[1] 中国抗癌协会血液肿瘤专业委员会,中华医学会血液学分会白血病淋巴瘤学组,中国临床肿瘤学会抗淋巴瘤联盟.造血干细胞移植治疗淋巴瘤中国专家共识(2018年版)[J].中华肿瘤杂志, 2018,40(12):927-934.
[2] ZENG H, CHEN W, ZHENG R, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6(5):e555-e567.
[3] AL-MANSOUR Z, LI H, COOK JR, et al. Autologous transplantation as consolidation for high risk aggressive T-cell non-Hodgkin lymphoma: a SWOG 9704 intergroup trial subgroup analysis. Leuk Lymphoma. 2019;60(8):1934-1941.
[4] HAMADANI M, HARI PN, ZHANG Y, et al. Early failure of frontline rituximab-containing chemo-immunotherapy in diffuse large B cell lymphoma does not predict futility of autologous hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2014;20(11): 1729-1736.
[5] MOHTY M, HÜBEL K, KRÖGER N, et al. Autologous haematopoietic stem cell mobilisation in multiple myeloma and lymphoma patients: a position statement from the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 2014;49(7):865-872.
[6] GIRALT S, COSTA L, SCHRIBER J, et al. Optimizing autologous stem cell mobilization strategies to improve patient outcomes: consensus guidelines and recommendations. Biol Blood Marrow Transplant. 2014;20(3):295-308.
[7] YOON JH, KIM JW, JEON YW, et al. Role of frontline autologous stem cell transplantation in young, high-risk diffuse large B-cell lymphoma patients. Korean J Intern Med. 2015;30(3):362-371.
[8] HERMINE O, HOSTER E, WALEWSKI J, et al. Addition of high-dose cytarabine to immunochemotherapy before autologous stem-cell transplantation in patients aged 65 years or younger with mantle cell lymphoma (MCL Younger): a randomised, open-label, phase 3 trial of the European Mantle Cell Lymphoma Network. Lancet. 2016; 388(10044):565-575.
[9] GERSON JN, HANDORF E, VILLA D, et al. Survival Outcomes of Younger Patients With Mantle Cell Lymphoma Treated in the Rituximab Era. J Clin Oncol. 2019;37(6):471-480.
[10] METZNER B, POTT C, MÜLLER TH, et al. Long-term clinical and molecular remissions in patients with follicular lymphoma following high-dose therapy and autologous stem cell transplantation. Ann Oncol. 2013;24(6):1609-1615.
[11] BATCHELOR T, LOEFFLER JS. Primary CNS lymphoma. J Clin Oncol. 2006; 24(8):1281-1288.
[12] YOKOTA H, MIYAO K, OHARA F, et al. Exploring the Safety and Efficacy of Upfront Autologous Stem Cell Transplantation with LEED Preconditioning for Primary Central Nervous System Lymphoma. Blood. 2019;134(Supplement_1):1611.
[13] LIU S , JIN Z , WU D , et al. Outcome of Autologous Hematopoietic Cell Transplantation in First Complete Remission(CR1) in Patients with Peripheral T-Cell Lymphomas(PTCLs). Blood. 2019;134(Supplement_1): 3315.
[14] JOHNSTON C, HARRINGTON R, JAIN R, et al. Safety and Efficacy of Combination Antiretroviral Therapy in Human Immunodeficiency Virus-Infected Adults Undergoing Autologous or Allogeneic Hematopoietic Cell Transplantation for Hematologic Malignancies. Biol Blood Marrow Transplant. 2016;22(1):149-156.
[15] STIFF PJ, UNGER JM, COOK JR, et al. Autologous transplantation as consolidation for aggressive non-Hodgkin’s lymphoma. N Engl J Med. 2013;369(18):1681-1690.
[16] REDDY NM, OLUWOLE O, GREER JP, et al. Outcomes of autologous or allogeneic stem cell transplantation for non-Hodgkin lymphoma. Exp Hematol. 2014;42(1):39-45.
[17] ASSOULINE S, LI S, GISSELBRECHT C, et al. The conditional survival analysis of relapsed DLBCL after autologous transplant: a subgroup analysis of LY.12 and CORAL. Blood Adv. 2020;4(9):2011-2017.
[18] 马军,石远凯,朱军,等.西达本胺治疗外周 T 细胞淋巴瘤中国专家共识 (2016 版)[J]. 中国肿瘤临床,2016,43(8):317-323.
[19] AYALA E. Hematopoietic cell transplantation for B-cell lymphoma: an update. Cancer Control. 2012;19(3):175-186.
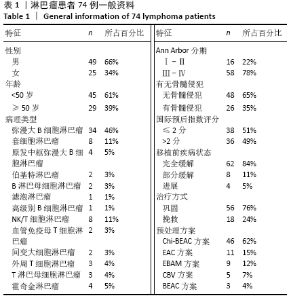
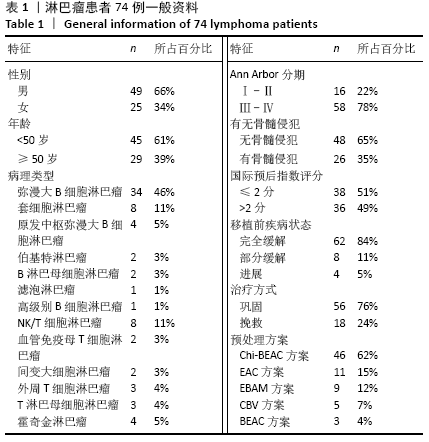
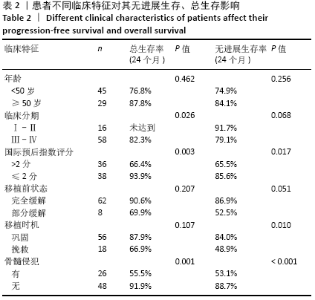
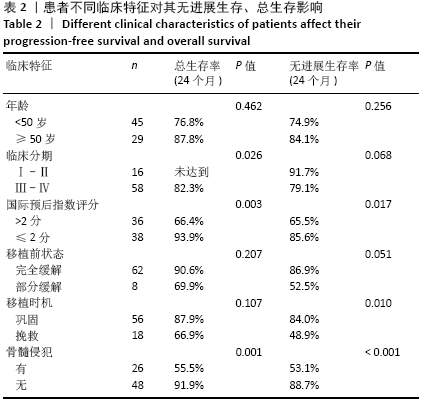
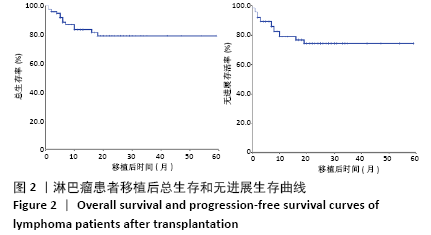
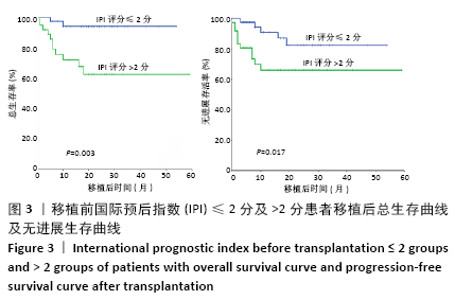
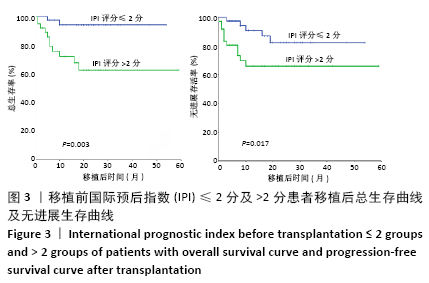
[20] 姜丽,朱尊民.影响高危难治淋巴瘤患者自体外周血造血干细胞移植治疗后生存和预后的相关因素分析[J].中国实验血液学杂志, 2018,26(3):784-788. |