Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (9): 1352-1358.doi: 10.12307/2023.212
Previous Articles Next Articles
Influence of different bone mineral densities on cage subsidence after stand-alone oblique lateral interbody fusion: three-dimensional finite element analysis
Wu Tianliang1, Tao Xiuxia2, Xu Hongguang3
- 1Department of Spine Surgery, 2Department of Nuclear Medicine, The Second People’s Hospital of Wuhu, East China Normal University, Wuhu 241001, Anhui Province, China; 3Spine Research Center, Department of Spine Surgery, Yijishan Hospital (First Affiliated Hospital), Wannan Medical College, Wuhu 241001, Anhui Province, China
-
Received:2021-12-14Accepted:2022-01-30Online:2023-03-28Published:2022-07-01 -
Contact:Xu Hongguang, Professor, Chief physician, Spine Research Center, Department of Spine Surgery, Yijishan Hospital (First Affiliated Hospital), Wannan Medical College, Wuhu 241001, Anhui Province, China -
About author:Wu Tianliang, MD, Associate chief physician, Department of Spine Surgery, The Second People’s Hospital of Wuhu, East China Normal University, Wuhu 241001, Anhui Province, China -
Supported by:National Natural Science Foundation of China, No. 81972108 (to XHG); the “Mountain Climbing” Cultivation Plan for the Technological Innovation Team of Yijishan Hospital of Wannan Medical College (Minimally Invasive Team for Lumbar Degenerative Diseases), No. PF2019007 (to XHG); the “Peak” Cultivation Plan of Scientific Research Capacity of Yijishan Hospital of Wannan Medical College, No. GF2019T02, GF2019G07, GF2019332 (to XHG)
CLC Number:
Cite this article
Wu Tianliang, Tao Xiuxia, Xu Hongguang. Influence of different bone mineral densities on cage subsidence after stand-alone oblique lateral interbody fusion: three-dimensional finite element analysis[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1352-1358.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
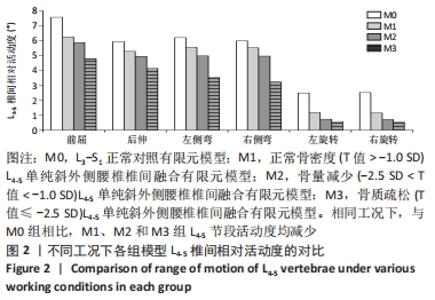
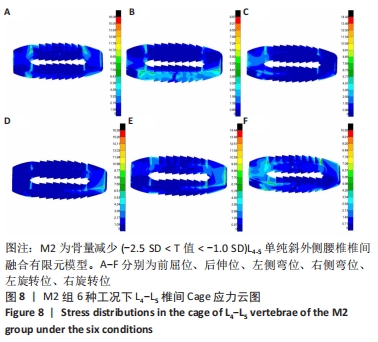
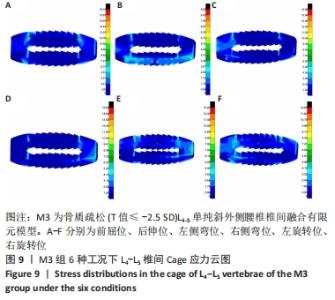
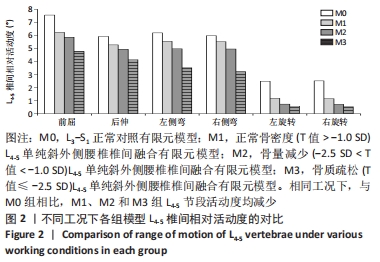
2.1 模型验证结果 为验证建模方法、正确设置、边界条件和建模假设是否合理和正确,在相同的载荷和约束条件下,对正常的L3-S1腰椎模型模拟前屈、后伸、左右侧弯、左右旋转下的腰椎生物力学特性,将体外实验和前人的研究结果与椎体每次运动的相对活动范围值进行比较[15-16],对数据进行定性和定量比较。此次研究所得活动范围相对转度数据在趋势和数值上与以往研究结果相近,可说明此次模型是有效、正确的,该L3-S1腰椎模型可用于后续生物力学研究(M1、M2、M3)和其他相关手术模型。 2.2 各组模型L4-5节段活动度比较 针对L3-S1各椎间相对活动度来说,6种不同运动状态下4组模型对应的各椎间相对活动度各不相同,其中L3-L4椎间相对活动度基本保持在2.83°-7.55°之间,L4-L5椎间相对活动度基本保持在0.52°-6.23°之间,L5-S1椎间相对活动度基本保持在1.43°-12.23°之间。 相较于M0组,L4-L5椎体间置入Cage融合器后,由于Cage融合器的弹性模量远比椎间盘高很多,间接地导致了L4-L5椎体刚度的增大,从而导致了L4-L5椎间相对活动度大幅度降低,各运动状态下的降幅为7.71%-79.28%。其中,L3-L4在后伸、左右旋转运动状态下的椎间相对活动度、L4-L5在左右旋转运动状态下的椎间相对活动度、L5-S1在前屈、右侧弯运动状态下的椎间相对活动度相对M0组变化幅度较为显著,尤其以M3组L4-L5椎间相对活动度降幅最大,为30.12%-79.28%;M1组与M2组在椎间相对活动度变化上相对较为接近,差异较小,见图2。 "
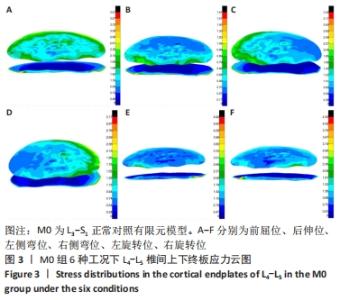
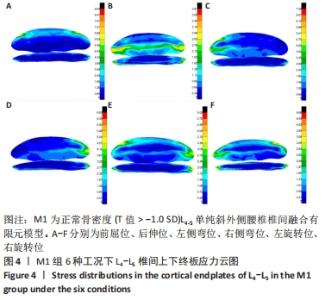
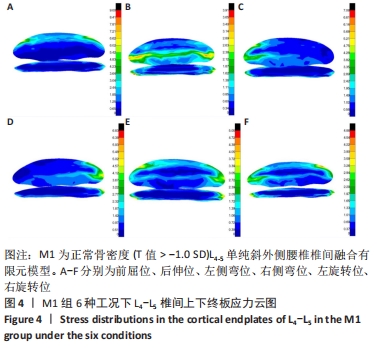
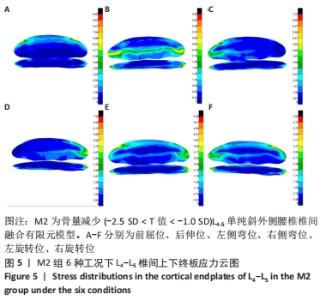
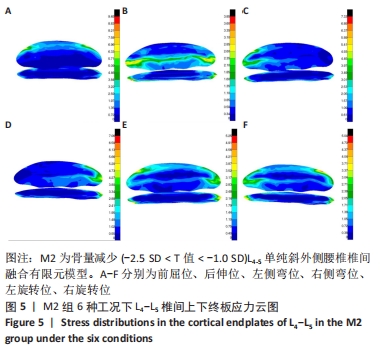
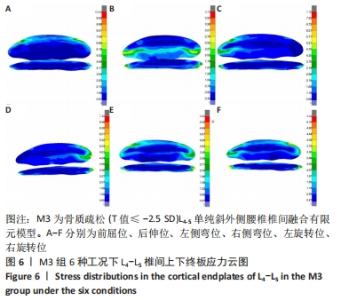
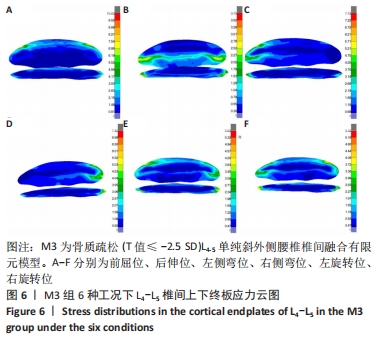
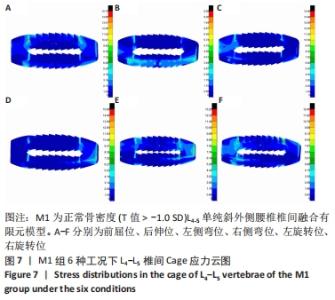
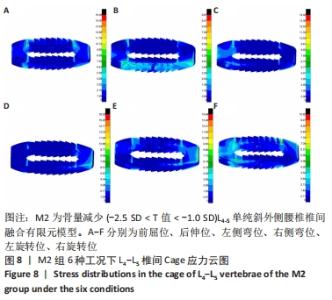
2.3 各组模型骨性终板应力比较 在6种运动状态下,4组模型L4下终板应力峰值在1.01-7.75 MPa之间,L5上终板应力峰值在1.61-10.23 MPa之间。相对M0组对应骨性终板应力而言,在L4-5间隙置入Cage对L4下终板、L5上终板的影响程度较显著,其中M1、M2、M3组在前屈、后伸、左右侧弯状态下的L4下终板应力增量分别为150.2%-257.4%、156.2%-264.4%、159.1%-252.5%,在前屈、后伸、左右侧弯状态下的L5上终板应力增量分别为113.3%-142.9%、120.8%-148.0%、132.5%-168.5%,且在左右旋转运动状态下L4下终板、L5上终板表现相对较为突出外,相对M0组的应力增量为92.6%-129.7%、2.6%-28.4%。相对M1组而言,M2组骨性终板应力增幅不明显,增幅约在5.9%以内;M3组骨性终板应力增加明显,应力增幅约在16.2%以内。4组L4-5上下骨性终板应力分布云图,见图3-6。"

| [1] SILVESTRE C, MAC-THIONG JM, HILMI R, et al. Complications and Morbidities of Mini-open Anterior Retroperitoneal Lumbar Interbody Fusion: Oblique Lumbar Interbody Fusion in 179 Patients. Asian Spine J. 2012;6(2):89-97. [2] MARCHI L, ABDALA N, OLIVEIRA L, et al. Radiographic and clinical evaluation of cage subsidence after standalone lateral interbody fusion. J Neurosurg Spine. 2013;19:110-118. [3] KOTHEERANURAK V, JITPAKDEE K, LIN GX, et al. Subsidence of Interbody Cage Following Oblique Lateral Interbody Fusion: An Analysis and Potential Risk Factors. Global Spine J. 2021;17:21925682211067210. [4] 沈俊宏,王建,刘超,等.斜外侧腰椎间融合术治疗退变性腰椎疾病的并发症和早期临床结果[J].中国脊柱脊髓杂志,2018,28(5): 397-404. [5] ZHANG QY, TAN J, HUANG K, et al. Minimally invasive transforaminal lumbar interbody fusion versus oblique lateral interbody fusion for lumbar degenerative disease: a meta-analysis. BMC Musculoskelet Disord. 2021;22(1):802. [6] OH BK, SON DW, LEE SH, et al. Learning Curve and Complications Experience of Oblique Lateral Interbody Fusion : A Single-Center 143 Consecutive Cases. J Korean Neurosurg Soc. 2021;64(3):447-459. [7] 侯坤鹏,赵泉来,吴天亮,等.斜外侧入路腰椎融合内固定的生物力学稳定性[J].中国组织工程研究,2021,25(33):5362-5368. [8] YUAN W, KALIYA-PERUMAL AK, CHOU SM, et al. Does Lumbar Interbody Cage Size Influence Subsidence? A Biomechanical Study. Spine (Phila Pa 1976). 2020;45(2):88-95. [9] BERECZKI F, TURBUCZ M, KISS R, et al. Stability Evaluation of Different Oblique Lumbar Interbody Fusion Constructs in Normal and Osteoporotic Condition - A Finite Element Based Study. Front Bioeng Biotechnol. 2021;9:749914. [10] 孙毅,梁彦超,武峰,等.成人腰椎软骨终板的组织学特征[J].脊柱外科杂志,2019,1(1):47-49. [11] PANJABI MM, OXLAND TR, YAMAMOTO I, et al. Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg Am. 1994; 76(3):413-424. [12] LU T, LU Y. Comparison of Biomechanical Performance Among Posterolateral Fusion and Transforaminal, Extreme, and Oblique Lumbar Interbody Fusion: A Finite Element Analysis. World Neurosurg. 2019;129:890-899. [13] LO CC, TSAI KJ, ZHONG ZC, et al. Biomechanical differences of Coflex-F and pedicle screw fixation combined with TLIF or ALIF--a finite element study. Comput Methods Biomech Biomed Engin. 2011;14(11):947-956. [14] POLIKEIT A, NOLTE LP, FERGUSON SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine (Phila Pa 1976). 2003;28(10): 991-996. [15] XIAO Z, WANG L, GONG H, et al. Biomechanical evaluation of three surgical scenarios of posterior lumbar interbody fusion by finite element analysis. Biomed Eng Online. 2012;11(1):1-11. [16] YAMAMOTO I, PANJABI MM, CRISCO JJ, et al. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine (Phila Pa 1976). 1989;14(11):1256-1260. [17] PIMENTA L, MARCHI L, OLIVEIRA L, et al. A prospective,randomized, controlled trial comparing radiographic and clinical outcomes between stand-alone lateral interbody lumbar fusion with either silicate calcium phosphate or rh-BMP2. Neurol Surg A Cent Eur Neurosurg. 2013;74: 343-350. [18] TEMPEL ZJ, GANDHOKE GS, OKONKWO DO, et al. Impaired bone mineral density as a predictor of graft subsidence following minimally invasive transpsoas lateral lumbar interbody fusion. Eur Spine J. 2015; 24 Suppl 3:414-419. [19] GE T, AO J, LI G, et al. Additional lateral plate fixation has no effect to prevent cage subsidence in oblique lumbar interbody fusion. J Orthop Surg Res. 2021;16(1):584. [20] AGARWAL N, FARAMAND A, ALAN N, et al. Lateral lumbar interbody fusion in the elderly: a 10-year experience: Presented at the 2018 AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves. J Neurosurg Spine. 2018;29(5):525-529. [21] HUO Y, YANG D, MA L, et al. Oblique Lumbar Interbody Fusion with Stand-Alone Cages for the Treatment of Degenerative Lumbar Spondylolisthesis: A Retrospective Study with 1-Year Follow-Up. Pain Res Manag. 2020;11:9016219. [22] ZHU G, HAO Y, YU L, et al. Comparing stand-alone oblique lumbar interbody fusion with posterior lumbar interbody fusion for revision of rostral adjacent segment disease: A STROBE-compliant study. Medicine (Baltimore). 2018;97(40):e12680. [23] ZHANG C, WANG K, JIAN F, et al. Efficacy of Oblique Lateral Interbody Fusion in Treatment of Degenerative Lumbar Disease. World neurosurg. 2018;S1878-8750(18)32698-6. [24] AHMADIAN A, BACH K, BOLINGER B, et al. Stand-alone minimally invasive laterallumbar interbody fusion: multicenter clinical outcomes. J Clin Neurosci. 2015;22(4):740-746. [25] ZENG Z, XU Z, HE D, et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. 2018;10(2): 98-106. [26] GUO HZ, TANG YC, GUO DQ, et al. Stability Evaluation of Oblique Lumbar Interbody Fusion Constructs with Various Fixation Options: A Finite Element Analysis Based on Three-Dimensional Scanning Models. World Neurosurg. 2020;138:e530-e538. [27] Wang B, Hua W, Ke W, et al. Biomechanical Evaluation of Transforaminal Lumbar Interbody Fusion and Oblique Lumbar Interbody Fusion on the Adjacent Segment: A Finite Element Analysis. World Neurosurg. 2019;126:e819-e824. [28] SONG C, CHANG H, ZHANG D, et al. Biomechanical Evaluation of Oblique Lumbar Interbody Fusion with Various Fixation Options: A Finite Element Analysis. Orthop Surg. 2021;13(2):517-529. [29] DU CF, CAI XY, GUI W, et al. Does oblique lumbar interbody fusion promote adjacent degeneration in degenerative disc disease: A finite element analysis. Comput Biol Med. 2021;128:104122. [30] LING Q, ZHANG H, HE E. Screws Fixation for Oblique Lateral Lumbar Interbody Fusion (OL-LIF): A Finite Element Study. Biomed Res Int. 2021;2021:5542595. [31] CHOY W, MAYER RR, MUMMANENI PV, et al. Oblique Lumbar Interbody Fusion With Stereotactic Navigation: Technical Note. Global Spine J. 2020;10(2 Suppl):94S-100S. [32] HAH R, KANG HP. Lateral and Oblique Lumbar Interbody Fusion-Current Concepts and a Review of Recent Literature. Curr Rev Musculoskelet Med. 2019;12(3):305-310. [33] TEMPEL ZJ, GANDHOKE GS, OKONKWO DO, et al. Impaired bone mineral density as a predictor of graft subsidence following minimally invasive transpsoas lateral lumbar interbody fusion. Eur Spine J. 2015; 24 Suppl 3:414-419. [34] WANG B, CHEN C, HUA W, et al. Minimally Invasive Surgery Oblique Lumbar Interbody Debridement and Fusion for the Treatment of Lumbar Spondylodiscitis. Orthop Surg. 2020;12(4):1120-1130. [35] WEN J, SHI C, YU L, et al. Unilateral Versus Bilateral Percutaneous Pedicle Screw Fixation in Oblique Lumbar Interbody Fusion. World Neurosurg. 2020;134:e920-e927. [36] HU Z, HE D, GAO J, et al. The Influence of Endplate Morphology on Cage Subsidence in Patients With Stand-Alone Oblique Lateral Lumbar Interbody Fusion (OLIF). Global Spine J. 2021;9:2192568221992098. [37] LIU J, DING W, YANG D, et al. Modic Changes (MCs) Associated with Endplate Sclerosis Can Prevent Cage Subsidence in Oblique Lumbar Interbody Fusion (OLIF) Stand-Alone. World Neurosurg. 2020;138: e160-e168. |
| [1] | Peng Zhixin, Yan Wengang, Wang Kun, Zhang Zhenjiang. Finite element analysis and structural optimization design of 3D printed forearm braces [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1340-1345. |
| [2] | Liu Jinyu, Zhang Hanshuo, Cui Hongpeng, Pan Lingzhi, Zhao Boran, Li Fei, Ding Yu. Finite element biomechanical analysis of minimally invasive treatment of cervical spondylotic myelopathy and accurate exercise rehabilitation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1359-1364. |
| [3] | He Yujie, Kang Zhijie, Xue Mingming, Jin Feng, Li Zhijun, Wang Xing, Xu Yangyang, Gao Mingjie, Li Jiawei, Li Xiaohe, Wang Haiyan. Finite element analysis of transarticular screw fixation of adolescent thoracic vertebra [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1365-1370. |
| [4] | Wen Xinghua, Ding Huanwen, Cheng Kai, Yan Xiaonan, Peng Yuanhao, Wang Yuning, Liu Kang, Zhang Huiwu. Three-dimensional finite element model analysis of intramedullary nailing fixation design for large femoral defects in Beagle dogs [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1371-1376. |
| [5] | Liu Qinghua, Cai Yongqiang, Jin Feng, Yu Jinghong, Wang Haiyan, Zhang Yunfeng, Wang Lidong, Li Jiawei, Wang Xing, He Yujie, Dai Lina, Wang Jianzhong, Wu Chao, Tong Ling, Kang Zhijie, Li Zhijun, Li Xiaohe. Finite element model of the 12-year-old child whole cervical spine: establishment and validity verification based on CT data [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 500-504. |
| [6] | Liu Hao, Yang Hongsheng, Zeng Zhimou, Wang Liping, Yang Kunhai, Hu Yongrong, Qu Bo. Lumbar MRI vertebral bone quality score to evaluate the severity of osteoporosis in postmenopausal women [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 606-611. |
| [7] | Lu Hui, Wu Qimei, Liu Rong. Finite element analysis and application of unilateral and bilateral bone-filling mesh container in treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 391-397. |
| [8] | Wei Guoqiang, Li Yunfeng, Wang Yi, Niu Xiaofen, Che Lifang, Wang Haiyan, Li Zhijun, Shi Guopeng, Bai Ling, Mo Kai, Zhang Chenchen, Xu Yangyang, Li Xiaohe. Biomechanical analysis of non-uniform material femur under different loads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1318-1322. |
| [9] | Lü Qianyi, Chen Xinyi, Zheng Huie, He Haolong, Li Qilong, Chen Chutao, Tian Haomei. Stress and displacement of normal lumbar vertebra and posterior structure with different elbow pressing methods [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1346-1350. |
| [10] | Zhang Yufang, Lü Meng, Mei Zhao. Construction and verification of a full spine biomechanical model of adolescent scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1351-1356. |
| [11] | Zhang Jichao, Dong Yuefu, Mou Zhifang, Zhang Zhen, Li Bingyan, Xu Xiangjun, Li Jiayi, Ren Meng, Dong Wanpeng. Finite element analysis of biomechanical changes in the osteoarthritis knee joint in different gait flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1357-1361. |
| [12] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [13] | Li Guijun, Fang Xiaohui, Kong Weifeng, Yuan Xiaoqing, Jin Rongzhong, Yang Jun. Finite element analysis of the treatment of hallux valgus deformity by microplate combined with super strong suture elastic fixation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 938-942. |
| [14] | Wen Mingtao, Liang Xuezhen, Li Jiacheng, Xu Bo, Li Gang. Mechanical stability of Sanders II type calcaneal fractures fixed by two internal fixation methods [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 838-842. |
| [15] | Wang Hailong, Li Long, Maihemuti·Yakufu, Chen Hongtao, Liu Xu, Yilihamu·Tuoheti. Finite element analysis of stress distribution of acetabular prosthesis in the Lewinnek safety zone [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 843-847. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||