerve crush injury in rats
Liu Zan1, 2, An Ran1, Li Baocheng2
- 1Baotou Medical College of Inner Mongolia University of Science and Technology, Baotou 014000, Inner Mongolia Autonomous Region, China; 2Department of Hand, Foot and Ankle Surgery, The First Affiliated Hospital of Baotou Medical College, Inner Mongolia University of Science and Technology, Baotou 014010, Inner Mongolia Autonomous Region, China
-
Received:2024-01-10Accepted:2024-02-22Online:2025-02-18Published:2024-06-03 -
Contact:Li Baocheng, Professor, Chief physician, Department of Hand, Foot and Ankle Surgery, The First Affiliated Hospital of Baotou Medical College, Inner Mongolia University of Science and Technology, Baotou 014010, Inner Mongolia Autonomous Region, China -
About author:Liu Zan, Master candidate, Baotou Medical College of Inner Mongolia University of Science and Technology, Baotou 014000, Inner Mongolia Autonomous Region, China; Department of Hand, Foot and Ankle Surgery, The First Affiliated Hospital of Baotou Medical College, Inner Mongolia University of Science and Technology, Baotou 014010, Inner Mongolia Autonomous Region, China An Ran, Master candidate, Baotou Medical College of Inner Mongolia University of Science and Technology, Baotou 014000,Inner Mongolia Autonomous Region, China Liu Zan and An Ran contributed equally to this work. -
Supported by:Graduate Student Research and Innovation Program of Baotou Medical College, No. bycx2023013 (to AR)
CLC Number:
Cite this article
Liu Zan, An Ran, Li Baocheng. Effect of pravastatin on functional recovery from sciatic nerve crush injury in rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 942-950.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
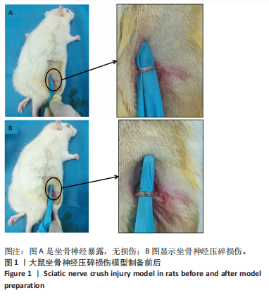
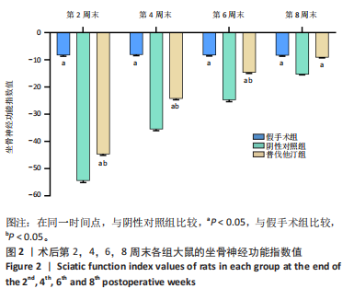
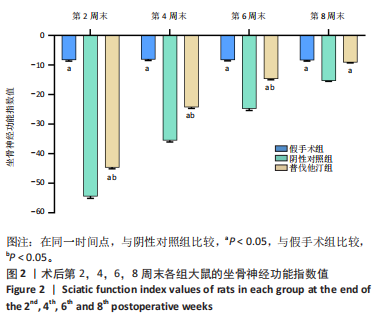
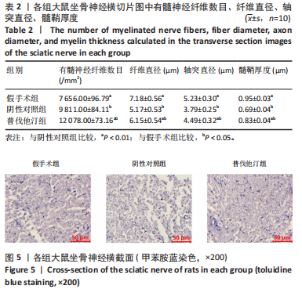
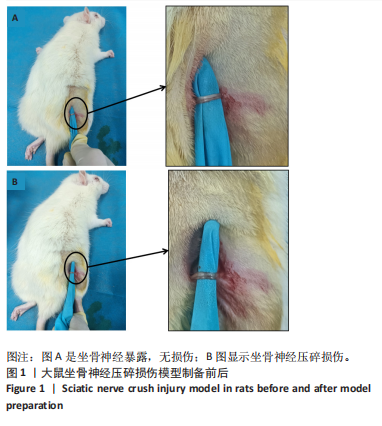
2.1 术后各组大鼠一般情况观察 术后观察发现,除假手术组外,其余两组大鼠饮水、进食明显减少,右脚不能运动,脚趾聚拢,不能完全展开,精神差。术后约7 d各组大鼠皮肤切口完全愈合。阴性对照组个别大鼠有自残行为发生(右脚部分脚趾被啃食)。术后8周取材时发现阴性对照组和普伐他汀组神经断端已对接。 2.2 术后各组大鼠坐骨神经功能指数的变化情况 术后第2,4,6,8周末通过测定坐骨神经功能指数来评估大鼠坐骨神经功能恢复情况,见图2。假手术组各时间点坐骨神经功能指数评分都高于-10,表明坐骨神经功能正常。术后第2周末,阴性对照组和普伐他汀组平均坐骨神经功能指数数值都降到最低,表明两组坐骨神经功能严重丧失。随着术后时间延长,普伐他汀组和阴性对照组的"
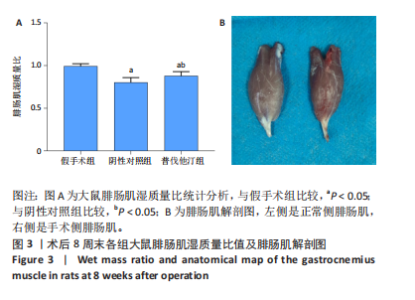
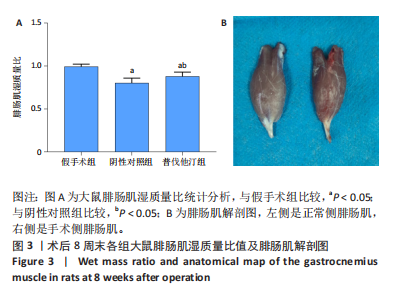
坐骨神经功能指数数值都在逐渐升高,表明神经功能都在逐步恢复。与假手术组相比,普伐他汀组在第2,4,6周末坐骨神经功能指数数值均较小(P < 0.05),表示坐骨神经功能还未完全恢复,在第8周末普伐他汀组坐骨神经功能指数评分与假手术组相当,都高于-10,差别无显著性意义,表示坐骨神经功能已恢复到接近正常水平。在同一测量时间点与阴性对照组相比,普伐他汀组坐骨神经功能指数数值更大(P < 0.05),说明普伐他汀组功能恢复更快。以上结果表明,普伐他汀的治疗加速了坐骨神经压碎损伤后的神经再生。 2.3 腓肠肌湿质量比 坐骨神经支配大腿后部的肌肉,神经损伤后会导致靶肌肉发生失神经萎缩,神经再生后对肌肉进行重新支配,可以减轻萎缩。通过测量术后8周大鼠腓肠肌湿质量比,来评估腓肠肌的失神经萎缩情况,见图3。与假手术组相比,普伐他汀组和阴性对照组腓肠肌湿质量比数值均较低(P < 0.05),说明神经损伤后,损伤侧腓肠肌发生了不同程度的失神经萎缩。但是,与阴性对照组相比,普伐他汀组的腓肠肌湿质量比数值更高(P < 0.05)且与假手术组接近。说明术后经过普伐他汀的治疗,肌肉萎缩程度有所降低。以上结果表明,普伐他汀减轻了坐骨神经压碎损伤后的失神经肌萎缩。 "
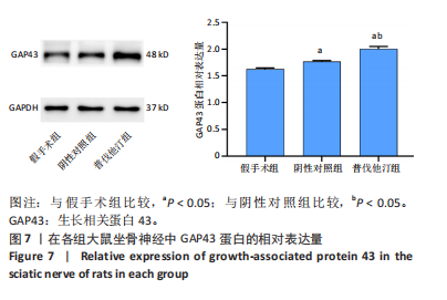
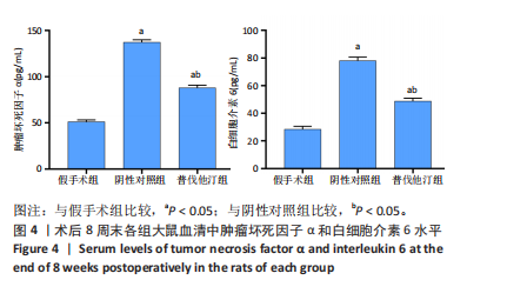
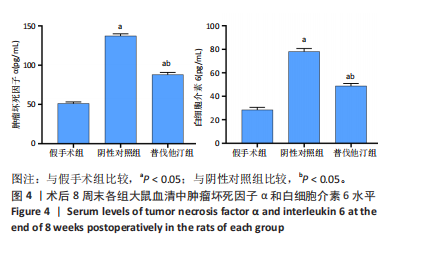
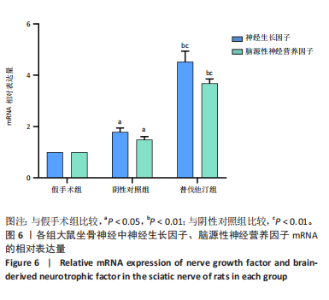
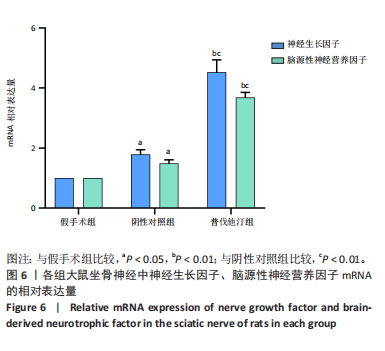
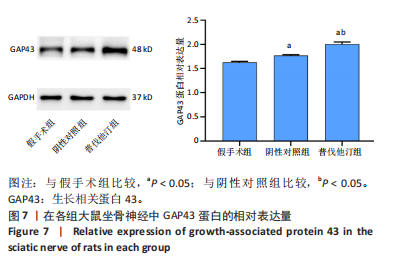
与假手术组比较,普伐他汀组和阴性对照组神经生长因子、脑源性神经营养因子相对表达量显著增加(P < 0.05或P < 0.01)。表明神经损伤后神经营养因子的分泌显著增加。与阴性对照组比较,普伐他汀组神经生长因子、脑源性神经营养因子相对表达量更高(P < 0.05或P < 0.01)。表明普伐他汀的治疗促进了神经生长因子、脑源性神经营养因子的分泌。以上结果表明,坐骨神经损伤后,神经生长因子、脑源性神经营养因子的分泌增加,而普伐他汀治疗增强了神经生长因子、脑源性神经营养因子的分泌水平。 2.7 Western blot法检测坐骨神经组织中GAP43蛋白的表达情况 GAP43是突触前膜蛋白,在调节突触再生和功能中起着重要作用。GAP43蛋白的表达情况见图7。与假手术组比较,普伐他汀组和阴性对照组GAP43蛋白相对表达量增加(P < 0.05),说明在神经损伤处发生了突触再生。与阴性对照组比较,普伐他汀组GAP43蛋白相对表达量更高 (P < 0.05),说明普伐他汀对神经损伤处突触再生具有促进作用。以上结果表明,神经损伤后损伤处有突触再生情况,而普伐他汀通过某些途径加速了突触的再生。"
| [1] KAPLAN B, LEVENBERG S. The Role of Biomaterials in Peripheral Nerve and Spinal Cord Injury: A Review. Int J Mol Sci. 2022;23(3):1244. [2] LOPES B, SOUSA P, ALVITES R,et al. Peripheral Nerve Injury Treatments and Advances: One Health Perspective. Int J Mol Sci. 2022;23(2):918. [3] ZHANG M, LI L, AN H, et al. Repair of Peripheral Nerve Injury Using Hydrogels Based on Self-Assembled Peptides. Gels. 2021;7(4):152. [4] PFISTER BJ, GORDON T, LOVERDE JR,et al. Biomedical engineering strategies for peripheral nerve repair: surgical applications, state of the art, and future challenges. Crit Rev Biomed Eng. 2011;39(2):81-124. [5] SLAVIN BR, SARHANE KA, VON GUIONNEAU N, et al. Insulin-Like Growth Factor-1: A Promising Therapeutic Target for Peripheral Nerve Injury. Front Bioeng Biotechnol. 2021;9:695850. [6] FERDOWSI S, ABDOLMALEKI A, ASADI A,et al. Effect of Azithromycin on Sciatic Nerve Injury in the Wistar Rats. Neurochem Res. 2023;48(1): 161-171. [7] DIVAC N, AKSIĆ M, RASULIĆ L, et al. Pharmacology of repair after peripheral nerve injury. Int J Clin Pharmacol Ther. 2021;59(6):447-462. [8] HUANG W, YI S, ZHAO L. Genetic Features of Young and Aged Animals After Peripheral Nerve Injury: Implications for Diminished Regeneration Capacity. Cell Mol Neurobiol. 2023;43(8):4363-4375. [9] SIDHU G, SAPRA A. Pravastatin. 2023 Jun 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. [10] SOLHEIM S, SELJEFLOT I, ARNESEN H, et al. Reduced levels of TNF alpha in hypercholesterolemic individuals after treatment with pravastatin for 8 weeks. Atherosclerosis. 2001;157(2):411-415. [11] SOMMEIJER DW, MACGILLAVRY MR, MEIJERS JC,et al. Anti-inflammatory and anticoagulant effects of pravastatin in patients with type 2 diabetes. Diabetes Care. 2004;27(2):468-473. [12] LU P, LIU J, PANG X. Pravastatin inhibits fibrinogen- and FDP-induced inflammatory response via reducing the production of IL-6, TNF-α and iNOS in vascular smooth muscle cells. Mol Med Rep. 2015;12(4):6145-6151. [13] SATO F, WAJIMA D, TAKESHIMA Y, et al. Neuroprotective effects of pravastatin in cerebral venous infarction in a rat model. IBRO Neurosci Rep. 2023;14:202-209. [14] MAZARD T, RITZENTHALER T, DAILLER F. Pravastatin may improve neurological outcome following low-grade aneurysmal subarachnoid hemorrhage. J Clin Neurosci. 2022;98:11-14. [15] BERGER C, XIA F, MAURER MH, et al. Neuroprotection by pravastatin in acute ischemic stroke in rats. Brain Res Rev. 2008;58(1):48-56. [16] YALÇıNKAYA B, OCAK H, ÇOLAK AF, et al. Sciatic neurotmesis and periostitis ossificans progressiva due to a traumatic/unexpected glass injury: a case report. J Yeungnam Med Sci. 2024;41(1):45-47. [17] HUSSAIN G, WANG J, RASUL A,et al. Current Status of Therapeutic Approaches against Peripheral Nerve Injuries: A Detailed Story from Injury to Recovery. Int J Biol Sci. 2020;16(1):116-134. [18] VIJAYAVENKATARAMAN S. Nerve guide conduits for peripheral nerve injury repair: A review on design, materials and fabrication methods. Acta Biomater. 2020;106:54-69. [19] LIU X, DUAN X. Mechanisms and Treatments of Peripheral Nerve Injury. Ann Plast Surg. 2023;91(2):313-318. [20] ZIMMERMANN KS, AMAN M, HARHAUS L, et al. Improving outcomes in traumatic peripheral nerve injuries to the upper extremity. Eur J Orthop Surg Traumatol. 2023 Oct 21. doi: 10.1007/s00590-023-03751-3. [21] SAFA B, JAIN S, DESAI MJ, et al. Peripheral nerve repair throughout the body with processed nerve allografts: Results from a large multicenter study. Microsurgery. 2020;40(5):527-537. [22] PEREIRA C, LAZAR SV, WANG A. Bioengineering approaches for nerve graft revascularization: Current concepts and future directions. WIREs Mech Dis. 2023;15(4):e1609. [23] YU T, AO Q, AO T, et al. Preparation and assessment of an optimized multichannel acellular nerve allograft for peripheral nerve regeneration. Bioeng Transl Med. 2022;8(4):e10435. [24] LOVATI AB, D’ARRIGO D, ODELLA S,et al. Nerve Repair Using Decellularized Nerve Grafts in Rat Models. A Review of the Literature. Front Cell Neurosci. 2018;12:427. [25] BOLANDGHAMAT S, BEHNAM-RASSOULI M. Recent Findings on the Effects of Pharmacological Agents on the Nerve Regeneration after Peripheral Nerve Injury. Curr Neuropharmacol. 2020;18(11):1154-1163. [26] DAIMON M, AOMI S, KAWAMATA T,et al. Pravastatin, a 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, reduces delayed neuronal death following transient forebrain ischemia in the adult rat hippocampus. Neurosci Lett. 2004;362(2):122-126. [27] TRAMONTINA AC, WARTCHOW KM, RODRIGUES L,et al. The neuroprotective effect of two statins: simvastatin and pravastatin on a streptozotocin-induced model of Alzheimer’s disease in rats. J Neural Transm (Vienna). 2011;118(11):1641-1649. [28] AL-SAEDI HF, PANAHI Y, GHANIMI HA,et al. Enhancement of nerve regeneration with nimodipine treatment after sciatic nerve injury. Fundam Clin Pharmacol. 2023;37(1):107-115. [29] SHAN C, ZHANG C, ZHANG C. The Role of IL-6 in Neurodegenerative Disorders. Neurochem Res. 2024 Jan 16. doi: 10.1007/s11064-023-04085-6. [30] KOULAXOUZIDIS G, REIM G, FLUHR JW,et al. In Situ Deactivation of Interleukin-6 Enhances Early Peripheral Nerve Regeneration in a Murine Injury Model. J Reconstr Microsurg. 2015;31(7):508-515. [31] HUANG Z, ZHONG L, ZHU J,et al. Inhibition of IL-6/JAK/STAT3 pathway rescues denervation-induced skeletal muscle atrophy. Ann Transl Med. 2020;8(24):1681. [32] IDRISS HT, NAISMITH JH.TNF alpha and the TNF receptor superfamily: structure-function relationship(s). MicroscResTech. 2000;50(3):184-195. [33] URABE H, TERASHIMA T, LIN F, et al. Bone marrow-derived TNF-α causes diabetic neuropathy in mice. Diabetologia. 2015;58(2):402-410. [34] LORENZINI L, BALDASSARRO VA, STANZANI A,et al. Nerve Growth Factor: The First Molecule of the Neurotrophin Family. Adv Exp Med Biol. 2021;1331:3-10. [35] KOPACH O, PAVLOV AM, SINDEEVA OA, et al. Biodegradable Microcapsules Loaded with Nerve Growth Factor Enable Neurite Guidance and Synapse Formation. Pharmaceutics. 2020;13(1):25. [36] MIZUSHIMA N, KOMATSU M. Autophagy: renovation of cells and tissues. Cell. 2011;147(4):728-741. [37] DODSON M, WANI WY, REDMANN M, et al. Regulation of autophagy, mitochondrial dynamics, and cellular bioenergetics by 4-hydroxynonenal in primary neurons. Autophagy. 2017;13(11): 1828-1840. [38] LI R, LI D, WU C, et al. Nerve growth factor activates autophagy in Schwann cells to enhance myelin debris clearance and to expedite nerve regeneration. Theranostics. 2020;10(4):1649-1677. [39] FLETCHER JL, MURRAY SS, XIAO J. Brain-Derived Neurotrophic Factor in Central Nervous System Myelination: A New Mechanism to Promote Myelin Plasticity and Repair. Int J Mol Sci. 2018;19(12):4131. [40] ARANAZ I, ACOSTA N, REVUELTA J, et al. Fast and Sustained Axonal Growth by BDNF Released from Chitosan Microspheres. Mar Drugs. 2023;21(2):91. [41] LAN G, DU J, CHEN X,et al. Association of APOE-ε4 and GAP-43-related presynaptic loss with β-amyloid, tau, neurodegeneration, and cognitive decline. Neurobiol Aging. 2023;132:209-219. [42] SHI LF, WANG CJ, YU KW, et al. An Enriched Environment Promotes Motor Function through Neuroprotection after Cerebral Ischemia. Biomed Res Int. 2023;2023:4143633. [43] CHATO-ASTRAIN J, RODA O, SÁNCHEZ-PORRAS D, et al. Peripheral nerve regeneration through nerve conduits evokes differential expression of growth-associated protein-43 in the spinal cord. Neural Regen Res. 2023;18(8):1852-1856. [44] MANKAVI F, IBRAHIM R, WANG H. Advances in Biomimetic Nerve Guidance Conduits for Peripheral Nerve Regeneration. Nanomaterials (Basel). 2023;13(18):2528. [45] WU X, LI H, YIN J, et al. [Experimental study on the construction of telmisartan/collagen/polycaprolactone nerve conduit and its repair effect on rat sciatic nerve defect]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36(3):352-361. [46] LI Y, KAMEI Y, KAMBE M, et al. Peripheral Nerve Regeneration Using Different Germ Layer-Derived Adult Stem Cells in the Past Decade. Behav Neurol. 2021;2021:5586523. |
| [1] | Chen Yuning, Jiang Ying, Liao Xiangyu, Chen Qiongjun, Xiong Liang, Liu Yue, Liu Tong. Buqi Huoxue Compounds intervene with the expression of related factors and autophagy related proteins in a rat model of cerebral ischemia/reperfusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1152-1158. |
| [2] | Zhao Xiaoxuan, Liu Shuaiyi, Li Qi, Xing Zheng, Li Qingwen, Chu Xiaolei. Different exercise modalities promote functional recovery after peripheral nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1248-1256. |
| [3] | Shui Jing, He Yu, Jiang Nan, Xu Kun, Song Lijuan, Ding Zhibin, Ma Cungen, Li Xinyi. Astrocytes regulate remyelination in central nervous system [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7889-7897. |
| [4] | Zhao Xiaoxuan, Liu Shuaiyi, Xing Zheng, Li Qingwen, Chu Xiaolei, Li Qi. Research hotspots and trends in application of tissue engineering in peripheral nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6591-6600. |
| [5] | Wang Jiaru, Zhang Ying, Yang Yong, Qi Wen, Xiao Huaye, Ma Qiuping, Yang Lianzhao, Luo Ziwei, He Yaqing, Zhang Jiangyin, Wei Jiawen, Meng Yuan, Tan Silian. Systematic review of machine learning models for predicting functional recovery and prognosis in stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6317-6325. |
| [6] | Lei Senlin, Chen Xiaoan, Chen Ping, Wang Zhaofeng. Exercise prevention and treatment of Parkinson’ s disease mediated by brain-derived neurotrophic factor: role and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5454-5468. |
| [7] | Deng Yiran, Wang Xianliang, Li Dandan. Meta-analysis of exercise intervention on cardiopulmonary function in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5203-5211. |
| [8] | Tian Liangliang, Zhou Rui, Cao Guangzhao, Zhang Jingjing. Action mechanism of Coptidis Rhizoma Alkaloids against cerebral ischemia based on transcriptome sequencing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(19): 4161-4171. |
| [9] | Zhao Liping, Chen Yibo, Wang Yaqian, Li Zhitong, Zhang Qi, Gou Bo. Mechanism of central analgesia in rats with myofascial pain syndrome by intervention of “trigger points” with stagnant moving needles [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3614-3623. |
| [10] | Liu Minqi, Gao Mingwei, Chu Xiaolei, Xing Zheng, Li Shihao, Ding Ning, Li Yajie, Li Qi . Different frequencies of electrical stimulation promote recovery from peripheral nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(14): 3061-3069. |
| [11] | Duan Kunling, Fei Jing, Li Leiji. Autophagy protects neurons against facial nerve injury in rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4378-4382. |
| [12] | Liu Xinxin, Geng Zhizhong, Chen Jian. Effects of high-intensity interval training with different intervention durations on cognitive function in older adults: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2282-2289. |
| [13] | Li Jingxuan, Shi Dai, Wu Guofeng. Regulatory effects of cAMP response element-binding protein on hippocampal brain-derived neurotrophic factor level in a rat model of drug-resistant epilepsy [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(35): 5659-5664. |
| [14] | Ma Ruixin, Liu Pan, Zhang Qiong, Zeng Gaofeng, Zong Shaohui. Molecular mechanism of total flavonoids of hawthorn leaves regulating astrocytes to repair spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(33): 5327-5333. |
| [15] | Xu Xingxing, Wen Chaoju, Li Ying, Meng Maohua, Wang Qinying, Chen Jingqiao, Dong Qiang. Effect of silane coupling agent composite graphene oxide coating on biological behavior of Schwann cells on pure titanium [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(30): 4783-4789. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||