[1] 蒋文杰.先天性小耳畸形的治疗进展[J].中国现代医药杂志,2009, 11(2):125-127.
[2] 庄洪兴,蒋海越,潘博,等.先天性小耳畸形的皮肤软组织扩张器法外耳再造术[J].中华整形外科杂志,2006,22(4):286-289.
[3] 李高峰,谭军,罗滔,等. 耳后延迟皮瓣白体肋软骨支架法外耳再造术[J].中华医学美学美容杂志,2014,20(4):241-243.
[4] LI G, ZHANG F, DING W, et al. A New Microtia Reconstruction Method Using Delayed Postauricular Skin Flap. Plast Reconstr Surg. 2017; 139(4):946-955.
[5] NAGATA S. Modification of the stages in total reconstruction of the auricle: Part I. Grafting the three-dimensional costal cartilage framework for lobule-type microtia. Plast Reconstr Surg. 1994; 93(2):221-230.
[6] BRENT B. Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstr Surg. 1992; 90(3):355-374.
[7] BRENT B. Microtia repair with rib cartilage grafts: a review of personal experience with 1000 cases. Clin Plast Surg. 2002;29(2):257-271.
[8] NAGATA S. A new method of total reconstruction of the auricle for microtia. Plast Reconstr Surg. 1993;92(2):187-201.
[9] 张帆,李高峰.耳廓再造术的发展历程[J].中国美容医学,2016, 25(5):102-104.
[10] 吴琍,任纪祯,陈振雨,等.高压氧对大鼠超长随意皮瓣成活率的影响[J].中华航海医学与高气压医学杂志, 2008, 15(5):279-282.
[11] 焦向阳,郭恩覃.真皮下血管网皮瓣血供重建的实验研究[J].中华整形外科杂志, 1992, 8(3):213-215.
[12] 张强,邵家松,岳毅刚,等.高压氧对兔耳创面模型早期瘢痕组织形成的影响[J].中华整形外科杂志,2013,29(1):55-58.
[13] ALTINEL D, SERIN M, ERDEM H, et al. Comparison of incisional delay patterns on a rat random flap model. J Plast Surg Hand Surg. 2019; 53(4):247-253.
[14] JIANG Z, LI X, CHEN M, et al. Effect of Endogenous Vascular Endothelial Growth Factor on Flap Surgical Delay in a Rat Flap Model. Plast Reconstr Surg. 2019;143(1):126-135.
[15] 朱江英,殷国前.高压氧预处理超长皮瓣组织血管内皮生长因子、转化生长因子β的表达[J].中国组织工程研究,2016,20(11):1525-1531.
[16] RICHARDS L, LINEAWEAVER WC, STILE F, et al. Effect of hyperbaric oxygen therapy on the tubed pedicle flap survival in a rat model. Ann Plast Surg. 2003;50(1):51-56.
[17] 戚征,高春锦.高压氧预处理促进皮瓣成活的研究[J].中华医学美学美容杂志,2009,15(1):46-48.
[18] BAYNOSA RC, ZAMBONI WA. The effect of hyperbaric oxygen on compromised grafts and flaps. Undersea Hyperb Med. 2012;39(4):857-865.
[19] PHILLIPS JC. Understanding hyperbaric oxygen therapy and its use in the treatment of compromised skin grafts and flaps. Plast Surg Nurs. 2005;25(2):72-80.
[20] HONG JP, KWON H, CHUNG YK, et al. The effect of hyperbaric oxygen on ischemia-reperfusion injury: an experimental study in a rat musculocutaneous flap. Ann Plast Surg. 2003;51(5):478-487.
[21] HUNT TK, PAI MP. The effect of varying ambient oxygen tensions on wound metabolism and collagen synthesis. Surg Gynecol Obstet. 1972;135(4):561-567.
[22] CLARK RA. Fibrin glue for wound repair: facts and fancy. Thromb Haemost. 2003;90(6):1003-1006.
[23] JANIS JE, KWON RK, LALONDE DH. A practical guide to wound healing. Plast Reconstr Surg. 2010;125(6):230e-244e.
[24] 王炜.整形外科学[M].杭州:浙江科学技术出版社, 1999: 144.
[25] GHALI S, BUTLER PE, TEPPER OM, et al. Vascular delay revisited. Plast Reconstr Surg. 2007;119(6):1735-1744.
[26] CARROLL CM, CARROLL SM, SCHUSCHKE DA, et al. Augmentation of skeletal muscle flap survival using platelet derived growth factor. Plast Reconstr Surg. 1998;102(2):407-415.
[27] AUSPRUNK DH, FOLKMAN J. Migration and proliferation of endothelial cells in preformed and newly formed blood vessels during tumor angiogenesis. Microvasc Res. 1977;14(1):53-65.
[28] MORRIS SF, TAYLOR GI. The time sequence of the delay phenomenon: when is a surgical delay effective? An experimental study. Plast Reconstr Surg. 1995;95(3):526-533.
[29] 胡长青.延迟皮瓣的临床应用及动物实验研究[D]. 苏州:苏州大学, 2017.
[30] LI X, CHEN M, JIANG Z, et al. Visualized identification of the maximal surgical delay effect in a rat flap model. Wound Repair Regen. 2019; 27(1):39-48.
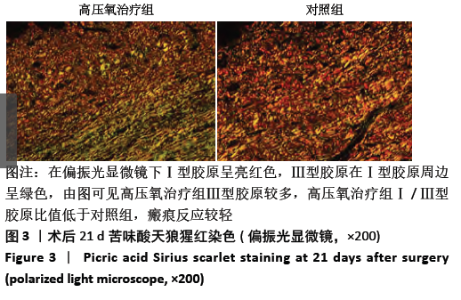
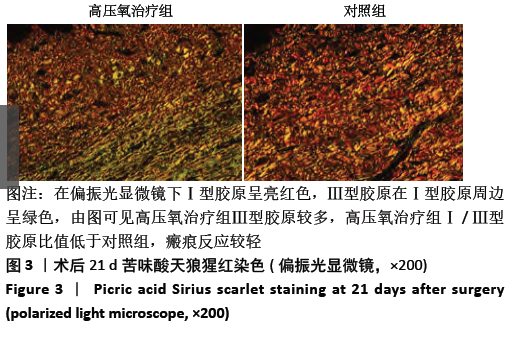
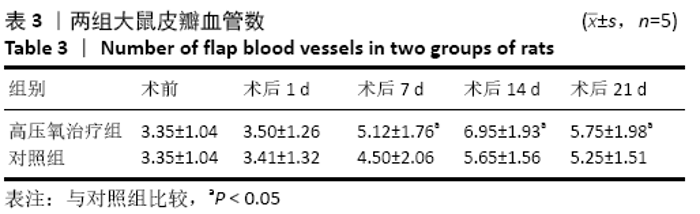
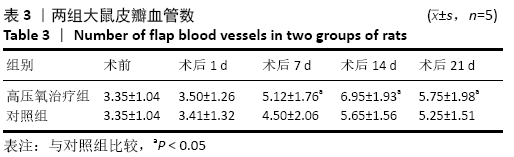
|