Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (5): 951-957.doi: 10.12307/2025.277
Previous Articles Next Articles
Compressive stress induces degeneration of cartilaginous endplate cells through the SOST/Wnt/beta-catenin pathway
Xiang Pan1, Che Yanjun2, Luo Zongping1
- 1Department of Orthopaedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China; 2Orthopedics and Sports Medicine Center, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou 215000, Jiangsu Province, China
-
Received:2024-01-02Accepted:2024-02-21Online:2025-02-18Published:2024-06-03 -
Contact:Luo Zongping, MD, Professor, Department of Orthopaedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China Co-corresponding author: Che Yanjun, MD, Associate chief physician, Master’s supervisor, Orthopedics and Sports Medicine Center, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou 215000, Jiangsu Province, China -
About author:Xiang Pan, Master candidate, Department of Orthopaedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China -
Supported by:National Natural Science Foundation of China, No. 32071307 (to LZP); Jiangsu Provincial Higher Education Key Discipline Construction Project (PAPD) (to LZP); Suzhou Science and Technology Bureau Project, No. SKY2022185 (to CYJ); Gusu Health Talent Program Talent Research Project, No. GSWS2021035 (to CYJ); Scientific Research Fund for Integrative Medicine of Suzhou City, No. SKYD:2023254 (to CYJ)
CLC Number:
Cite this article
Xiang Pan, Che Yanjun, Luo Zongping. Compressive stress induces degeneration of cartilaginous endplate cells through the SOST/Wnt/beta-catenin pathway[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 951-957.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

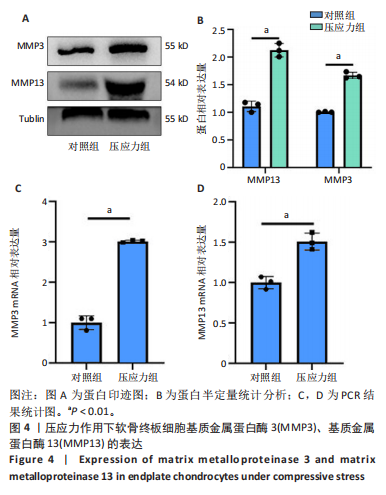
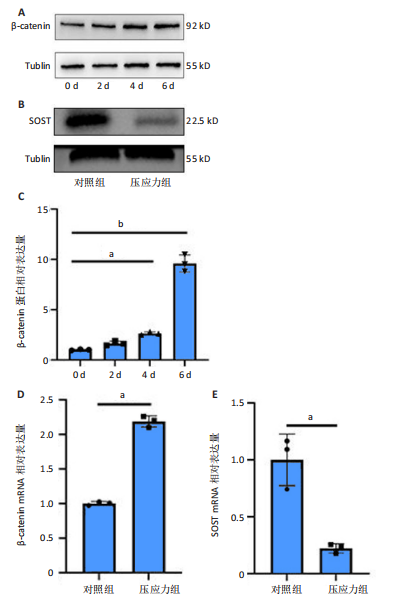
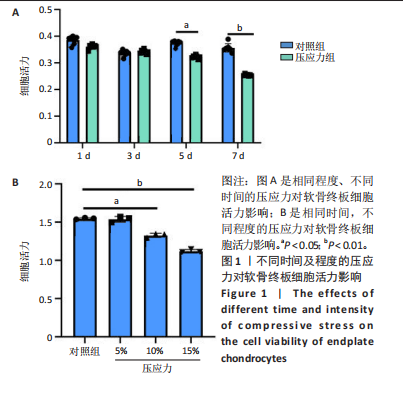
2.1 压应力诱导软骨终板细胞活力降低 CCK-8结果显示,在受到10%形变压应力的作用下,软骨终板细胞在前几天的细胞活力与对照组相比没有明显差异。然而,在第5天时,压应力组的细胞活力开始出现轻微下降,并且在第7天时,与对照组相比,细胞活力的差异进一步增大(P < 0.01,图1A)。测试了在不同强度(0%,5%,10%,15%)下压应力对软骨终板细胞的影响,结果显示,随着压应力强度的增加,压应力组的细胞活性逐渐降低(P < 0.05或< 0.01,图1B)。这表明压应力程度对软骨终板细胞的生理功能产生了显著的影响。结果说明,压应力对软骨终板细胞的影响是与其形变程度和作用时间密切相关的,在较低程度的压应力下,细胞活力可能没有明显的改变,但随着压应力的增加,细胞活性逐渐下降。 2.2 压应力诱导软骨终板细胞退变 Western blot分析观察到在压应力组中,软骨终板细胞中聚集蛋白聚糖和Ⅱ型胶原的蛋白水平较对照组明显降低(P < 0.01);RT-qPCR结果也显示,在压应力组中,软骨终板细胞中聚集蛋白聚糖和Ⅱ型胶原的基因表达水平显著下调(P < 0.05或< 0.01)。结果表明,压应力的作用对软骨终板细胞的软骨标记物的表达产生了抑制作用,见图2。 2.3 压应力诱导软骨终板细胞钙化 利用Western blot和RT-qPCR技术检测了在压应力作用下软骨终板细胞中钙化相关因子(Runx2、骨钙素)的变化情况。Western blot分析发现在压应力组中,软骨终板细胞中Runx2和骨钙素的蛋白水平较对照组明显升高(P < 0.05或< 0.01);RT-qPCR结果也显示,在压应力组中,软骨终板细胞中Runx2和骨钙素的基因表达水平显著上调(P < 0.01,图3)。结果提示,压应力的作用可以刺激软骨终板细胞中钙化相关因子的表达增加。 2.4 压应力促进软骨终板细胞外基质降解增加 Western blot分析发现在压应力组中,软骨终板细胞中基质金属蛋白酶3和基质金属蛋白酶13的蛋白水平较对照组明显升高(P < 0.01);RT-qPCR结果也显示,在压应力组中,软骨终板细胞中两种基质金属蛋白酶的基因表达水平显著上调"
| [1] BUCHBINDER R, VAN TULDER M, OBERG B, et al. Low back pain: a call for action. Lancet. 2018;391(10137):2384-2388. [2] HARTVIGSEN J, HANCOCK MJ, KONGSTED A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367. [3] FONTANA G, SEE E, PANDIT A. Current trends in biologics delivery to restore intervertebral disc anabolism. Adv Drug Deliv Rev. 2015;84: 146-158. [4] JIANG LB, CAO L, YIN XF, et al. Activation of autophagy via Ca(2+)-dependent AMPK/mTOR pathway in rat notochordal cells is a cellular adaptation under hyperosmotic stress. Cell Cycle. 2015;14(6):867-879. [5] WALTER BA, KORECKI CL, PURMESSUR D, et al. Complex loading affects intervertebral disc mechanics and biology. Osteoarthritis Cartilage. 2011;19(8):1011-1018. [6] GULLBRAND SE, PETERSON J, AHLBORN J, et al. ISSLS Prize Winner: Dynamic Loading-Induced Convective Transport Enhances Intervertebral Disc Nutrition. Spine (Phila Pa 1976). 2015;40(15):1158-1164. [7] CHE YJ, LI HT, LIANG T, et al. Intervertebral disc degeneration induced by long-segment in-situ immobilization: a macro, micro, and nanoscale analysis. BMC Musculoskelet Disord. 2018;19(1):308. [8] GULLBRAND SE, PETERSON J, MASTROPOLO R, et al. Drug-induced changes to the vertebral endplate vasculature affect transport into the intervertebral disc in vivo. J Orthop Res. 2014;32(12):1694-1700. [9] MALANDRINO A, LACROIX D, HELLMICH C, et al. The role of endplate poromechanical properties on the nutrient availability in the intervertebral disc. Osteoarthritis Cartilage. 2014;22(7):1053-1060. [10] DOLAN P, LUO J, POLLINTINE P, et al. Intervertebral disc decompression following endplate damage: implications for disc degeneration depend on spinal level and age. Spine. 2013;38(17):1473-1481. [11] DURAN S, CAVUSOGLU M, HATIPOGLU HG, et al. Association Between Measures of Vertebral Endplate Morphology and Lumbar Intervertebral Disc Degeneration. Can Assoc Radiol J. 2017;68(2):210-216. [12] ZEHRA U, ROBSON-BROWN K, ADAMS MA, et al. Porosity and Thickness of the Vertebral Endplate Depend on Local Mechanical Loading. Spine. 2015;40(15):1173-1180. [13] TOMASZEWSKI KA, SAGANIAK K, GŁADYSZ T, et al. The biology behind the human intervertebral disc and its endplates. Folia Morphol (Warsz). 2015;74(2):157-168. [14] XIA DD, LIN SL, WANG XY, et al. Effects of shear force on intervertebral disc: an in vivo rabbit study. Eur Spine J. 2015;24(8):1711-1719. [15] SENGUPTA DK, FAN H. The basis of mechanical instability in degenerative disc disease: a cadaveric study of abnormal motion versus load distribution. Spine. 2014;39(13):1032-1043. [16] CHE YJ, GUO JB, LIANG T, et al. Controlled immobilization-traction based on intervertebral stability is conducive to the regeneration or repair of the degenerative disc: an in vivo study on the rat coccygeal model. Spine J. 2019;19(5):920-930. [17] DING L, JIANG Z, WU J, et al. β‑catenin signalling inhibits cartilage endplate chondrocyte homeostasis in vitro. Mol Med Rep. 2019;20(1): 567-572. [18] XU Y, HE J, HE J. Cyanidin attenuates the high hydrostatic pressure-induced degradation of cellular matrix of nucleus pulposus cell via blocking the Wnt/β-catenin signaling. Tissue Cell. 2022;76:101798. [19] SONG Q, ZHANG F, WANG K, et al. MiR-874-3p plays a protective role in intervertebral disc degeneration by suppressing MMP2 and MMP3. Eur J Pharmacol.2021; 895: 173891. [20] XU HG, ZHENG Q, SONG JX, et al. Intermittent cyclic mechanical tension promotes endplate cartilage degeneration via canonical Wnt signaling pathway and E-cadherin/β-catenin complex cross-talk. Osteoarthritis Cartilage. 2016;24(1):158-168. [21] ROBLING AG, NIZIOLEK PJ, BALDRIDGE LA, et al. Mechanical stimulation of bone in vivo reduces osteocyte expression of Sost/sclerostin]. J Biol Chem. 2008;283(9):5866-5875. [22] HEILAND GR, ZWERINA K, BAUM W, et al. Neutralisation of Dkk-1 protects from systemic bone loss during inflammation and reduces sclerostin expression. Ann Rheum Dis. 2010;69(12):2152-2159. [23] CHANG JC, CHRISTIANSEN BA, MURUGESH DK, et al.SOST/Sclerostin Improves Posttraumatic Osteoarthritis and Inhibits MMP2/3 Expression After Injury. J Bone Miner Res. 2018;33(6):1105-1113. [24] LIAO H, ZHANG Z, LIU Z, et al. Inhibited microRNA-218-5p attenuates synovial inflammation and cartilage injury in rats with knee osteoarthritis by promoting sclerostin. Life Sci. 2021;267:118893. [25] XU HG, ZHENG Q, SONG JX, et al. Intermittent cyclic mechanical tension promotes endplate cartilage degeneration via canonical Wnt signaling pathway and E-cadherin/β-catenin complex cross-talk. Osteoarthritis Cartilage. 2016;24(1):158-168. [26] ARIGA K, MIYAMOTO S, NAKASE T, et al. The relationship between apoptosis of endplate chondrocytes and aging and degeneration of the intervertebral disc. Spine. 2001;26(22):2414-2420. [27] GAWRI R, ROSENZWEIG D H, KROCK E, et al. High mechanical strain of primary intervertebral disc cells promotes secretion of inflammatory factors associated with disc degeneration and pain. Arthritis Res Ther. 2014;16(1):R21. [28] ALKHATIB B, ROSENZWEIG DH, KROCK E, et al. Acute mechanical injury of the human intervertebral disc: link to degeneration and pain. Eur Cell Mater. 2014;28:98-110; discussion 110-111. [29] VERGROESEN PPA, KINGMA I, EMANUEL KS, et al. Mechanics and biology in intervertebral disc degeneration: a vicious circle. Osteoarthritis Cartilage. 2015;23(7):1057-1070. [30] FENG C, LIU M, FAN X, et al. Intermittent cyclic mechanical tension altered the microRNA expression profile of human cartilage endplate chondrocytes. Mol Med Rep. 2018;17(4):5238-5246. [31] CHE YJ, GUO JB, LIANG T, et al. Assessment of changes in the micro-nano environment of intervertebral disc degeneration based on Pfirrmann grade. Spine J. 2019;19(7):1242-1253. [32] PRAXENTHALER H, KRäMER E, WEISSER M, et al. Extracellular matrix content and WNT/β-catenin levels of cartilage determine the chondrocyte response to compressive load. Biochim Biophys Acta Mol Basis Dis. 2018;1864(3):851-859. [33] JIANG YY, WEN J, GONG C, et al. BIO alleviated compressive mechanical force-mediated mandibular cartilage pathological changes through Wnt/β-catenin signaling activation. J Orthop Res. 2018;36(4):1228-1237. [34] SHI H, ZHOU K, WANG M, et al. Integrating physicomechanical and biological strategies for BTE: biomaterials-induced osteogenic differentiation of MSCs. Theranostics. 2023;13(10):3245-3275. [35] ZHU Z, TANG T, HE Z, et al. Uniaxial cyclic stretch enhances osteogenic differentiation of OPLL-derived primary cells via YAP-Wnt/β-catenin axis. Eur Cell Mater. 2023;45:31-45. [36] GOULD NR, LESER JM, TORRE OM, et al. In vitro Fluid Shear Stress Induced Sclerostin Degradation and CaMKII Activation in Osteocytes. Bio Protoc. 2021;11(23):e4251. [37] LIN C, JIANG X, DAI Z, et al. Sclerostin mediates bone response to mechanical unloading through antagonizing Wnt/beta-catenin signaling. J Bone Miner Res. 2009;24(10):1651-1661. [38] KROON T, BHADOURIA N, NIZIOLEK P, et al. Suppression of Sost/Sclerostin and Dickkopf-1 Augment Intervertebral Disc Structure in Mice. J Bone Miner Res. 2022;37(6):1156-1169. [39] YAN JY, TIAN FM, WANG WY, et al. Parathyroid hormone (1-34) prevents cartilage degradation and preserves subchondral bone micro-architecture in guinea pigs with spontaneous osteoarthritis. Osteoarthritis Cartilage. 2014;22(11):1869-1877. |
| [1] | Zhao Jiyu, Wang Shaowei. Forkhead box transcription factor O1 signaling pathway in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1923-1930. |
| [2] | Yin Lu, Jiang Chuanfeng, Chen Junjie, Yi Ming, Wang Zihe, Shi Houyin, Wang Guoyou, Shen Huarui. Effect of Complanatoside A on the apoptosis of articular chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1541-1547. |
| [3] | Liu Qi, Li Linzhen, Li Yusheng, Jiao Hongzhuo, Yang Cheng, Zhang Juntao. Icariin-containing serum promotes chondrocyte proliferation and chondrogenic differentiation of stem cells in the co-culture system of three kinds of cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1371-1379. |
| [4] | Yang Zhihang, Sun Zuyan, Huang Wenliang, Wan Yu, Chen Shida, Deng Jiang. Nerve growth factor promotes chondrogenic differentiation and inhibits hypertrophic differentiation of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1336-1342. |
| [5] | Qian Kun, Li Ziqing, Sun Shui . Endoplasmic reticulum stress in the occurrence and development of common degenerative bone diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1285-1295. |
| [6] | Lang Mecuo, Zhang Yilin, Wang Li. MiR-338-3p affects proliferation and apoptosis of alveolar bone osteoblasts by targeting receptor activator of nuclear factor-kappaB ligand [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 899-907. |
| [7] | Sima Xinli, Liu Danping, Qi Hui. Effect and mechanism of metformin-modified bone marrow mesenchymal stem cell exosomes on regulating chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7728-7734. |
| [8] | Ma Weibang, Xu Zhe, Yu Qiao, Ouyang Dong, Zhang Ruguo, Luo Wei, Xie Yangjiang, Liu Chen. Screening and cytological validation of cartilage degeneration-related genes in exosomes from osteoarthritis synovial fluid [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7783-7789. |
| [9] | Yin Hang, Song Kui. Effect of crocin hydrogel on chondrocytes and MC3T3-E1 cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7293-7300. |
| [10] | Yu Qinghe, Cai Ziming, Wu Jintao, Ma Pengfei, Zhang Xin, Zhou Longqian, Wang Yakun, Lin Xiaoqin, Lin Wenping. Vanillic acid inhibits inflammatory response and extracellular matrix degradation of endplate chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6391-9397. |
| [11] | Liu Ruojing, Zhao Xue, Zhu Yizhen, Fu Lingling, Zhu Junde. Ginsenoside Rb1 alleviates cerebral ischemic injury in mice by regulating microglial polarization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6219-6227. |
| [12] | An Xingqi, Li Wenjin. Mechanism of Notch signaling pathway regulating condylar cartilage development and temporomandibular joint inflammation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5673-5679. |
| [13] | Hu Enxi, He Wenying, Tao Xiang, Du Peijing, Wang Libin. Regulation of THZ1, an inhibitor of cyclin-dependent kinase 7, on stemness of glioma stem cells and its mechanism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5374-5381. |
| [14] | Liang Zhifeng, Yang Yingcai, Cheng Qiangang, Jia Yongxing, Wang Bo . Effect of stromal cell-derived factor-1 in cartilage and subchondral bone homeostasis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5422-5433. |
| [15] | Yan Pengan, Cai Yifan, Yan Zhenxing, Wei Yuqiao, Geng Bin, Xia Yayi. Role and influence of compressive stress on cells in vitro [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(23): 4993-5001. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||